Trip photos
I found inspiration in India
Here are a few pictures from my latest visit to this amazing country.

Around this time last year, I wrote a Gates Notes post that began: “I just returned from my visit to India, and I can’t wait to go back again.”
Last week, I got my wish and returned to India—and now that I’m home, I can’t wait to go back for another visit.
My goal was to get an update on some of the world-changing ideas and inventions that are coming out of India, and that’s exactly what I got. I spent four days there, meeting with political leaders, government officials, scientists, philanthropists, women who are lifting their communities out of poverty, and many others. The Gates Foundation funds more work in India than in any other country (other than the United States), and it’s always uplifting and educational to be there in person and see the impact of the efforts we’re supporting. Here are a few photos from my visit.
The doctor can see you now
Expanding access to health care through AI
Today’s AI can transform health care systems and support health care workers the world over.

A core principle underlying the Gates Foundation’s work is closing the innovation gap between rich countries and everyone else. People in poorer parts of the world shouldn’t have to wait decades for new technologies to reach them. That’s why we've worked for 25 years to accelerate access to life-saving medicines and vaccines in low- and middle-income countries.
It's also why, today, the Gates Foundation and OpenAI are announcing an initiative called Horizon1000 to support several countries in Africa, starting in Rwanda, as they apply AI technology to improve their health care systems.
Over the next few years, we will collaborate with leaders in African countries as they pioneer the deployment of AI in health. Together, the Gates Foundation and OpenAI are committing $50 million in funding, technology, and technical support to back their work. The goal is to reach 1,000 primary healthcare clinics and their surrounding communities by 2028.
Today’s AI can help save lives
A few years ago, I wrote that the rise of artificial intelligence would mark a technological revolution as far-reaching for humanity as microprocessors, PCs, mobile phones, and the Internet. Everything I’ve seen since then confirms my view that we are on the cusp of a breathtaking global transformation.
All over the world, AI, in the form of LLMs and machine learning models, are improving far more quickly than I first anticipated. From science to education to customer service and more, AI tools are reshaping every facet of our lives.
I spend a lot of time thinking about how AI can help us address fundamental challenges like poverty, hunger, and disease. One issue that I keep coming back to is making great health care accessible to all—and that’s why we’re partnering with OpenAI and African leaders and innovators on Horizon1000.
Not enough doctors in the house
We have seen amazing successes in global health over the past 25 years: child mortality has been cut in half, and there are now real pathways to eliminating or controlling deadly diseases like polio, malaria, TB, and HIV. But one stubborn problem that keeps slowing progress is the desperate shortage of health care workers in poorer parts of the world.
In Sub-Saharan Africa, which suffers from the world’s highest child mortality rate, there is a shortfall of nearly 6 million health care workers, a gap so large that even the most aggressive hiring and training efforts can’t close it in the foreseeable future.
These huge shortages put health care workers in these countries in an impossible situation. They’re forced to triage too many patients with too little administrative support, modern technology, and up-to-date clinical guidance. Partly as a result, the WHO estimates that low-quality care is a contributing factor in 6 to 8 million deaths in low- and middle-income countries every year, and that’s not even counting the millions who die because they aren’t able to access health care at all.
Rwanda leads the way
Today’s AI can help save those lives by reaching many more people with much higher-quality care.
Rwanda currently has only one health care worker per 1,000 people, far below the WHO recommendation of about four per 1,000. It would take 180 years for that gap to close at the current pace of progress. So, as part of the 4x4 reform initiative, Minister of Health Dr. Sabin Nsanzimana recently announced the launch of an AI-powered Health Intelligence Center in Kigali to help ensure limited health care resources are being used as wisely as possible.
As part of the Horizon1000 initiative, we aim to accelerate the adoption of AI tools across primary care clinics, within communities, and in people’s homes. These AI tools will support health workers, not replace them.
On the horizon
Minister Nsanzimana has called AI the third major discovery to transform medicine, after vaccines and antibiotics, and I agree with his point of view.
If you live in a wealthier country and have seen a doctor recently, you may have already seen how AI is making life easier for health care workers. Instead of taking notes constantly, they can now spend more time talking directly to you about your health, while AI transcribes and summarizes the visit. Afterwards, AI can handle much of the onerous paperwork, so doctors and nurses can focus on the next patient.
In poorer countries with enormous health worker shortages and lack of health systems infrastructure, AI can be a gamechanger in expanding access to quality care. I believe this partnership with OpenAI, governments, innovators, and health workers in sub-Saharan Africa is a step towards the type of AI we need more of: systems that help people all over the world to solve generational challenges that they simply didn’t know how to address before. I invite others working on AI to think about how we can put these massively powerful tools to the best use.
This announcement is a great example of why I remain optimistic about the improvements we can make. I’m looking forward to seeing health workers using some of these AI solutions in action when I visit Africa, and I plan to continue focusing on ways AI technology can help billions of people in low- and middle-income countries meet their most important needs.
The Year Ahead
Optimism with footnotes
As we start 2026, I am thinking about how the year ahead will set us up for the decades to come.

I have always been an optimist. When I founded Microsoft, I believed a digital revolution powered by great software would make the world a better place. When I started the Gates Foundation, I saw an opportunity to save and improve millions of lives because critical areas like children’s health were getting so little money.
In both cases, the results exceeded my expectations. We are far better off than when I was born 70 years ago. I believe the world will keep improving—but it is harder to see that today than it has been in a long time.
Friends and colleagues often ask me how I stay optimistic in an era with so many challenges and so much polarization. My answer is this: I am still an optimist because I see what innovation accelerated by artificial intelligence will bring. But these days, my optimism comes with footnotes.
The thing I am most upset about is the fact that the world went backwards last year on a key metric of progress: the number of deaths of children under 5 years old. Over the last 25 years, those deaths went down faster than at any other point in history. But in 2025, they went up for the first time this century, from 4.6 million in 2024 to 4.8 million in 2025—an increase driven by less support from rich countries to poor countries. This trend will continue unless we make progress in restoring aid budgets.
The next five years will be difficult as we try to get back on track and work to scale up new lifesaving tools. Yet I remain optimistic about the long-term future. As hard as last year was, I don’t believe we will slide back into the Dark Ages. I believe that, within the next decade, we will not only get the world back on track but enter a new era of unprecedented progress.
The key will be, as always, innovation. Consider this: An HIV diagnosis used to be a death sentence. Today, thanks to revolutionary treatments, a person with HIV can expect to live almost as long as someone without the virus. By the 2040s, new innovations could virtually eliminate deaths from HIV/AIDS.
Budget cuts limit how many people benefit from lifesaving tools, as we saw to devastating effect last year. But nothing can erase the fact that for decades we didn’t know how to save people from HIV, and now we do. Breakthroughs are a bell that cannot be unrung. They ensure that we will never go back to the world in 2000 where over 10 million children died from preventable causes every year—and they form the core of my optimism about where the world is headed.
But as I mentioned, there are footnotes to my optimism. Although the innovation pipeline sets us up for long-term success, the trajectory of progress hinges on how the world addresses three key questions.
1.
Will a world that is getting richer increase its generosity toward those in need?
The “golden rule” precept is more important now than ever with the record disparities in wealth. This idea of treating others as you wish to be treated does not just apply to rich countries giving aid. It must also include philanthropy from the wealthy to help those in need—both domestically and globally—which should grow rapidly in a world with a record number of billionaires and even centibillionaires.
Through the Giving Pledge, I get to work with a number of incredible philanthropists who set a great example by giving away substantial portions of their wealth in smart ways. However, more needs to be done to encourage higher levels of generosity from the rich and to show how fulfilling and impactful it can be.
Turning to aid budgets for poor countries, I am worried about one number: If funding for health decreases by 20 percent, 12 million more children could die by 2045. I know cuts won’t be reversed overnight, even though aid represented less than 1 percent of GDP even in the most generous countries. But it is critical that we restore some of the funding. The foundation’s Goalkeepers report lays out what is at risk and how the world can best spend the aid it gives.
I will spend much of my year working with partners to advocate for increased funding for the health of the world’s children. I plan to engage with a number of communities, including health care workers, religious groups, and members of diaspora communities to help make this case.
2.
Will the world prioritize scaling innovations that improve equality?
Some problems require doing far more than just letting market incentives take their course.
The first critical area is climate change. Without a large global carbon tax (which is, unfortunately, politically unachievable), market forces do not properly incentivize the creation of technologies to reduce climate-related emissions.
Yet only by replacing all emitting activities with cheaper alternatives will we stop the temperature increase. This is why I started Breakthrough Energy 10 years ago and why I will continue to put billions into innovation.
The world has made meaningful progress in the last decade, cutting projected emissions by more than 40 percent. But we still have a lot of innovation and scaling up to do in tough areas like industrial emissions and aviation. Government policies in rich countries are still critical because unless innovations reach scale, the costs won’t come down and we won’t achieve the impact we need.
If we don’t limit climate change, it will join poverty and infectious disease in causing enormous suffering, especially for the world’s poorest people. Since even in the best case the temperature will continue to go up, we also need to innovate to minimize the negative impacts.
This is called climate adaptation, and a critical example is helping farmers in poor countries with better seeds and better advice so they can grow more even in the face of climate change. Using AI, we will soon be able to provide poor farmers with better advice about weather, prices, crop diseases, and soil than even the richest farmers get today. The foundation has committed $1.4 billion to supporting farmers on the frontlines of extreme weather.
I will be investing and giving more than ever to climate work in the years ahead while also continuing to give more to children’s health, the foundation’s top priority. The need to ensure money is spent on the most important priorities was the topic of a memo I wrote in the fall.
A second critical area where the world must focus on innovation-driven equality is health care. Concerns about healthcare costs and quality are higher than ever in all countries.
In theory, people should feel optimistic about the state of health care with the incredible pipeline of innovations. For example, a recent breakthrough in diagnosing Alzheimer’s will revolutionize how we test for—and ultimately prevent—this disease, saving billions of dollars in costs. (Funding Alzheimer’s research is a particular focus for me.) There’s similar progress on obesity and cancer, as well as on problems in developing countries like malaria, TB, and malnutrition.
Despite so much progress, however, the cost and complexity of the system means very few people are satisfied with their care. I believe we can improve health care dramatically in all countries by using AI not only to accelerate the development of innovations but directly in the delivery of health care.
Like many of you, I already use AI to better understand my own health. Just imagine what will be possible as it improves and becomes available for every patient and provider. Always-available, high-quality medical advice will improve medicine by every measure.
We aren’t quite there yet—developers still have work to do on reliability and how we connect the AI to doctors and nurses so they are empowered to check and override the system. But I’m optimistic we will soon begin to scale access globally. I am following this work so the Gates Foundation and partners can make sure this capability is available in the countries that need it most—where there aren’t enough medical personnel—at the same time it is available elsewhere. We are already working on pilots and making sure that even relatively uncommon African languages are fully supported.
Governments will have to play a central role in leading the implementation of AI into their health systems. This is another case where the market alone won’t and can’t provide the solution.
A third and final area I will mention briefly is education. AI gives us a chance for the kind of personalized learning to keep students motivated that we have dreamed of in the past. This is now a focus of the Gates Foundation’s spending on education, and I am hopeful it will be empowering to both teachers and students. I’ve seen this firsthand in New Jersey, and it will be game changing as we scale it for the world.
All three of these areas—climate, health, and education—can improve rapidly with the right government focus. This year I will spend a lot of time meeting with pioneers all over the world to see which countries are doing the best work so we can spread best practices.
3.
Will we minimize negative disruptions caused by AI as it accelerates?
Of all the things humans have ever created, AI will change society the most. It will help solve many of our current problems while also bringing new challenges very different from past innovations.
When people in the AI space predict that AGI or fully humanoid robots will come soon and then those deadlines are missed, it creates the impression that these things will never happen. However, there is no upper limit on how intelligent AIs will get or on how good robots will get, and I believe the advances will not plateau before exceeding human levels.
The two big challenges in the next decade are use of AI by bad actors and disruption to the job market. Both are real risks that we need to do a better job managing. We’ll need to be deliberate about how this technology is developed, governed, and deployed.
In 2015, I gave a TED talk warning that the world was not ready to handle a pandemic. If we had prepared properly for the Covid pandemic, the amount of human suffering would have been dramatically less. Today, an even greater risk than a naturally caused pandemic is that a non-government group will use open source AI tools to design a bioterrorism weapon.
The second challenge is job market disruption. AI capabilities will allow us to make far more goods and services with less labor. In a mathematical sense, we should be able to allocate these new capabilities in ways that benefit everyone. As AI delivers on its potential, we could reduce the work week or even decide there are some areas we don’t want to use AI in.
The effects of this disruption are hard to model. Sometimes, when a game-changing technology improves rapidly, it drives more demand at lower cost and, by making the world richer, increases demand in other areas. For example, AI makes software developers at least twice as efficient, which makes coding cheaper while also creating demand elasticity for code. (Computing is a good historical example where lower costs actually caused the overall market to grow.)
Even with this complexity, the rate of improvement is already starting to be enough to disrupt job demand in areas like software development. Other areas like warehouse work or phone support are not quite there yet, but once the AIs become more capable, the job disruption will be more immediate.
We’re already starting to see the impact of AI on the job market, and I think this impact will grow over the next five years. Even if the transition takes longer than I expect, we should use 2026 to prepare ourselves for these changes—including which policies will best help spread the wealth and deal with the important role jobs play in our society. Different political parties will likely suggest different approaches.
By including these footnotes, particularly the last one, some readers may find my continued optimism even more surprising. But as we start 2026, I remain optimistic about the days ahead because of two core human capabilities.
The first is our ability to anticipate problems and prepare for them, and therefore ensure that our new discoveries make all of us better off. The second is our capacity to care about each other. Throughout history, you can always find stories of people tending not just to themselves or their clan or their country but to the greater good.
Those two qualities—foresight and care—are what give me hope as the year begins. As long as we keep exercising those abilities, I believe the years ahead can be ones of real progress.
A new way to look at the problem
Three tough truths about climate
What I want everyone at COP30 to know.

There’s a doomsday view of climate change that goes like this:
In a few decades, cataclysmic climate change will decimate civilization. The evidence is all around us—just look at all the heat waves and storms caused by rising global temperatures. Nothing matters more than limiting the rise in temperature.
Fortunately for all of us, this view is wrong. Although climate change will have serious consequences—particularly for people in the poorest countries—it will not lead to humanity’s demise. People will be able to live and thrive in most places on Earth for the foreseeable future. Emissions projections have gone down, and with the right policies and investments, innovation will allow us to drive emissions down much further.
Unfortunately, the doomsday outlook is causing much of the climate community to focus too much on near-term emissions goals, and it’s diverting resources from the most effective things we should be doing to improve life in a warming world.
It’s not too late to adopt a different view and adjust our strategies for dealing with climate change. Next month’s global climate summit in Brazil, known as COP30, is an excellent place to begin, especially because the summit’s Brazilian leadership is putting climate adaptation and human development high on the agenda.
This is a chance to refocus on the metric that should count even more than emissions and temperature change: improving lives. Our chief goal should be to prevent suffering, particularly for those in the toughest conditions who live in the world’s poorest countries.
Although climate change will hurt poor people more than anyone else, for the vast majority of them it will not be the only or even the biggest threat to their lives and welfare. The biggest problems are poverty and disease, just as they always have been. Understanding this will let us focus our limited resources on interventions that will have the greatest impact for the most vulnerable people.
I know that some climate advocates will disagree with me, call me a hypocrite because of my own carbon footprint (which I fully offset with legitimate carbon credits), or see this as a sneaky way of arguing that we shouldn’t take climate change seriously.
To be clear: Climate change is a very important problem. It needs to be solved, along with other problems like malaria and malnutrition. Every tenth of a degree of heating that we prevent is hugely beneficial because a stable climate makes it easier to improve people’s lives.
I’ve been learning about warming—and investing billions in innovations to reduce it—for over 20 years. I work with scientists and innovators who are committed to preventing a climate disaster and making cheap, reliable clean energy available to everyone. Ten years ago, some of them joined me in creating Breakthrough Energy, an investment platform whose sole purpose is to accelerate clean energy innovation and deployment. We’ve supported more than 150 companies so far, many of which have blossomed into major businesses. We’re helping build a growing ecosystem of thousands of innovators working on every aspect of the problem.
My views on climate change are also informed by my work at the Gates Foundation over the past 25 years. The foundation’s top priority is health and development in poor countries, and we approach climate largely through that lens. This has led us to fund a lot of climate-smart innovations, especially in agriculture, in places where extreme weather is taking the worst toll.
COP30 is taking place at a time when it’s especially important to get the most value out of every dollar spent on helping the poorest. The pool of money available to help them—which was already less than 1 percent of rich countries’ budgets at its highest level—is shrinking as rich countries cut their aid budgets and low-income countries are burdened by debt. Even proven efforts like providing lifesaving vaccines for all the world’s children are not being fully funded. Gavi (the vaccine-buying fund) will have 25 percent less money for the next five years compared to the past five years. We have to think rigorously and numerically about how to put the time and money we do have to the best use.
So I urge everyone at COP30 to ask: How do we make sure aid spending is delivering the greatest possible impact for the most vulnerable people? Is the money designated for climate being spent on the right things?
I believe the answer is no.
Sometimes the world acts as if any effort to fight climate change is as worthwhile as any other. As a result, less-effective projects are diverting money and attention from efforts that will have more impact on the human condition: namely, making it affordable to eliminate all greenhouse gas emissions and reducing extreme poverty with improvements in agriculture and health.
In short, climate change, disease, and poverty are all major problems. We should deal with them in proportion to the suffering they cause. And we should use data to maximize the impact of every action we take.
I believe that embracing the following three truths will help us do that.
Even if the world takes only moderate action to curb climate change, the current consensus is that by 2100 the Earth’s average temperature will probably be between 2°C and 3°C higher than it was in 1850.
That’s well above the 1.5°C goal that countries committed to at the Paris COP in 2015. In fact, between now and 2040, we are going to fall far short of the world’s climate goals. One reason is that the world’s demand for energy is going up—more than doubling by 2050.
From the standpoint of improving lives, using more energy is a good thing, because it’s so closely correlated with economic growth. This chart shows countries’ energy use and their income. More energy use is a key part of prosperity.
Unfortunately, in this case, what’s good for prosperity is bad for the environment. Although wind and solar have gotten cheaper and better, we don’t yet have all the tools we need to meet the growing demand for energy without increasing carbon emissions.
But we will have the tools we need if we focus on innovation. With the right investments and policies in place, over the next ten years we will have new affordable zero-carbon technologies ready to roll out at scale. Add in the impact of the tools we already have, and by the middle of this century emissions will be lower and the gap between poor countries and rich countries will be greatly reduced.
I wasn’t sure this would be possible when Breakthrough Energy was started in 2015 after the Paris agreement. Since then, the progress of Breakthrough companies and others and the acceleration now being provided by the use of artificial intelligence have made me confident that these advances will be ready to scale.
All countries will be able to construct buildings with low-carbon cement and steel. Almost all new cars will be electric. Farms will be more productive and less destructive, using fertilizer created without generating any emissions. Power grids will deliver clean electricity reliably, and energy costs will go down.
Even with these innovations, though, the cumulative emissions will cause warming and many people will be affected. We’ll see what you might call latitude creep: In North America, for instance, Iowa will start to feel more like Texas. Texas will start to feel more like northern Mexico. Although there will be climate migration, most people in countries near the equator won’t be able to relocate—they will experience more heat waves, stronger storms, and bigger fires. Some outdoor work will need to pause during the hottest hours of the day, and governments will have to invest in cooling centers and better early warning systems for extreme heat and weather events.
Every time governments rebuild, whether it’s homes in Los Angeles or highways in Delhi, they’ll have to build smarter: fire-resistant materials, rooftop sprinklers, better land management to keep flames from spreading, and infrastructure designed to withstand harsh winds and heavy rainfall. It won’t be cheap, but it will be possible in most cases. Unfortunately, this capacity to adapt is not evenly distributed, a subject I will return to below.
So why am I optimistic that innovation will curb climate change? For one thing, because it already has.
You probably know about improvements like better electric vehicles, dramatically cheaper solar and wind power, and batteries to store electricity from renewables. What you may not be aware of is the large impact these advances are having on emissions.
Ten years ago, the International Energy Agency predicted that by 2040, the world would be emitting 50 billion tons of carbon dioxide every year. Now, just a decade later, the IEA’s forecast has dropped to 30 billion, and it’s projecting that 2050 emissions will be even lower.
Read that again: In the past 10 years, we’ve cut projected emissions by more than 40 percent.
This progress is not part of the prevailing view of climate change, but it should be. What made it possible is that the Green Premium—the cost difference between clean and dirty ways of doing something—reached zero or became negative for solar, wind, power storage, and electric vehicles. By and large, they are just as cheap as, or even cheaper than, their fossil fuel counterparts.
Of course, to get to net zero, we need more breakthroughs. This will become even more important if new evidence shows that climate change will be much worse than what the current generation of climate models predicts, because we will need to lower the Green Premium faster and accelerate the transition to a zero-emission economy.
Luckily, humans’ ability to invent is better than it has ever been.
Breakthrough Energy focuses its new investment on the areas of innovation that still have large positive Green Premiums. Below I write about the state of play in the five sectors of the economy that are responsible for all carbon emissions. I’ll cover highlights and challenges—one common theme will be the difficulty of scaling rapidly—and I’ll include some of the companies Breakthrough Energy works with so you can see how much activity there is in each sector.
Electricity (28 percent of global emissions)
Making electricity is the second biggest source of emissions, but it’s arguably the most important: To decarbonize the other sectors, we’ll have to electrify a lot of things that currently use fossil fuels. We need more innovation in renewables, transmission, and other ways to generate and store electricity.
- New approaches to wind power can generate more energy using less land, and advances in geothermal mean it’s being tapped in more places around the world. (Examples: Fervo, Baseload Capital, Airloom)
- Companies are pilot-testing highly efficient power lines that can transmit much more electricity than the previous generation of cables. (TS Conductor, VEIR)
- We need to keep reducing the cost of clean energy that’s available around the clock, including new nuclear fission and fusion facilities. More than half of today’s emissions from electricity could only be eliminated using these so-called “firm” sources, but they have a Green Premium of well over 50 percent. I’m hopeful that we can get rid of the Green Premium with fission; a next-generation nuclear power plant is under construction in Wyoming. And fusion, which promises to give us an inexhaustible supply of cheap clean electricity, has moved from science fiction to near-commercial. (TerraPower, Commonwealth Fusion Systems, Type One Energy)
Manufacturing (30 percent of global emissions)
When someone tells you they know how to curb emissions, the first question you should ask is: What’s your plan for cement and steel? They’re key to modern life, and they’re hard to decarbonize on a global scale because it’s so cheap to make them with fossil fuels.
- Zero-emissions steel exists today. It’s made using electricity, so if you can get clean electricity that’s cheap enough, you end up with clean steel that’s cheaper than the conventional type. The technology still needs to get into more markets, and companies that make clean steel need to expand their capacity. (Boston Metal, Electra)
- Clean cement faces similar hurdles. Several companies have found ways to make it with no Green Premium, but it takes years to get a foothold in the global market and ramp up manufacturing capacity. (Brimstone, Ecocem, CarbonCure, Terra CO2, Fortera)
- One of the biggest energy surprises of the past decade is the discovery of geologic hydrogen. Eventually, hydrogen will be widely used to make clean fuels and will help with clean steel and cement. Today we make it from fossil fuels or by running electricity through water, but geologic hydrogen is generated by the Earth itself. Companies have already proven that they can find it underground; now the challenge is to extract it efficiently. There’s also been a lot of progress on making hydrogen with electricity much more cheaply than current technology does it. (Koloma, Mantle8, Electric Hydrogen)
- Companies are beginning to roll out ways to either capture carbon from facilities that currently emit it, such as cement and steel plants, or to remove it directly from the air and store it permanently. If captured carbon becomes cheap enough, we could even use it to make things like sustainable aviation fuel. (Heirloom, Graphyte, MissionZero, Deep Sky)
Agriculture (19 percent of global emissions)
Much of the emissions from agriculture comes from just two sources: the production and use of fertilizer, and grazing livestock that release methane.
- Farmers can already buy one replacement for synthetic fertilizer that’s made without any emissions, and another that turns the methane in manure into organic fertilizer. Both are selling at a negative Green Premium. Now the challenge is to produce them in large quantities and persuade farmers to use them. (Pivot Bio, Windfall Bio)
- Additives to cattle feed that keep livestock from producing methane are nearly cheap enough to be economical for farmers, and a vaccine that does the same thing has been shown to work. It’s now moving into the next stage of development. (Rumin8, ArkeaBio)
- Another source of methane is the cultivation of rice, one of the world’s most important staple foods. Companies are helping rice farmers around the world adopt new methods that both reduce methane emissions and increase crop yields. (Rize)
- One stubborn problem is that some of the nitrogen in fertilizer seeps into the atmosphere as nitrous oxide, a potent greenhouse gas. It’s very dilute, which makes it hard to capture.
Transportation (16 percent of global emissions)
Nearly one in four cars sold in 2024 was an EV, and more than 10 percent of all vehicles in the world are electric. In some countries including the U.S., they still have disadvantages, such as long charging times and too few public charging stations, that keep them from being as practical as gas-powered cars. In addition, cars and trucks are just one part of this sector, which also includes tough-to-decarbonize activities like shipping and aviation.
- Airplane emissions are projected to double by 2050, and clean jet fuel still comes with a Green Premium of over 100 percent. Today we know of only two cost-effective ways to make it: produce it with algae, or make synthetic fuel using very cheap hydrogen. Companies are in the early stages of work on both approaches.
- As more transportation goes electric, the demand for batteries is going to increase, which is why companies have developed ways to make them cheaper and more efficient. (KoBold Metals, GeologicAI, Redwood, Stratus Materials)
Buildings (7 percent of global emissions)
Heating and cooling buildings is the smallest slice of global emissions today, but it’s going to skyrocket with urbanization and the growing need for air conditioning.
- Electric heat pumps are widely available, up to five times more efficient than boilers and furnaces, and often the cheaper option. But there aren’t enough skilled workers around the world to install them. Next-generation, extra-efficient heat pumps are already on the market, and ones that are easier to install are in the works. (Dandelion, Blue Frontier, Conduit Tech)
- Other zero Green Premium products are available, including building sealants and super-efficient windows. But as with so many clean technologies, reaching scale takes time. (Aeroseal, Luxwall)
The global temperature doesn’t tell us anything about the quality of people’s lives. If droughts kill your crops, can you still afford food? When there’s an extreme heat wave, can you go somewhere with air conditioning? When a flood causes a disease outbreak, can the local health clinic treat everyone who’s sick?
Quality of life may seem like a vague concept, but it’s not. One useful tool for measuring it is the United Nations’ Human Development Index, which provides a snapshot of how people in a country are faring—from 0 to 1, with higher numbers meaning better outcomes.
If you look through a list of the HDI scores of the world’s countries, the disparities leap out at you. Switzerland has the highest HDI, at 0.96. South Sudan, the lowest, is at 0.33. The 30 countries with the lowest HDI scores are home to one out of every eight people on the planet, but they produce only about one third of 1 percent of global GDP. They have the highest poverty rates and, tragically, the worst health outcomes. A child born in South Sudan is 39 times more likely to die before her fifth birthday than one born in Sweden.
This inequity is the reason our climate strategies need to prioritize human welfare. This may seem obvious—who could be against improving people’s lives?—but sometimes human welfare takes a backseat to lowering emissions, with bad consequences.
For example, a few years ago, the government of one low-income country set out to cut emissions by banning synthetic fertilizers. Farmers’ yields plummeted, there was much less food available, and prices skyrocketed. The country was hit by a crisis because the government valued reducing emissions above other important things.
Sometimes the pressure comes from outsiders. For example, multilateral lenders have been pushed by wealthy shareholders to stop financing fossil fuel projects, with the hope of limiting emissions by leaving oil, gas, and coal in the ground. This pressure has had almost no impact on global emissions, but it has made it harder for low-income countries to get low-interest loans for power plants that would bring reliable electricity to their homes, schools, and health clinics.
Granted, situations like these are complicated, since burning fossil fuels helps people now at the cost of making the climate worse for people in the future. But remember that climate change is not the biggest threat to the lives and livelihoods of people in poor countries, and it won’t be in the future. In the next section, I’ll explain why and what it means for our climate strategies.
A few years ago, researchers at the University of Chicago’s Climate Impact Lab ran a thought experiment: What happens to the number of projected deaths from climate change when you account for the expected economic growth of low-income countries over the rest of this century? The answer: It falls by more than 50 percent.
This finding is exciting because it suggests a way forward. Since the economic growth that’s projected for poor countries will reduce climate deaths by half, it follows that faster and more expansive growth will reduce deaths by even more. And economic growth is closely tied to public health. So the faster people become prosperous and healthy, the more lives we can save.
When you look at the problem this way, it becomes easier to find the best buys in climate adaptation—they’re the areas where finance can do the most to fight poverty and boost health.
At the top of that list is improvements in agriculture.
Most poor countries are still largely agrarian economies. The average smallholder farmer in these countries has between two and four acres and makes about $2 a day. And she gets relatively little from her fields, about 80 percent less per acre than an American farmer. A single drought or flood can wipe her out for an entire season.
Lower emissions will eventually lead to fewer devastating losses, but today’s farmers don’t have time to wait for the climate to stabilize. They need to raise their incomes and feed their families now.
Mobile phones are already making a dramatic difference. Farmers use their phones to get advice on what to plant, when to plant, and when to fertilize that’s tailored by artificial intelligence to account for their soil, weather, and other local conditions. In India, during the most recent summer monsoon, around 40 million farmers in 13 states received an advance warning by SMS that the rains would arrive early and then pause. That single message saved millions of acres of crops.
And the technology is improving rapidly: In the next five years, a low-income farmer will be able to get better advice than anything that’s available to the richest farmers today.
Advances in crop breeding are another great buy, and Kenya has set an excellent example. Nearly 20 years ago, a group of African agricultural scientists saw that hotter, drier seasons were putting staple crops like maize under stress. So with support from the Gates Foundation and others, they developed a variety that could thrive in a changing climate. It worked: The new seeds gave a group of Kenyan farmers 66 percent more maize, enough to feed a family of six for a year and still have $880 worth of crops left over to sell. That’s equivalent to five months of income for them.
The list of innovations goes on. For example, researchers have helped farmers identify breeds of cattle that are naturally more resilient in tough conditions. And the new class of natural zero-emissions fertilizers I mentioned earlier is being tailored to the conditions in low-income countries. Scientists at the Tamil Nadu Agricultural University in India found that when smallholder farmers added these biofertilizers to their fields, their yields went up as much as 20 percent.
Improvements like these need to go hand in hand with improvements in health. I think if you ask most people how they think climate will affect health, they’ll talk about heat waves and natural disasters. So let’s start there and look at the facts.
Excessively hot weather now causes around 500,000 deaths every year. Despite the impression you’d get from the news, though, the number has been decreasing for some time, chiefly because more people can afford air conditioners. And, surprisingly, excessive cold is far deadlier, killing nearly ten times more people every year than heat does. As for what will happen in the future, heat deaths will go up and cold deaths will go down. The best current estimates suggest that the net effect will be a global rise in temperature-related mortality, and that most of the increase will be in developing countries.
The story so far with natural disasters is similar. In the past century, direct deaths from natural disasters, such as drowning during a flood, have fallen 90 percent to between 40,000 and 50,000 people a year, thanks mostly to better warning systems and more-resilient buildings.
But indirect deaths from natural disasters have not followed the same pattern of decline. In most cases today, people caught in storms and floods are more likely to die from a waterborne disease than from drowning. When floodwaters contaminate drinking water, they create ideal breeding grounds for cholera and rotavirus, which cause diarrhea and are especially deadly for children. More floods equals more diarrheal deaths.
But pathogens don’t wait around for storms or floods to infect people. Diarrheal diseases kill more than a million people a year, and the vast majority of infections don’t happen in a sudden tragic flash. They’re part of life in a low-income country. And, sadly, they’re not the only ongoing health threat.
If you include the other major causes of death in poor countries—malaria, TB, HIV/AIDS, respiratory infections, and complications from childbirth—poverty-related health problems kill about 8 million people a year.
And the burden is even worse when you factor in the health problems that don’t kill people but make them too sick to work, go to school, or take care of their kids. If a pregnant woman is already malnourished and then has her food supply cut off because of a flood, she’s even more likely to give birth prematurely, and her baby is more likely to start life underweight. But if she’s well-nourished to begin with, she and her baby have a much better chance to stay healthy.
I’m not saying we should ignore temperature-related deaths because diseases are a bigger problem. In fact, temperature-related deaths are one of the reasons why cheap clean energy is so important—it will make heating and air conditioning more affordable everywhere.
What I am saying is that we should deal with disease and extreme weather in proportion to the suffering they cause, and that we should go after the underlying conditions that leave people vulnerable to them. While we need to limit the number of extremely hot and cold days, we also need to make sure that fewer people live in poverty and poor health so that extreme weather isn’t such a threat to them.
Artificial intelligence has already begun to help do that. Today, for example, AI-powered devices make it possible for health workers to provide ultrasound exams for pregnant women in low-income settings—a breakthrough that means many more women will get the treatment they need to survive childbirth and deliver a healthy baby. AI is also helping researchers develop new vaccines and treatments faster, adding to the long list of affordable lifesaving tools that are already available, including vaccines, biofortified foods, bed nets, and treatments for diseases like AIDS, malaria, and tuberculosis.
The benefits of improving health and agriculture go beyond climate resilience. For example, as child survival rates go up, something unexpected takes place: People choose to have smaller families. When this happens, governments of poor countries can invest more in schools and health clinics, roads and ports, and sanitation systems and power grids. These things in turn make it easier to improve health and raise incomes. It is a remarkable virtuous cycle and it is set in motion by better health and agriculture.
In this memo, I’ve argued that we should measure success by our impact on human welfare more than our impact on the global temperature, and that our success relies on putting energy, health, and agriculture at the center of our strategies.
Development doesn’t depend on helping people adapt to a warmer climate—development is adaptation.
Under Brazil’s leadership, adaptation and human development will get more attention at COP30 than at any other COP. That’s a promising first step.
For COP30 and beyond, I see two priorities that I hope the climate community will embrace.
1.
Drive the Green Premium to zero.
At each COP, governments take turns announcing commitments to lower their emissions. Unfortunately, this process doesn’t tell us which technologies are needed to meet those commitments, whether we have them yet, or what it will take to get them.
This is why, in addition to country-by-country commitments, every COP should have high-level discussions and commitments based on the five sectors. Policies and innovations in each sector need to get more visibility. Representatives from each of the five sectors should report on progress toward affordable and practical zero-carbon innovations, using the Green Premium as their yardstick.
Government leaders would get a view into whether they can meet their commitments with existing tools. They would see, sector by sector, which technologies they can start adopting now, which ones they should plan to roll out soon, and which ones still need government action to reduce the Green Premium. They would talk to their peers from other countries about working together on promising breakthroughs that will help everyone meet their commitments.
If you’re a policymaker, you can bring this sector-by-sector focus on the Green Premium to your government’s work. You can also protect funding for clean technologies and the policies that promote them. This is not just a public good: The countries that win the race to develop these breakthroughs will create jobs, hold enormous economic power for decades to come, and become more energy independent.
If you’re an activist, you can call for steps that make clean alternatives in every sector as cheap and practical as their fossil fuel counterparts. The public is more likely to switch to clean technology when it’s cheaper and better than fossil fuels.
If you’re a young scientist or entrepreneur, this is a moment to rethink what it means to change the world. The people working on clean materials today will have an enormous impact on human welfare. If you need pointers, the Climate Tech Map published last month by Breakthrough Energy and other partners is an excellent guide to the technologies that are essential for decarbonizing the economy.
If you’re an investor, I encourage you to invest in companies working on high-impact clean technologies that will eventually have no Green Premium. I’m putting more of my own money into these efforts because reducing the Green Premium to zero demands more for-profit capital. It’s also a fantastic investment in what will be the biggest growth industry of the 21st century. (I will give any profits I make from my investments to the Gates Foundation.)
2.
Be rigorous about measuring impact.
I wish there were enough money to fund every good climate change idea. Unfortunately, there isn’t, and we have to make tradeoffs so we can deliver the most benefit with limited resources. In these circumstances, our choices should be guided by data-based analysis that identifies ways to deliver the highest return for human welfare.
Vaccines are the undisputed champion of lives saved per dollar spent. Since 2000, Gavi has spent $22 billion to immunize children in poor countries, preventing 19 million deaths. That means Gavi can save a life for a little more than $1,000. Other estimates find that vaccines cost less than $5,000 per life saved. And vaccines become even more important in a warming world because children who aren’t dying of measles or whooping cough will be more likely to survive when a heat wave hits or a drought threatens the local food supply.
Every effort in the world’s climate agenda should undergo a similar analysis and be prioritized by its ability to save and improve lives cost-effectively. Malaria prevention, for example, is nearly as good as vaccines on the basis of cost per life saved. Energy innovation is a good buy not because it saves lives now, but because it will provide cheap clean energy and eventually lower emissions, which will have large benefits for human welfare in the future. Many of the best buys in agricultural innovation will be on display at COP30 in a showcase hosted by the Gates Foundation, the Brazilian government, and other partners.
This moment reminds me of another time when I called for a new direction.
Thirty years ago, when I was running Microsoft, I wrote a long memo to employees about a major strategic pivot we had to make: embracing the internet in every product we made.
It seems like an obvious move now, given that online activity is such an integral part of everyone’s life, but at the time, the internet was just entering the mainstream. If we hadn’t adjusted our strategy, our success would have been at risk.
For a company, it's relatively easy to make a shift like that because there’s only one person in charge. By contrast, there is no CEO who sets the world’s climate priorities or strategies, which is exactly as it should be. These are rightly determined by the global climate community.
So I urge that community, at COP30 and beyond, to make a strategic pivot: prioritize the things that have the greatest impact on human welfare. It’s the best way to ensure that everyone gets a chance to live a healthy and productive life no matter where they’re born, and no matter what kind of climate they’re born into.

Life and death
How to cut child mortality in half… again
We already know how to save millions of newborn lives.

When Paul Allen and I started Microsoft, we had an ambitious goal: to put a computer on every desk and in every home. A lot of people thought we were out of our minds. But we believed in the power and potential of these machines to change the world. So every day, we came to work determined to make it happen. Now, it’s hard to imagine the world any other way. In a few short decades, that goal became reality for billions.
In 1990, the possibility that the world would be able to cut child mortality in half over the next thirty years would have seemed just as remote. But that’s exactly what happened. And I believe the world can do it again by 2040—we can cut child mortality in half once more—and get even closer to ending all preventable child deaths.
My introduction to this issue came 27 years ago, when I read a piece in The New York Times about deadly drinking water in the world’s poorest countries that contained the following statistic: “Diarrhea kills some 3.1 million people annually, almost all of them children.” Learning that shocked me to my core. There’s no greater pain than the death of a child. The death of millions of them—from something easily treatable in much of the world—is tragedy after tragedy on an almost unfathomable scale.
Before long, I was learning everything I could about global health generally and child mortality specifically. And shortly after, the Gates Foundation, which was just getting off the ground, made it our mission to fight preventable health disparities like this around the world—with an emphasis on children whose lives were being cut short before they ever had a chance.
My look ahead
What it takes to take a breath
New tools can help millions more newborns—and their mothers—survive.

In a rural health clinic, a baby tries to take her first breath.
But her lungs aren’t ready. Because she was born too early, they haven’t developed the slick, soap-like substance that keeps her air sacs from collapsing. Without that substance—called lung surfactant—breathing becomes a desperate, exhausting act.
She’s suffering from respiratory distress syndrome, or RDS, a life-threatening condition that appears within hours of birth in premature babies. Unless she gets treatment, her oxygen levels will plummet and her organs will begin to shut down. In one study from India, every baby born with RDS outside of a hospital setting died. In Ethiopia and Nigeria, RDS is responsible for almost half of all neonatal deaths.
At hospitals in higher-income countries, there’s a way to save her: a liquid form of organically-derived surfactant delivered directly into the lungs. But the procedure requires a highly-trained specialist to guide a breathing tube down the newborn’s windpipe—avoiding the stomach and placing it just right—at a cost of up to $20,000. In many parts of the world, that kind of care simply doesn’t exist.
But what if any healthcare worker anywhere in the world could simply hold a small nebulizer to the baby's face and deliver surfactant as an easy-to-administer inhalant?
This breakthrough—a synthetic surfactant that’s stable enough to be delivered through a nebulizer—is still in development, drive in part by Gates Foundation-supported research at Virginia Commonwealth University, Seattle Children’s Research Institute, and The Lundquist Institute. But its promise is extraordinary: an RDS treatment that costs less to make, doesn’t require a specialist to administer, and eliminates the need for intubation.
In other words, a therapy currently limited to the most advanced hospitals could become accessible in rural clinics and community settings around the world. Even in places with top-tier care, it could make treatment gentler, faster, and easier to deliver. In the United States—where RDS still affects 24,000 newborns a year—it could reduce the risks that come with intubating babies who might weigh only two or three pounds.
It’s the kind of innovation that could help solve one of the most persistent problems in global health: delivering intensive care without an intensive care unit, and helping millions more babies survive their first, most fragile moments.
Since 1990, the mortality rate for children under five has been cut by more than half—an amazing mark of global progress. But another statistic hasn’t fallen as fast: the number of babies who die in their first month of life.
Each year, 2.3 million newborns don’t survive past their first 28 days. And the day a baby is born is the most dangerous day of their life. The single biggest cause of these deaths is prematurity. Nearly 900,000 babies a year die from complications related to being born too soon, including infection, underdeveloped organs, and RDS.
Lower cost, easier-to-deliver surfactant is one way to give newborns a fighting chance, but it’s not the only way. Around the world, simple, affordable interventions already exist to identify at-risk pregnancies earlier, prevent more preterm births, and ensure a healthy birthing experience for mothers. Not only are these tools designed to work in the hardest-to-reach places—many of them start working even before a baby takes that first breath.
One of these innovations is a new type of ultrasound that’s changing who can catch the risks of preterm birth—and where.
Around the world, two thirds of women never get an ultrasound screening during pregnancy. Traditional machines are bulky and expensive, with specialized training required to operate them and interpret their results. In places where medical resources are already stretched thin, these types of ultrasounds are rarely an option.
But now, we have ultrasound devices about the size of a phone that can be operated by a nurse or midwife—no on-site specialist required. They weigh less than a pound. They process scans instantly. Their AI interface automatically detects high-risk conditions, like a shortened cervix or signs of early labor, so patients are referred for further care. And they have built-in telehealth functions to share images with remote specialists when needed.
By finding and flagging risks early, these AI-enabled ultrasounds are giving healthcare workers more time to act. In some cases, that means transferring the mother to a higher-level facility. In others, it means providing her with antenatal steroids—an inexpensive, underused treatment that speeds up fetal lung development—and, when needed, medications that delay labor just long enough for those steroids to take effect.
Early warning is essential, but we can save even more lives by going further upstream, starting with the health of pregnant women themselves.
In many low-income countries, undernutrition isn’t an exception. It’s the norm. And the intense demands of pregnancy make nutritional deficiencies even worse—putting mothers at increased risk of complications or death in childbirth, and raising the odds of early labor, low birth weight, and developmental delays for their babies.
But there’s a surprisingly simple fix: a daily supplement called MMS, or multiple-micronutrient supplementation, developed by the United Nations. It contains 15 essential vitamins and minerals for pregnancy—like zinc to reduce the risk of early labor, folic acid to help prevent birth defects, iron and vitamin D for healthy birth weight, and iodine for brain development. For an entire pregnancy, it costs just $2.60.
If MMS became the standard prenatal supplement in every low- and middle-income country, it could save nearly half a million newborn lives each year—and prevent serious complications in 25 million births by 2040.
The innovations above focus on treating, detecting, and preventing premature birth, a huge threat to newborn survival. But one of the most powerful ways to protect babies, preterm or full-term, is by ensuring their mothers stay healthy through pregnancy and childbirth.
When a woman dies during delivery, her baby is 46 times more likely to die in that first month of life. That’s why any serious effort to tackle infant mortality must also address postpartum hemorrhage—which tragically kills 70,000 women a year and is the leading cause of maternal mortality. Fortunately, two innovations are already helping healthcare workers catch and treat it before it becomes fatal.
The first is a calibrated drape—a simple plastic sheet placed under a woman during delivery that collects blood and shows, through printed measurement lines, exactly how much she’s losing. It gives healthcare workers a fast, accurate way to spot dangerous bleeding before it becomes life-threatening. The second is a one-time, 15-minute iron infusion during pregnancy that treats severe anemia—so if a woman does hemorrhage during childbirth, she’s less likely to experience catastrophic blood loss and more likely to survive.
Neither of these tools is complicated or expensive. But in combination, they can make a life-or-death difference for mothers and the babies who depend on them.
Taken together, these innovations form a chain of survival. They help mothers stay healthy through pregnancy. They detect problems before they become emergencies. They give fragile newborns a fighting chance. And they make it possible for families to celebrate a baby’s birth rather than mourning a loss.
Some of these tools are already saving lives. Others are on the verge of doing so. But their impact will be limited unless we prioritize and fund their delivery, not just their development. The world needs to make sure these innovations don’t get stuck in labs or warehouses—so they can reach the mothers and babies who need them most.
My look back
The breakthrough that transformed the Gates Foundation
This is the story of how better data helped us cut child mortality in half.

We started the Gates Foundation 25 years ago to save and improve children’s lives. But no one can solve a problem they don’t fully understand. And back in 2000, the world’s understanding of childhood mortality was occasionally inaccurate, often imprecise, and almost always incomplete.
That’s why I believe the breakthrough that transformed our foundation in the two-and-a-half decades since wasn’t a single vaccine or treatment—it was a revolution in the world’s understanding of childhood mortality. Through advances in how researchers collect and analyze global health data, we now know much more about what kills children, where these deaths occur, and why some kids are more vulnerable than others. By putting those insights to work, we’ve been able to save lives.
The first challenge was knowing exactly what was killing children.
Reading the 1993 World Development Report opened my eyes to the scale of the problem: Around 12 million children under the age of five were dying every year, with a staggering disparity between rich and poor countries. But the available data was fragmented and inconsistent. That made it difficult to understand trends or allocate resources effectively.
So the foundation helped create the Institute for Health Metrics and Evaluation at the University of Washington, to give a permanent home to the Global Burden of Disease study—originally developed in the 1990s by researchers at Harvard University and the World Health Organization. We wanted to expand it from a static snapshot of the problem into a regularly updated tool that tracked how diseases impact people around the world. That gave us something the world never had before: a comprehensive—and current—picture of child mortality across every country.
Measuring symptom-based causes of children’s deaths was an important step. But broad disease categories like “diarrhea” or “respiratory infection” didn’t give us enough information to act on. We needed to know which specific pathogens were responsible for the most common and fatal cases. So the Gates Foundation funded two landmark studies to find out.
In 2013, the Global Enteric Multicenter Study, or GEMS, found that rotavirus was causing 20 percent of lethal diarrhea cases in kids. At the time, diarrhea was the second-leading infectious killer of children. While oral rehydration therapy had already helped bring down deaths over previous decades, GEMS helped fast-track the rollout of a more targeted tool—a new rotavirus vaccine—in the hardest-hit countries, in close partnership with Gavi, the Vaccine Alliance.
A year later, the Pneumonia Etiology Research for Child Health study, or PERCH, revealed that respiratory syncytial virus, or RSV, was a much more common cause of severe pneumonia—the leading infectious killer of kids around the world—than previously understood. (And not just in low- and middle-income countries, where 97 percent of RSV deaths occur, but in higher-income ones too, where the virus still fills pediatric hospital wards each winter.) That prompted us to expand our investments in RSV prevention, which led to the approval of the first maternal vaccines for RSV in 2023.
But understanding what causes childhood mortality wasn’t enough on its own, because deaths aren’t distributed evenly across countries—or even within them. That’s why our second challenge was to figure out where exactly children were dying.
At the time, most health data was collected at national or regional levels. That masked major differences in disease burden from one community to the next—and made it harder to target interventions effectively.
To solve this second challenge, the foundation invested in new approaches to health mapping that combined satellite imagery, GIS technology, GPS data, and local health surveys. These maps gave Ministries of Health and implementing partners unprecedented, anonymized detail about disease patterns and population distribution, down to individual neighborhoods, that transformed how and where public health resources are deployed—while still preserving the privacy of the individual children and families in these places.
In Pakistan—one of just two countries where wild polio remains endemic—advanced mapping tools have helped vaccination teams reach and protect kids in settlements that weren’t on any official maps. Across sub-Saharan Africa, better geographic data has transformed the fight against malaria by revealing that transmission often clusters in small, hyper-local pockets. Through the Malaria Atlas Project, countries like Nigeria can now track those patterns more precisely—and then get bed nets, testing, and treatment where they’ll have the greatest impact.
With better knowledge of what was killing children, and where, one more fundamental question remained: Why might one child die from a disease while another—who lives in the same place, faces the same risks, and gets the same treatment—survives? This was our third big challenge.
In theory, traditional autopsies would provide the answer. But in the places where most childhood deaths still occur, these invasive procedures are often impossible to perform—too costly, and sometimes opposed for religious, cultural, or personal reasons.
So in 2015, the foundation launched the Child Health and Mortality Prevention Surveillance network, or CHAMPS, which now operates in nine countries across Africa and South Asia. Working with in-country partners, CHAMPS pioneered a new autopsy alternative—using minimally invasive tissue sampling—that can determine causes of death quickly and accurately while respecting local customs and beliefs.
Through CHAMPS, we discovered that childhood deaths rarely have a single cause. Instead, kids often have multiple conditions at the same time, with malnutrition frequently leaving them much more vulnerable to a whole host of infections. (While it rarely shows up on death certificates, it’s an underlying cause of death in nearly half of all child mortality cases.) That finding helped solidify nutrition as a core focus of the foundation’s global health work—and the research, innovation, and product development we invest in. On the ground, we’re supporting partners as they integrate nutrition screening into routine care and train healthcare workers to manage multiple risks at once.
CHAMPS also demonstrated that inadequate prenatal care is responsible for a majority of stillbirths, newborn deaths, and maternal deaths, prompting us to further expand access to maternal health services—like prenatal vitamins and AI-enabled ultrasounds—in the communities where we work.
But the biggest takeaway from CHAMPS is also the most hopeful—and a reminder of why we started the Gates Foundation in the first place: So many childhood deaths could be prevented with existing interventions. We just need to ensure they reach the right children at the right time.
Twenty-five years in, our work on child mortality is far from complete. Still, the impact of what we have learned has been enormous
The Global Burden of Disease, GEMS, and PERCH studies helped shift global priorities by showing the world what was really killing kids—and where new vaccines and treatments could make the biggest difference. Better geospatial tools have empowered countries to pinpoint disease hotspots, find previously unmapped settlements, and distribute life-saving resources where they’re needed most. And CHAMPS is giving governments better data on why children are dying—data that’s now shaping policies, improving reporting, and guiding more effective care.
Most importantly, even as the number of children born every year has gone up, the number of overall childhood deaths has fallen by more than half—from 11.3 million in 1990 to 4.5 million in 2022. Playing a part in making that happen is the best job I’ve ever had, and the most meaningful work I’ve ever done.
At the Gates Foundation, we used to say we could cut child mortality in half again by 2040. The truth, though, is that goal feels further out of reach now—not because the science has stalled, but because support for global health has. The progress we’ve been part of was only possible because governments around the world, including here in the U.S., made long-term commitments to saving lives and followed through. That kind of leadership gave millions of children who would have died a chance at life—and made life better for millions more.
The last 25 years have shown us what’s possible. The next 25 will depend on whether the world keeps showing up for the children who need it most.
PrEP talk
From once a day to twice a year
Long-acting preventatives will save more lives from HIV/AIDS.

I’ve been working in global health for two and a half decades now, and the transformation in how we fight HIV/AIDS is one of the most remarkable achievements I’ve witnessed. (It’s second only to how vaccines have saved millions of children's lives.)
At the dawn of the AIDS epidemic, an HIV diagnosis was often a death sentence. But in the years since, so much has changed. Today, not only do we have anti-retroviral medications that allow people with HIV to live full, healthy lives with undetectable viral loads—meaning they can’t transmit the virus to others. We also have powerful preventative medications known as PrEP, or pre-exposure prophylaxis, that can reduce a person’s risk of contracting the virus by up to 99 percent when taken as prescribed. It’s an incredible feat of science: a pill that virtually prevents HIV contraction.
In theory, if we could get these tools to everyone who needs them and make sure they’re used correctly, we could stop HIV in its tracks. Because when people with the virus receive proper treatment, they can’t transmit it to others. And when people at risk take PrEP, they can’t contract it. In practice, however, getting these tools to people—and making sure they’re used correctly—is the hard part. Especially for PrEP.
That’s because current preventatives require people to take medication every single day. Miss a dose, and protection drops. It’s like trying to remember to lock your front door 365 times a year—if you mess up once, you’re vulnerable. For many people, the barriers stack up quickly. Some have to walk hours to reach a clinic. Others struggle to store medication safely or discreetly at home. And many face judgment and stigma for taking PrEP, especially young women in conservative communities. The very act of protecting yourself can lead to being shamed or ostracized.
That’s why I’m so excited about a new wave of innovations in HIV prevention. Scientists are in the process of developing several longer-lasting PrEP breakthroughs, each with distinct advantages that could help more people protect themselves on their own terms.
Lenacapavir, which requires only two doses per year through injection, could open HIV prevention up to people who can’t make frequent clinic visits. Cabotegravir, another injectable option that works for two months at a time, offers a more flexible dosing schedule than daily PrEP pills, too. Meanwhile, a monthly oral medication called MK-8572, still in the trial stage, could provide an alternative for people who prefer pills to injections. The Gates Foundation is even exploring ways to maintain a person’s protection for six months or longer. And researchers are working on promising PrEP options that include contraception, which would be particularly valuable for women who need both types of protection.
To understand how these options work in real life, and not just in labs, our foundation has supported implementation studies in South Africa, Malawi, and elsewhere. Unlike traditional clinical trials that test safety and efficacy in highly controlled settings, these studies examine how medications fit into people’s lives and work in everyday circumstances—looking at ease of use, cultural acceptance, and other practical challenges. This real-world understanding is crucial for successful adoption.
Some people ask me if these new preventative tools mean the Gates Foundation has given up on finding an HIV vaccine. Not at all. In fact, these advances push us to aim even higher in our research for a vaccine that could prevent HIV for a lifetime—and not just a few months at a time. Our goal is to create multiple layers of protection, much like modern cars have seatbelts, airbags, and even collision-warning sensors. Different tools work better for different people in different ways, and we need every tool we can get.
But even the most brilliant innovations make no difference unless they reach the people who need them most. This is where partnerships become crucial. Through grants to research institutions around the world, the foundation is working to lower manufacturing costs for HIV drugs so they’re accessible to everyone, everywhere. Then there are organizations like the Global Fund and PEPFAR, which have been instrumental in turning scientific advances into real-world impact.
The Global Fund—which needs to raise significant new resources next year to continue its work—currently helps more than 24 million people access HIV prevention and treatment. And PEPFAR has saved 25 million lives since its inception in 2003—a powerful example of how American leadership can build tremendous goodwill while transforming the world. Motivated by the belief that no person should die of HIV/AIDS when lifesaving medications are available, President George W. Bush created PEPFAR with strong bipartisan backing and it continues to serve as a lifeline to millions of people.
We're at a pivotal moment in this fight. Twenty years ago, many believed it would be impossible to deliver HIV treatment at scale in Africa’s poorest regions. Since then, we’ve made fantastic progress. Science has shown us promising paths forward—for better prevention options, easier treatment regimens, and, maybe one day, an effective vaccine. Our task now? Ensuring the life-saving innovations we already have reach the people whose lives they can save.

Game changer
Grassroot Soccer scores a hat trick for African youth
This organization uses the beautiful game to reach millions of young people with lifesaving services.

I’ve never been much of a soccer fan. (Tennis and pickleball are my favorite sports.) Still, seeing the athleticism and passion on display during the World Cup, I understand why soccer has earned the nickname “the beautiful game.” What makes soccer even more beautiful is the positive impact it can have off the field.
There may be no better example of this than the work of a unique non-profit organization called Grassroot Soccer, which was featured at a health innovation event where I spoke earlier this week.
For the last two decades, Grassroot Soccer has used the incredible popularity of the game to help young people across Africa navigate some of their toughest health challenges.
Despite significant progress in health and development in Africa, including a dramatic decline in child mortality, HIV/AIDS continues to be a leading cause of death among youth in Africa. Sexual violence threatens the health and safety of girls. A lack of access to contraceptives contributes to high rates of teen pregnancy. And mental health services are often unavailable.
Solving these challenges is difficult—and especially important given that 60 percent of Africans are under the age of 25. So, how can soccer make a difference?
Because it’s so popular, soccer offers a hook to capture the attention of young people. Grassroot Soccer uses the game to involve them in activities that encourage them to live healthier, more productive lives.
Here’s one simple example. In an activity called “Risk Field,” players are asked to dribble a soccer ball through cones labeled with some of the risky behaviors that young people often encounter, such as unprotected sex, HIV, multiple partners, and alcohol.
The local youth who serve as Grassroot Soccer coaches are a critical component of the program. Trained in basic counseling skills, the coaches play an important role as trusted mentors to the young participants.
The coaches also accompany adolescents to clinics where they can get HIV testing, contraceptives, and other services. (In some countries, young people might be turned away because of their age or criticized by health staff for seeking contraceptives and testing. The coaches serve as advocates to support their right to health services.) Coaches also conduct home visits to talk with parents and guardians about their programs and health services.
Founded in 2002 by Dr. Tommy Clark, a pediatrician and former professional soccer player, Grassroot Soccer initially focused on stopping the spread of HIV. (The Gates Foundation was an early funder of its work.) Today the organization works in more than 60 countries and has reached more than 18 million young people.
Studies have shown that its participants had better access to sexual and reproductive health services, were more likely to stick with their HIV treatment, and were less likely to experience depression.
That kind of impact gives everyone, even casual soccer fans like me, something to cheer about.
The last mile
We’re closer than ever to eradicating polio
...And closer than ever to seeing a resurgence.

When most Americans think of polio, we probably picture President Franklin Delano Roosevelt. In 1921, at age 39, he was paralyzed by the virus and never regained the use of his legs. His story helped turn polio into a national cause. But in many ways, his experience was an anomaly.
After all, polio is overwhelmingly a childhood disease, with the vast majority of cases affecting those younger than five. That was true when FDR fell ill, and it’s true today. The typical patient isn’t an adult with an already established political career—it’s a little kid, often a little kid in a low-income country, who might never get the chance to take his first steps.
That injustice is one big reason I've spent the past two decades working to eradicate polio. The other reason is that eradication is actually possible, realistic, and well within reach. This is a disease we can get rid of—not just control, but eliminate everywhere. That is a rarity in global health.
The world has already made extraordinary progress. Back in 1988, when Rotary International and the World Health Assembly set the goal of eradication, the virus was paralyzing more than 350,000 children each year across 125 countries. Since then, cases have dropped by 99.9 percent. The strains known as Type 2 and Type 3 wild poliovirus have been eradicated. The entire African continent is certified wild-polio free. Only two countries—Afghanistan and Pakistan—still have persistent transmission of Type 1 wild poliovirus.
Now we're closer than ever to total polio eradication. But the last mile is proving the hardest because viruses find ways to exploit any immunity gaps or weaknesses. Wherever vaccination rates slip—even briefly—they can resurface.
One of the biggest challenges comes from what are called variant outbreaks. In communities where immunization is low, the weakened virus used in the oral polio vaccine can circulate asymptomatically and rarely, over time, mutate enough to regain the ability to cause paralysis in unvaccinated children.
While most variant outbreaks happen in places with extremely low vaccination coverage, poor sanitation, and weaker health systems, no place is risk-free until the world is polio-free. In 2022, the United States confirmed its first paralytic polio case in nearly a decade, and the virus was detected in New York wastewater samples. In the time since, variant polioviruses have also been found in the U.K., Ukraine, Indonesia, and other countries.
The good news is that today’s tools are better than anything we had even five years ago, and they make every dollar spent on the cause go further than ever before. We have a new oral vaccine, nOPV2, that’s far less likely to mutate and lead to new variant outbreaks; nearly two billion doses have already been given worldwide. New regional labs in Ghana, Nigeria, South Africa, and Uganda that test wastewater samples and sequence viruses have cut detection times by over 30 percent, which gives health workers a critical head start on outbreak response. And the surveillance network for polio is one of the most sophisticated ever built—also helping alert public health officials to outbreaks of cholera, measles, Ebola, and even COVID-19 at the height of that pandemic.
The Gates Foundation has been proud to support these advances as part of the Global Polio Eradication Initiative, a coalition of the WHO, UNICEF, the CDC, Gavi, Rotary International, and dozens of countries’ governments. It’s one of the most successful collaborations in the history of global health.
But right now, GPEI is facing a $1.7 billion funding gap, with various long-term donor governments cutting back their support. Without the right resources, vaccination campaigns may have to be scaled back, surveillance sites will likely close, and the virus could spread globally.
In the century since FDR was paralyzed by the virus, American leadership and generosity have helped turn polio into a fight the whole world could win. From the March of Dimes, which funded research, to the development of the first vaccines, to support for eradication campaigns, U.S. commitment has been decisive.
The world is at the brink of ending this terrible disease, and the stakes of this moment couldn’t be higher. If we finish the job, we free up billions of dollars for other health priorities and—most importantly—protect generations of children from a virus that has paralyzed millions. If we back down from the fight, up to 200,000 children could be paralyzed each year within a decade.
We have the scientific tools and infrastructure needed to cross the finish line. And we have hundreds of thousands of committed vaccinators who are determined to get us there—who go door to door across deserts, jungles, floodplains, and war zones to make sure no child is missed. I've met them, I've heard their stories, and I've seen how determined they are to finish the job.
We should be too.

Polio progress
Going door to door, this hero brings the world closer to ending polio
19 million people who would have otherwise been paralyzed are now walking today thanks to heroes like Shumaila Rehmani.

The world is so close to ending polio.
Since the start of the global eradication effort in 1988, the number of polio cases worldwide has fallen 99.9 percent.
19 million people who would have otherwise been paralyzed are now walking today because of vaccines. And 1.5 million people are alive who would have otherwise died from the disease.
Much of the credit for this progress goes to the thousands of polio workers who have gone door to door vaccinating more than 3 billion children over the last 33 years.
October 24 is World Polio Day and to mark the occasion I’d like to share the story of one of these dedicated polio fighters.
Her name is Shumaila Rehmani.
Shumaila is a polio vaccinator in Pakistan, which is one of the two countries in the world—the other is Afghanistan—where the wild poliovirus is still endemic.
Shumaila’s job is to deliver the polio vaccine to every child under age five in the community she serves. While that probably sounds like a straightforward job, what it takes to get it done is not. Reaching every child requires hard work, meticulous planning, and patience.
During polio immunization drives in Pakistan, Shumaila sets out on foot early in the morning with a cooler filled with vaccines and a detailed plan for all the homes she needs to visit. Then she begins knocking on doors to give the oral polio vaccine drops to every child.
The overwhelming majority of families she visits want their children to be vaccinated. Some parents, however, out of fear or a lack of information, refuse to have their children vaccinated.
But Shumaila doesn’t give up.
She talks with the mothers and fathers, answering all their questions about polio and reassuring them that the vaccine is safe and effective. She also works with community and religious leaders to speak with families about the importance of vaccination.
Progress can be slow. In the community she serves, Shumaila says this year she initially had more than 250 families refuse vaccinations. But today, because of her efforts to work closely with the families, all but four of them have had their children vaccinated. And she continues to talk with those families to encourage them to get vaccinated.
And thanks to the thousands of dedicated health workers like Shumaila and the leadership of Prime Minister of Pakistan Imran Khan, there’s been just one case of wild polio in Pakistan so far this year, compared with 84 in 2020.
While the incredible efforts of Shumaila and other polio fighters have brought us to the brink of a polio-free world, COVID-19 has created new challenges. The pandemic has disrupted polio campaigns and routine immunizations in many parts of the world, causing outbreaks of other forms of polio to crop up in Africa and Asia.
That’s why the global polio program adapted its approach to help contain the spread of COVID-19 while also working to end polio. The Global Polio Eradication Initiative used its workforce and laboratory and disease surveillance network to respond to the pandemic, investigating suspected COVID cases, coordinating response operations, and training health care workers. In Pakistan, the national polio team now operates a toll-free number for anyone who wants to speak with a doctor about COVID, polio, or get any questions answered about routine immunization. They have received more than 17 million calls during the pandemic.
Like other polio workers, Shumaila has used her community relationships to raise awareness of COVID, teach families how to stay safe, and provide handwashing and hygiene lessons. This has made for longer days, but Shumaila says it’s easy to stay motivated. As a mother of three children herself, she is driven by her dream of a day when polio will no longer be a threat to her children or any child in Pakistan.
It’s a day she knows will come soon, she says. Again and again since the start of the global polio eradication effort, one country after the next has eliminated this crippling disease from within their borders. Less than a decade ago, for example, Nigeria accounted for more than half of all wild polio cases worldwide. But last year, Nigeria, along with the 47 countries in the African region, were certified free of the wild poliovirus.
With Afghanistan recently announcing it would conduct a nationwide polio campaign in November—the first in over three years to reach all children in the country—and Pakistan’s continued commitment to eradication, the final two polio endemic countries will hopefully soon follow others on the path to ending wild polio.
“If other countries can be polio free, why can’t Pakistan be?” Shumaila asks.

Eyes on eradication
Optimism and resolve on Pakistan’s last mile to end polio
I made my first trip ever to Pakistan to learn about the country’s incredible efforts to wipe out polio.

Earlier this year, I made my first trip ever to Pakistan to learn more about the country’s incredible efforts to wipe out polio.
At the time of my visit in February, Pakistan had gone more than a year without a single child being paralyzed by the crippling disease. This was a huge achievement made possible by the skill and dedication of the polio program’s leadership and its more than 300,000 polio workers. Their energy and enthusiasm reminded me of what I saw in India and Nigeria when those countries were traveling the final mile to eliminate polio within their borders.
But the last mile is often the toughest. The gains made against this highly contagious disease are often fragile.
In recent weeks, the world received a sobering reminder of this fact when three new cases of wild poliovirus were detected in Pakistan: 12 and 15-month-old boys, and a two-year-old girl all living in the same district in Khyber Pukhtunkhwa Province, Pakistan, near the border with Afghanistan. (Pakistan and Afghanistan are the only two countries where the wild poliovirus has not been eliminated.)
It is heartbreaking to see these three children paralyzed by a preventable virus that has been eliminated in nearly every part of the world. (The government of Pakistan is providing rehabilitation services and other support to help the children and their families.)
At the same time, the emergence of these new cases was not entirely unexpected given the challenges of wiping out the virus in one of the most challenging places on Earth. The border region between Pakistan and Afghanistan, where the cases were detected, struggles with insecurity and misinformation that can sometimes prevent vaccinators from reaching every child who needs the polio vaccine.
When I learned about the new cases, I was disappointed. But I was also heartened by the response of Pakistan’s polio program. Despite having every reason to be frustrated, Dr. Shahzad Baig, who runs Pakistan’s National Emergency Operations Center for polio, said his team was not deterred. “This strengthens our resolve to reach every child with the polio vaccine,” he said.
After what I saw during my visit to Pakistan, I shouldn’t have been surprised by the team’s unfailing confidence. The polio workers are driven and detail oriented. They understand that running effective polio vaccination drives is not about getting one thing right. It’s about getting everything right that’s necessary to ensure all children get vaccinated.
In Pakistan, that has meant training 300,000 frontline workers who walk from house to house to vaccinate over 43 million children under the age of five; creating detailed maps for those teams to use to ensure no child is missed; running public information campaigns to inform communities about the risks of polio and the benefits of vaccination; organizing security to protect vaccinators; and building strong supply chains so vaccines are available across the country.
In between vaccination drives, Pakistan’s polio surveillance workers are constantly hunting for signs of acute flaccid paralysis in children and testing the environment for the presence of the virus. Pakistan currently has the largest environmental surveillance network in the world. From tiny villages to larger cities and urban areas, Pakistan’s system has the capacity to find the poliovirus wherever it exists.
The nerve center for all this work is the National Polio Emergency Operations Center, which was a highlight of my visit. A wall of screens in a control room displayed real-time information about vaccinations, security, and supplies, as well as detailed maps following the movements of polio workers. This data helps the team see where they need to make improvements to the vaccination programs to ensure they reach all the children. You probably know I have an insatiable appetite for data, especially health data. So, it should be no surprise I lingered here for longer than planned to look at all the information and learn from the polio experts who are as passionate about data as I am.
What was also remarkable to see is how Pakistan has continued to build community support for its polio activities by integrating them with other essential health programs, like routine immunization programs. During the pandemic, polio workers used their deep knowledge of local communities to reach out to families to raise awareness of COVID-19, teach them how to protect themselves with handwashing and mask wearing, and encourage people to get vaccinated.
Polio workers constantly battle rumors and misinformation about the polio vaccines. But by engaging openly with the public’s questions they’re making headway against this challenge.
I got a glimpse of part of this effort at a national immunization call center where doctors and other health workers respond to tens of thousands of queries every month from the public about immunization, including polio. If families hear a rumor about the polio vaccine, they can call for free and ask about it. Pakistan has reduced the number of vaccine refusals and I believe that the work of this call center is one of the key reasons why. The call center was set up to support polio inquiries, but due to the success of the program, the call center expanded its services to answer questions about COVID-19 vaccines and all other vaccines.
Pakistan’s polio effort also benefits from the strong support it receives from the very top of its government. I recently had an opportunity to speak with Pakistan’s new Prime Minister, Shehbaz Sharif, and it was clear that his administration is actively engaged in stopping transmission for good.
Even with the three new polio cases in Pakistan, the virus is still circulating at very low levels and the world has an historic opportunity to make sure this virus never paralyzes a child again. The fact is, we’ve never been closer to ending polio and it’s critical that the world doesn’t lose sight of this goal.
The last mile to end polio, of course, will be challenging. And that’s why it’s important that the world keep up its support for the polio programs in Pakistan and Afghanistan, so they don’t travel it alone.
I look forward to keeping you posted on their progress in the months ahead.
No fever dream
How the U.S. got rid of malaria
This is how a parasite helped build the CDC and changed public health forever.

I spend a lot of time thinking and worrying about malaria. After all, it’s one of the big focuses of my work at the Gates Foundation. But for most Americans, the disease is a distant concern—something that happens “there,” not here.
That’s true today. It wasn’t always.
It was especially rampant in the South, from the Carolinas and the Mississippi Delta down to Florida and all along the Gulf Coast.
Every summer, people braced for the start of “fever season.” In her Little House on the Prairie books, Laura Ingalls Wilder wrote about what she called “fever ‘n’ ague.” A laundry list of presidents—including George Washington, Andrew Jackson, Abraham Lincoln, and Ulysses S. Grant—battled the disease.
During the Civil War, Confederate General Robert E. Lee was even counting on malaria to weaken Union troops, confident that “the climate in June will force the enemy to retire.” (It ended up crippling his own army more.)
Without modern medicine, or any understanding of how the disease spread, people reached for whatever remedies they could find: drinking vinegar and whiskey, rubbing onions on their skin, and boiling bitter herbs into tea. Powdered quinine, a substance derived from cinchona bark, actually worked—but it was expensive and hard to obtain, so few people had access to it.
For most people, the fevers kept returning year after year and summer after summer.
The first breakthrough came at the turn of the 20th century. Scientists finally proved that malaria was transmitted by mosquitoes—not, as had been previously thought, by contaminated water or poor air quality. (Malaria means “bad air” in medieval Italian.) It was a crucial discovery. Finally, people knew what to target. Across the South, some communities began draining swamps to try to control their mosquito populations. But most of these efforts were basic and improvised. What was needed was the kind of massive, coordinated, well-funded approach that only the federal government could mount. Enter one of the most ambitious and impactful infrastructure projects in American history: the Tennessee Valley Authority.
Enter one of the most ambitious and impactful infrastructure projects in American history
the Tennessee Valley Authority.
The TVA wasn’t created to fight malaria. Launched in 1933 as part of the New Deal, its mission was mainly economic: to bring electricity and jobs to the rural South, where some of the country’s poorest people lived, during the Great Depression. But the region also had some of the nation’s highest malaria rates, with 30 percent of its population infected. TVA leaders quickly realized their work wouldn’t succeed unless public health improved too.
So they incorporated malaria prevention into their projects. As engineers built dams and power plants across the region, they also drained thousands of acres of swamps, reshaped rivers, regraded land, and upgraded housing—which all helped to destroy mosquito breeding grounds. At the same time, public health campaigns educated people on installing window screens and eliminating standing water around their homes after storms. Then came World War II.
Then Came
world war II
As military bases popped up across the South, malaria became a growing threat to soldiers and defense industry workers. So the U.S. responded by launching a new program in 1942: the Office of Malaria Control in War Areas, headquartered in Atlanta. It was the federal government’s first centralized program created explicitly to fight malaria—and it laid the groundwork for what would become the Centers for Disease Control and Prevention, or CDC, which officially took over the malaria effort in 1947.
The goal of the campaign, which began with wartime control before transitioning to peacetime eradication, was simple but ambitious: Stop mosquitoes from spreading malaria, and stop people from carrying it.
ON THE MOSQUITO FRONT
The campaign launched the largest insecticide operation in U.S. history and paired it with an aggressive effort to destroy mosquito breeding grounds. Teams of sprayers went door-to-door with tanks of DDT strapped to their backs, covering millions of homes in what was essentially a chemical shield against mosquitoes. In some areas, airplanes dusted entire counties with insecticide. Meanwhile, construction crews drained ditches by hand or with bulldozers. In Florida, they used dynamite to blast open drainage paths from mosquito-infested marshland.
ON THE HUMAN SIDE
Quinine and later chloroquine—its synthetic successor—were distributed widely, especially in rural areas with high infection rates. These drugs cleared the parasite from the bloodstream, which meant that even if someone was bitten by a mosquito, they wouldn’t pass the disease on. Mobile teams traveled from town to town, testing and treating entire communities. In the Mississippi Delta, they even set up roadside treatment stations where people could stop for a dose on the way to work or school.
Public health messaging played a huge role, too. One memorable cartoon featured a mosquito named Bloodthirsty Ann—yes, short for Anopheles—that taught troops how to reduce their risk of contracting malaria. Its creator was a young army captain named Theodor Geisel, who eventually became better known as Dr. Seuss.
Perhaps the most impressive part of the program was its scale and speed. In just a few years, tens of thousands of public health workers across fifteen states were hired and trained. Doctors, nurses, scientists, teachers, technicians, and trusted community figures knocked on doors, gathered data, treated patients, and made sure no outbreak went unchecked. In 1951, America declared victory over malaria.
In 1951
AMERICA DECLARED VICTORY OVER MALARIA
I think about this history a lot when I’m visiting Sub-Saharan Africa, where the parasite still kills 600,000 people a year. Because in many ways, the strategy hasn’t changed: Stop transmission, clear infections, and build public health systems that prevent malaria from roaring back.
Malarious area of the United States
But the U.S. had some key advantages that made elimination much easier. Compared to the species responsible for most malaria today, our mosquitoes weren’t as efficient at transmitting the parasite. Our climate also limited transmission to the summer months; in tropical regions, people get infected year-round. And by the 1940s, our country had relatively strong infrastructure, even in rural areas, that many malaria-endemic countries today still lack.
ON THE TREATMENT SIDE
So the challenge today is much bigger. Fortunately, today’s malaria-fighting toolbox is much bigger—and better—too.
Instead of blanket spraying DDT, which has since been banned, modern prevention relies on safer insecticide-treated bed nets and indoor spraying techniques that use smaller doses of more targeted chemicals. Sugar baits, which lure mosquitoes to ingest a lethal dose of insecticide, are already helping reduce their numbers. And gene drive technology could soon block the parasite inside the mosquito itself—so even if someone gets bitten, they won’t get infected.
Chloroquine has been replaced by artemisinin-based combination therapies, or ACTs, which are more effective and less prone to resistance. New drugs like tafenoquine are helping eliminate recurring strains. Seasonal chemoprevention protects children during peak transmission months. And the first malaria vaccine has been approved, with more on the way.
Malaria elimination is never easy. But unlike a century ago, it’s no longer a mystery. The world knows how to stop this disease. We’ve done it before. And with the right investments and innovations, we can do it again—this time, for everyone.
Bug fix
The buzz stops here
African scientists are engineering mosquitoes that can’t spread malaria.

A genetic cheat code
Moving ahead responsibly

Bite back
Great news for mosquito haters
With some breakthrough tools, the end of malaria could be here soon.

I was scrolling Reddit recently when I saw a video of a mosquito trying and failing to suck someone’s blood. Some of the replies were pretty funny, but I noticed that most of them were just some form of “How do I get this person’s superpower?” It was a great reminder of how universally hated these bloodsuckers are.
But I have good news—for Reddit users and everyone else: Real progress has been made in the fight against mosquitoes and specifically against malaria, the deadliest disease they carry. And I believe we’ll soon have the transformational tools needed to end malaria entirely.
Eradication is a goal Melinda and I set back in 2007, when we stood before a group of global health leaders and called for something many considered impossible: wiping malaria out completely from every country. And until that happened, our goal was—and is—to save as many lives as possible by maximizing the impact of the tools we already have. Eradicating the disease wasn't a new idea; the World Health Organization had made a similar declaration back in 1955. But that earlier campaign, while successful in many wealthier parts of the world, had fallen short across Africa, Asia, the Middle East, Eastern Europe, Central and South America, the Caribbean, and Oceania. Despite half a century of effort, malaria was still infecting up to half a billion people—and claiming a million lives—annually.
Today, the landscape has changed dramatically. In 2022—the last year we have data on—there were 249 million cases worldwide and 608,000 deaths. Those are staggering numbers, but they’re also improvements from where the world was back in 2007. Since then, 17 additional countries have been declared malaria-free by the World Health Organization. Outside of Africa, deaths from the disease have mostly been eliminated.

Just the facts
Health aid saves lives. Don’t cut it.
Here’s the proof I’m showing Congress.

I’ve been working in global health for 25 years—that’s as long as I was the CEO of Microsoft. At this point, I know as much about improving health in poor countries as I do about software.
I’ve spent a quarter-century building teams of experts at the Gates Foundation and visiting low-income countries to see the work. I’ve funded studies about the effectiveness of health aid and pored over the results. I’ve met people who were on the brink of dying of AIDS until American-funded medicines brought them back. And I’ve met heroic health workers and government leaders who made the best possible use of this aid: They saved lives.
The more I’ve learned, the more committed I’ve become. I believe so strongly in the value of global health that I’m dedicating the rest of my life to it, as well as most of the $200 billion the foundation will give away over the next 20 years.
People in global health argue about a lot of things, but here’s one thing everyone agrees on: Health aid saves lives. It has helped cut the number of children who die each year by more than half since 2000. The number used to be more than 9 million a year; now it’s fewer than 5 million. That’s incontrovertible.
So when the United States and other governments suddenly cut their aid budgets the way they've been doing, I know for a fact that more children will die. We’re already seeing the tragic impact of reductions in aid, and we know the number of deaths will continue to rise.
A study in the Lancet looked at the cumulative impact of reductions in American aid. It found that, by 2040, 8 million more children will die before their fifth birthday. To give some context for 8 million: That's how many children live in California, Texas, Florida, New York, Pennsylvania, and Ohio combined.
I’ve submitted written testimony on this topic, which you can read below, for the Senate Appropriations Committee hearing occurring later today. In it, I discuss what’s already happened and what needs to happen next.
Testimony to the United States Senate Committee on Appropriations
June 25, 2025
Over the past 25 years—the same span of time I spent leading Microsoft—I have immersed myself in global health: building knowledge, deepening expertise, and working to save lives from deadly diseases and preventable causes. During that time, I have built teams of world-class scientists and public health experts at the Gates Foundation, studied health systems across continents, and worked in close partnership with national and local leaders to strengthen the delivery of lifesaving care. I have visited hundreds of clinics, listened to frontline health workers, and spoken with people who rely on these programs. Earlier this month, I traveled to Ethiopia and Nigeria, where I witnessed firsthand the impact that recent disruptions to U.S. global health funding are having on lives and communities.
Global health aid saves lives. And when that aid is withdrawn—abruptly and without a plan—lives are lost.
Yet, in recent months, some have questioned whether the foreign assistance pause has caused harm. Concerns about the human impact of these disruptions have been dismissed as overstated. Some people have even claimed that no one is dying as a result.
I wish that were true. But it is not.
It is important to note that while this hearing is about the Trump Administration’s $9 billion recission package, what is really at stake is tens of billions of dollars in critical aid and health research that has been frozen by DOGE with complete disregard for the Congress and its Constitutional power of the purse.
In the early weeks of implementing the foreign aid freeze, DOGE directives resulted in the dismissal of nearly all United States Agency for International Development (USAID) staff and many personnel at the Centers for Disease Control and Prevention (CDC). Some funding was later restored to allow for the continuation of what has been categorized as "lifesaving" programs. However, to date that designation has been applied narrowly and with limited transparency, in an inconsistent manner, often prioritizing emergency interventions when a patient is already in critical condition over essential preventative or supportive care.
For example, providing a child with a preventive antimalarial treatment, ensuring access to nutrition so that HIV/AIDS medications can be properly administered, testing pregnant women for HIV to see if they are eligible for treatment to prevent transmission to their children or identifying and treating tuberculosis cases early have not consistently qualified for exemption. As a result, many of the programs delivering these services have been suspended, delayed, or scaled back.
Recent reporting from the New York Times has shed light on the devastating human cost of the abrupt aid cuts. One especially tragic example is Peter Donde, a 10-year-old orphan in South Sudan, born with HIV, who died in February after losing his access to life-saving medication when USAID operations were suspended. His story is one of many.
During my recent visit to Nigeria, I met with leaders from local nonprofit organizations previously funded by the United States. One group shared the remarkable progress they had made in tuberculosis detection and treatment. In just a few years, case identification increased from 25 percent to 80 percent, a critical step toward breaking transmission and reducing the overall disease burden. That progress has now stalled. The grants that enabled this work were tied to USAID staff who have been dismissed, and with their departure, the funding ended, and the work stopped.
The broader effects of these sudden shifts are difficult to overstate. For example, funding for polio eradication has been preserved in the State Department budget but cut from the CDC—even though the two agencies collaborate closely on the program. This type of fragmented decision-making has left implementing organizations uncertain about staffing and operations. Many no longer feel confident that promised U.S. funds will materialize, even when awards have been announced. In some cases, staff continue to work without pay. Some organizations are approaching insolvency.
Meanwhile, in warehouses across the globe, food aid and medical supplies sourced from American producers are sitting idle—spoiling or approaching expiration—because the systems that once distributed them have been disrupted. Clinics are closing. Health workers are being laid off. HIV/AIDS patients are missing critical doses of medication. Malaria prevention campaigns, including bed net distributions and indoor spraying, have been delayed or canceled, leaving hundreds of millions of people unprotected at the peak of transmission season.
Efforts to track data that would illustrate the severity of this worsening crisis have also been severely compromised. Many of the people responsible for collecting and reporting health information—health workers, statisticians, and program managers—have been laid off or placed on leave. The systems that once monitored health outcomes are shutting down, and the offices where that data was once analyzed now sit empty. As a result, the true scope of the harm is becoming harder to measure, just as the need for information is most urgent.
The situation we face is not about political ideology, and it is not a debate over fiscal responsibility. U.S. government spending on global health accounts for just 0.2 percent of the federal budget. Shutting down USAID did nothing to reduce the deficit. In fact, the deficit has grown in the months since.
Furthermore, many of the allegations regarding waste, fraud, and abuse have proven to be unsubstantiated. For example, the widely circulated claim that USAID sent millions of dollars’ worth of condoms to the Gaza Strip is inaccurate. In fact, the Wall Street Journal reported that the program allocated approximately $27,000 for condoms as part of an HIV transmission prevention initiative—not in the Middle East, but in Gaza Province, Mozambique.
What we are witnessing because of the rapid dismantling of America’s global health infrastructure is a preventable, human-caused humanitarian crisis—one that is growing more severe by the day. DOGE made a deadly mistake by cutting health aid and laying off so many people. But it is not too late to undo some of the damage.
A Record of Progress—and What is at Risk
Since 2000, child mortality worldwide has been cut in half. Deaths from HIV/AIDS, tuberculosis, and malaria have declined significantly. And we are on the verge of eradicating only the second human disease in history: polio. These are not abstract statistics; they represent tens of millions of lives saved. None of this progress would have been possible without consistent, bipartisan U.S. leadership and investment.
Over the past several decades, the United States has built one of its most strategic global assets: a respected and robust public health presence. This leadership is not just a humanitarian achievement—it is a core pillar of American soft power and security. For example, a Stanford study analyzing 258 global surveys across 45 countries found that U.S. health aid is strongly linked to improved public opinion of the United States. In countries and years where U.S. health aid was highest, the probability of people having a very favorable view of the United States was 19 percentage points higher. Other forms of aid—like military or governance—did not have the same effect. Another example is the 2014 Ebola outbreak in West Africa. The rapid deployment of U.S. scientists, health workers, and CDC teams helped contain the virus before it could spread globally. Their presence allowed the U.S. to help shape the response strategy, speed up containment, and prevent a wider outbreak. Many African countries are facing the dual burden of rising debt and pressing health needs, forcing painful choices between repaying creditors, and protecting their citizens. Helping them navigate this challenge is not just the right thing to do—it is a strategic imperative. If the United States retreats, others will fill the gap, and not all of them will bring our values, our priorities, or our interests to the table. Preserving American global influence will require restoring the staff, systems, and resources that underpin it—before the damage becomes irreversible.
I understand the fiscal pressures facing Congress. I recognize the need to prioritize spending and to hold programs accountable for results. I also share the Trump Administration’s commitment to promoting efficiency and encouraging country-led solutions. But I believe those goals can—and must—be pursued while still protecting the programs that deliver the highest return on investment and the greatest impact on human lives.
The United States’ support for Gavi, the Vaccine Alliance; the Global Fund to Fight AIDS, Tuberculosis, and Malaria; the President’s Emergency Plan for AIDS Relief (PEPFAR); and the Global Polio Eradication Initiative (GPEI) represent some of the smartest, most effective investments our country has ever made. These initiatives are proven, strategically aligned with American interests, and cost-effective on a scale few other government programs can match.
Together, Gavi and the Global Fund have helped save more than 82 million lives. Gavi has helped halve childhood deaths in the world’s poorest countries and returns an estimated $54 for every $1 invested. The Global Fund has contributed to a 61% reduction in deaths from HIV/AIDS, TB, and malaria. PEPFAR has saved over 26 million lives and helped millions of children be born HIV-free. GPEI has brought us closer than ever to the eradication of polio. Pulling back now would not only jeopardize these historic gains—it would invite a resurgence of preventable disease, deepen global instability, and undermine decades of bipartisan American leadership.
This is not a forever funding stream for the U.S. Government. These programs set out clear pathways for countries to “graduate” from aid, which many have already done. For example, nineteen countries, including Viet Nam and Indonesia, have successfully graduated from Gavi support and now fully finance their own immunization programs. Others—from Bangladesh to Cote d'Ivoire—are on track to do the same. This is how U.S. development policy should work: catalytic, cost effective, and designed to help countries become self-reliant and drive their own progress. I agree that aid funding should have an end date, but not overnight. The most effective path to that end date is innovation. By investing in the development and delivery of new medical tools and treatments, we can drive down the cost of care, and in some cases, make diseases that were once a death sentence treatable, or even curable. Advances in therapies for chronic conditions like sickle cell disease, HIV, or certain types of cancers could transform lives and health systems. American innovation offers a sustainable exit strategy—one that reduces long-term costs, allows the United States to responsibly step back, and builds lasting trust and good will that far exceed the original investment.
Over the past 25 years, the Gates Foundation has invested nearly $16 billion in global health partnerships like Gavi, the Global Fund, and GPEI. We will continue to invest, through innovation, research, and close coordination with partners. But no private institution—or coalition of them—can replace the scale, reach, or authority of the U.S. government in delivering lifesaving impact at the global level.
The decisions made in the coming weeks will shape not only the lives saved in the near term—but the legacy of American leadership for generations to come.
Download a PDF of the testimony with appendices that include reflections from Gates Foundation staff in Africa on the impact of the U.S. aid cuts; analytical projections from respected organizations; and a selection of first-hand reporting from reputable news organizations and journalists.

No laughing matter
A gut-wrenching problem we can solve
Diarrhea used to be one of the biggest killers of kids—but now it’s one of the greatest global health success stories.

In 1997, I came across a New York Times column by Nick Kristof that stopped me in my tracks. The headline was “For Third World, Water Is Still a Deadly Drink,” and it included a statistic I almost didn’t believe: Diarrhea was killing 3.1 million people every year—most of them kids under the age of five.
I didn’t know much about the problem back then, except that it seemed so solvable. After all, in rich countries it felt like it already had been. My oldest daughter was a toddler at the time, and we never worried that an upset stomach would kill her. None of the other parents I knew worried about that either.
But in much of the world, kids without clean drinking water or basic sanitation were constantly being exposed to rotavirus, cholera, shigella, typhoid, and more—dangerous pathogens that spread easily when toilets are scarce and water is contaminated.
Nick’s column ended up changing my life. I sent it to my dad with a note: “Maybe we can do something about this.” He agreed. And after he traveled to Bangladesh to see the problem firsthand, we made a $40 million investment in vaccine research for diarrheal diseases. That grant helped shape what would become the Gates Foundation—and kickstarted decades of progress that’s now saved millions of lives.
Within a few years, I stepped away from Microsoft to focus on this work full-time. Once you’ve seen what’s possible in global health, it’s hard to do anything else.
When we first got involved, diarrhea was one of the biggest killers of kids worldwide. But over the past two and a half decades, these deaths have dropped by more than 70 percent.
The biggest breakthrough came from making vaccines for rotavirus, the leading cause of severe diarrhea and death in kids, affordable and accessible. When the vaccines first debuted in the early 2000s, they were priced at around $200 per dose—which meant they were completely out of reach for most families in most of the world. So the foundation partnered with vaccine manufacturers in India like Bharat Biotech and Serum Institute to develop high-quality, low-cost alternatives. Today, rotavirus protection costs about a dollar.
But getting the vaccines developed was only half the challenge. The other half was getting them to the kids who needed them most.
That’s where Gavi came in. The organization was set up a few years earlier to help low-income countries pay for lifesaving vaccines that had existed for decades but weren’t reaching the world’s poorest. But they were well-positioned to do the same with a new vaccine, and they did—purchasing the rotavirus vaccine for millions of children and supporting countries as they added it to their routine immunization programs. USAID played a huge role in this work, too, by helping local governments train community health workers and strengthen their vaccine delivery systems. Meanwhile, public health campaigns promoted treatments like oral rehydration salts and zinc supplements that can save a sick child's life for pennies. (Think of it as the medical-grade equivalent of Pedialyte.)
As all this was happening, countries quietly made enormous progress on clean water and sanitation too. Since 1990, 2.6 billion people around the world have gained access to safe drinking water—and the number of people who now have basic sanitation similarly has skyrocketed. These improvements help break a cycle where kids get sick, recover, and then get reinfected a few weeks later.
Despite the incredible progress, around 340,000 kids under five are still dying from diarrhea each year.
Part of the problem is that many kids still don't get vaccinated. Some live in places where health systems are weak or vaccines are hard to transport and store. Others are caught in conflict zones that make it dangerous for health workers to reach them.
And new challenges make the fight against diarrheal diseases even harder than it was 25 years ago. Shigella—one of the nastiest bacterial causes of diarrhea—is becoming more and more resistant to antibiotics, and we still don't have a vaccine. Climate change is making cholera and typhoid outbreaks more frequent, as floods contaminate water supplies and droughts force people to drink from unclean, unsafe sources.
For malnourished kids, everything is harder: They're more vulnerable to diarrheal diseases in the first place, and their damaged digestive tracts don't respond as well to oral vaccines or treatments. For families barely scraping by, diarrhea is both a medical crisis and an economic disaster. Parents miss work to care for sick kids. Kids miss school. Expenses pile up. It's one of the ways that disease keeps families trapped in poverty—and one of the reasons that a country’s public health is key to its development.
The encouraging news is that there’s a promising pipeline of innovations that builds on what we already know and could save even more lives.
At the foundation, we’re supporting scientists who are working on a vaccine for Shigella, which has become the leading bacterial cause of childhood diarrhea. We’re also funding efforts to combine different vaccines into a single shot, which would lower costs and make things easier for health workers and kids alike.
New delivery methods could make a big difference too. One example: vaccine patches for measles that don’t require needles, refrigeration, or trained staff to administer them. Just peel, stick, and protect.
We've already learned a lot about how chronic infections damage kids’ guts and make it harder for them to absorb nutrients or respond to vaccines. Now, scientists are researching how to repair that damage, which could help the sickest kids recover faster.
And outside the lab, environmental monitoring tools are being developed to detect early signs of outbreaks—by regularly testing sewage for typhoid, for instance. It’s like having an early warning system for epidemics.
We can’t afford to look away now
I’ve been talking about diarrhea for 25 years, even though it makes some people squeamish, because it’s a microcosm of global health. It’s proof that the world can come together to solve big problems. When we refuse to accept that some children won’t make it to their fifth birthday, we can save millions of lives.
But it’s also a warning of what can happen when we look away.
Right now, global health funding is being slashed around the world. According to one estimate, cuts to aid from the U.S. have already led to almost 60,000 additional childhood deaths from diarrhea. If nothing changes, by next January that number could rise to 126,000. These are projections, not final counts, but the reality is undeniable: When lifesaving programs are eliminated, kids pay the price.
Diarrhea is one of the most solvable problems in global health. We’ve come a long way, but we’re not done yet.
Lung Story Short
A book about tuberculosis, and everything else
Here’s how John Green turned a forgotten disease into a #1 NYT bestseller.

What do Adirondack chairs, Stetson hats, the city of Pasadena, and World War I have in common? According to John Green, all of their origin stories include tuberculosis.
In his new book, John argues that it’s impossible to separate the deadliest disease in history from, well, the rest of history. Adirondack chairs were designed by a man who vacationed in the New York mountains—a popular spot for TB patients seeking fresh air—and soon became staples of sanatorium porches across the country. John B. Stetson, who had TB himself, traveled west for dry mountain air and invented the cowboy hat to protect from sun, wind, and rain. Pasadena became a hub for TB treatment in the late 1800s, and TB “tourism” was a major driver of the city’s early economy, real estate, and identity. And the teenage assassins who killed Archduke Franz Ferdinand, which kicked off World War I? They were more willing to die for their cause since they were already dying of TB.
No wonder John calls this book Everything Is Tuberculosis. In so many ways, TB shaped the world we live in. Even though the disease is now both rare and treatable in rich countries, in poorer places it’s on the rise and still a death sentence for so many.
John is best known as the author of some of the best young adult novels of all time (at least according to my daughter Phoebe, whose encouragement led me to read The Fault in Our Stars and Turtles All the Way Down). So a lot of people were surprised when he announced that his next book would be about global health—about a disease most people in the western world think of in the past tense.
I wasn’t. After all, I first met John over a decade ago, when he joined me on a Gates Foundation trip to Ethiopia. While traveling, we talked about a lot of the big questions John wrestles with in Everything Is Tuberculosis—like why the place a person is born influences their odds of surviving childhood (or childbirth), and what people like us can do to increase those odds.
Since then, John has been an invaluable partner to the foundation, bringing his curiosity and clarity to our events and helping raise awareness of our work. But he’s also become a powerful advocate for global health in his own right. I don’t know anyone else who could turn a book about tuberculosis into a number one New York Times bestseller.
Everything Is Tuberculosis is poignant, smart, and at times infuriating. At its heart is the story of a boy named Henry, whom John met at a TB clinic in Sierra Leone. Henry was just six when he started showing classic signs of the disease: fatigue, weight loss, night sweats. But the first tests he got came back negative, so he was sent home from the hospital. By the time he was eventually diagnosed, Henry was already very sick.
He began treatment with the standard cocktail of decades-old antibiotics. It’s a brutal regimen that involves months of pills, painful injections, constant side effects—and, once the infection starts to subside, aching hunger from having an appetite again. The drugs only work if they’re taken consistently and on schedule, but that’s often unrealistic for patients. In much of the world, TB treatment means walking miles to a clinic, missing work or school, going into debt, and facing social stigma and isolation. Even though Henry’s mom did everything she could to support him, there were interruptions to his treatment, and eventually the TB became drug-resistant.
In the end, Henry got lucky. Even as he got sicker and ran out of options, his doctors wouldn’t give up on him. They fought to get him access to a personalized drug regimen—something that’s rarely available to kids in poor countries. That care ended up saving his life, and today Henry is thriving. After years stuck in the hospital, he’s caught up academically and now in university (and even has a YouTube channel where he shares his journey and advocates for other TB patients). John doesn’t romanticize Henry’s story as some kind of miracle. Instead, he uses it as proof: that TB is curable, that good care works, and that the real question isn’t whether we can save lives—but whether we’re willing to make that care available to everyone.
Even though John finished writing the book last year, he nails the urgency of this moment. He shows how a disease that most people in rich countries have forgotten is still killing over a million people a year, and how easily that number could keep climbing. That’s especially true now, as foreign aid cuts disrupt TB care across the globe. Henry might not be alive today if it weren’t for organizations like Partners In Health—funded in part by U.S. health aid—which fought to get him the treatment he needed. These aid cuts will be devastating for kids like him, who may lose access to treatment altogether. They’ll also lead to more interrupted care, more cases, more drug resistance, and more strains of an infectious disease that will be harder and more expensive for the entire world to contain.
This is a book about the central challenge of global health today: the reality that, in John’s words, “the cure is where the disease is not, and the disease is where the cure is not.”
A book about tuberculosis could be pretty boring, but John makes it super compelling by weaving in TB’s long and strange history, from the myth that it only afflicted white people, to the theory that it inspired creative genius, to its influence on Victorian beauty standards. (I didn’t know about those last two… or the Stetson hats.) If you’re familiar with John’s work, this approach won’t surprise you. He has a gift for getting people to care about things they might not think are “for me,” whether that’s poetry, astrophysics, or infectious disease.
John ends Everything Is Tuberculosis with a stirring call to action. He makes the case that saving lives from TB isn’t really a scientific challenge anymore; it’s a moral one. I largely agree. But I also think there are more reasons for hope than the book lets on.
While John is clear-eyed about the failures of the past and present—the slow pace of progress, the sky-high prices of new TB drugs, the inequality that determines who gets treated and who doesn’t—he doesn’t spend much time on what comes next. Having spent the last two-and-a-half decades investing in the science behind TB care through the Gates Foundation, I’ve seen a different side of the story. I know what’s in the pipeline, and I know what’s possible.
Today, we’re closer than ever to breakthroughs that could change everything about how we treat and even prevent TB: shorter drug regimens, better diagnostics, and even vaccines. These tools will only make a difference if they’re affordable enough to reach kids like Henry. But I think it’s important to recognize that the companies often criticized for pricing are also, ironically, the only ones that have been willing to invest in TB at all. We need to keep working with them as partners, keep the innovation coming, and keep bringing costs down.
If we do, we can make Henry’s story of survival the norm, not the exception—and make tuberculosis a disease of the past, not the future.
Such great heights
This heroic nurse climbs 1000-foot ladders to save lives
Agnes Nambozo goes to extraordinary lengths to vaccinate children in Uganda.

How do you get to work? Some people roll out of bed and move 10 feet to their desk. Others walk to the office or take public transit. I usually drive a car.
No matter how you get there, I guarantee that your commute isn’t as wild as Agnes Nambozo’s: She regularly climbs a rickety ladder that is nearly 1,000 feet tall—or 300 meters—before she can start work for the day.
Agnes is a nurse based in Buluganya, located in the shadow of Mount Elgon in eastern Uganda. Like many nurses in rural communities across sub-Saharan Africa, she wears a lot of different hats. She might spend one day delivering babies and treating wounds and the next as a health educator, promoting good nutrition and sanitation in her community. The days Agnes believes she makes the biggest difference, though, are the ones when she treks deep into the Ugandan countryside to vaccinate children.
Uganda has done an amazing job of reducing childhood mortality over the last 25 years. In 2000, about 145 children died per every thousand live births. By 2023, that figure had dropped to fewer than 40 deaths per 1,000 births. A lot of that progress can be attributed to vaccines and vaccinators like Agnes.
Eastern Uganda is a gorgeous place, but parts of it are incredibly difficult to cross. Many of the communities Agnes visits are high in the mountains. Some are only accessible by ladders, which act as links between communities. Older children can climb down them to go to school, but they are too steep for the little ones. Mothers can’t safely carry their babies down the ladders to the health clinic, so Agnes comes to them.
When Agnes was a little girl, she wanted to be a police officer—until her mom convinced her the job was too dangerous. Instead, she took a nursing course. She fell in love with the profession, even though it ended up being a much riskier job than her mom ever imagined. She travels to the villages to vaccinate kids in all kinds of weather. It’s often rainy in the mountains, and the ladders become slippery. “The ladders are risky because you might miss a step,” she says. “If you are lucky, you can get a fracture. If you’re not lucky, you can lose your life.”
On the days when she heads into the field to vaccinate children, Agnes leaves her house by 6:00 am. She takes a taxi from where she lives in Sironko to Buyaga, a town closer to where the health clinic is located. Cars can’t drive on the road to the clinic, so she takes a motorbike for the last stretch.
She arrives at the clinic around 8:00 am and starts packing for the day. Rural vaccinators like Agnes must carry their supplies on their backs, and there’s an art to making sure everything is loaded properly. The vaccines must be kept cold so she wears a heavy insulated backpack stuffed with ice packs.
Agnes then hops on another motorbike to a staging location before heading off on foot to the ladders. By the time she reaches the village and starts setting up to immunize the community, it’s usually around 10:30—more than four hours after she left her house for the day.
She comes in with a plan for how many people she’ll vaccinate, but Agnes always brings a couple extra doses just in case. A typical day usually means around 50 patients. Most are children under 5, who get vaccinated against deadly diseases like polio, measles, tetanus, and pneumonia. The latter is especially important in a region as rainy as this one, where the damp weather makes people more susceptible to respiratory diseases.
Agnes and her colleagues are often the only health workers who visit the most remote communities in the mountains, so they also provide general nursing care while they’re there. Agnes regularly gives kids deworming treatments and key supplements like vitamin A. She answers questions from the adults and offers them health guidance, including advice on planning a family.
After she wraps up for the day, Agnes makes the long trek back home. It’s exhausting, difficult work, but she is proud to help so many people. “Our motto for nurses in Uganda is ‘To love and serve,’” she says. “And to me, love is not just a word. It’s a verb.”
Unfortunately, Agnes’s job recently became a lot more difficult. Many of her colleagues at the health clinic in Buluganya were supported by USAID, and they lost their jobs when funding was cut. Some of the positions that were eliminated supported new and expectant mothers. Others worked on HIV and tuberculosis, distributing medication and testing high-risk individuals to prevent further spread.
Agnes and the others who are left are doing their best to ensure communities still receive care, but they can only do so much. “Our community is suffering a lot,” she says. She is worried about burnout if funding isn’t restored.
Still, Agnes won’t rest until she has helped as many people as she can. Thanks to the support of the Rotary Club of Kampala, she recently went back to school and is working towards a degree in nursing. She hopes to learn new skills that will save even more lives.
“My dream is to make people feel good, to make them happy, and to give my service to the people,” says Agnes. “When you have positivity, nothing is impossible.”

Everyday miracles
A perilous time for the world’s poorest children
My latest speech about why we need to keep funding vaccines.

I’ve been giving speeches about vaccines for 25 years. After so much time, it could have become routine for me. But it never has.
One reason is that the impact of vaccines—a single dose can protect a child from deadly diseases forever—is like a miracle to me, and who gets tired of talking about miracles?
The other reason is tied to this particular moment. There’s never been a point in the past 25 years when more lives hung in the balance. In all likelihood, 2025 will be the first year since the turn of the century when the number of children dying will go up instead of down.
Why? Governments are cutting health aid—including funds for Gavi, the vaccine organization that the Gates Foundation helped start. As a result, Gavi will likely not have all the money it needs to fund its next five years of work.
So when I spoke this week at a summit in Brussels where donors committed a new round of funding for Gavi, I focused on why it’s so important to keep the money flowing and maintain our momentum on vaccines. You can read my remarks below.
Remarks as delivered
June 25, 2025
Global Summit: Health & Prosperity through Immunisation
Brussels, Belgium
Good evening, and thank you to everyone joining us here tonight—and for all your support for one of the most transformative efforts in the world.
I want to particularly thank President von der Leyen and President Costa, and the European Union, for co-hosting this summit. President von der Leyen has long been an incredible champion for health and development, and the EU has been one of the Gavi's biggest supporters since the very beginning—support that's more crucial now than ever.
This chart is one that I think about a lot. It's really my most favorite chart. And I consider it almost kind of a report card for humanity. Because over the last 25 years, the reduction of under-five deaths has been far faster than any time in history. We've gone from over 9 million to now half as many deaths taking place by children. This is an unbelievable result.
And it doesn't fully state the benefit of these vaccines. The vaccines leave a lot of kids far more healthy, and so their ability to achieve their potential is increased.
Gavi prioritizes saving lives, and it's done with incredible scientific rigor. We're constantly improving vaccines. We're constantly looking at the safety, and I'm very proud of the work that's done to make sure that these vaccines are incredibly safe.
The founding of Gavi actually goes back to about the time the Gates Foundation was first started. And after 25 years, I can still say that it's at the top of the list of things that I'm very, very proud of. At that time, kids were not getting access to vaccines. They were too expensive. They hadn't been formulated properly. And I was stunned to learn that so many kids were dying from a disease like rotavirus because the vaccine wasn't getting out to all the children of the world.
So Gavi was created to not only help finance vaccines, but work with countries to adopt these new vaccines.
We've done an amazing job of getting these prices down. A good example is the pneumococcal vaccine, PCV. This vaccine became available in high-income countries the year that Gavi was founded. And it does a fantastic job of protecting kids against pneumonia, which was the single most deadly childhood infection. But it was very expensive.
And so Gavi and its partners incentivized vaccine manufacturers to develop a new, much cheaper PCV, which was introduced in 2017. Today, the manufacturers make PCV vaccines available to low-and middle-income countries for just $2 a dose.
And of course, we've seen similar reductions across all of the different vaccines, allowing us to add new vaccines to save even more children.
Since the founding of Gavi, the overall cost of fully vaccinating a child has been cut in more than half.
And we have a pipeline of new vaccines coming along, vaccines to address new diseases and that bring down costs even further.
A good example of this is the HPV vaccine. Cervical cancer, which HPV prevents, is the fourth most common cancer in women around the world. And this vaccine can prevent over 90% of these cases.
But countries were slow to adopt this vaccine, in part because it was hard to deliver: initially, it required three doses spread across six months.
Scientists believed that perhaps it could be done with fewer doses. And so the Gates Foundation funded a trial to see whether a single dose was essentially fully protective. And after seeing the incredible results, the WHO approved a single dose schedule in 2022.
Now, we have 75 countries around the world that have moved to this single dose approach.
And because the single dose is cheaper and easier to deliver, it's now getting to far more girls around the world. For example, after Nigeria introduced the single-dose vaccine, it was able to vaccinate more than 12 million girls in less than a year. That's really incredible.
Across Gavi countries, HPV vaccine coverage has increased dramatically. The year after this single-dose approval, we doubled the number of girls getting the vaccine. And [the next year] we doubled it again, and this year we'll double it again.
There's more than just making vaccines available. We have to work with our partner countries on helping improve their health systems. So the Gavi Alliance has spent a lot of its resources and a lot of its technical support in helping improve those primary health care systems, which are so vital. We've helped countries understand where they're missing kids and how to invest in raising those coverage levels.
As you've heard, over this 25-year period, that means over a billion children have been vaccinated—resulting in the saving of over 19 million lives.
Nineteen million is a big number. It's almost easier to understand if I just say: okay, here's a child whose life was saved. But you have to take your reaction to how valuable that is and multiply it by this absolutely gigantic number.
The total cost to save those lives was about $22 billion. And that means that Gavi saved children's lives for only about $1,000 per life saved.
And in addition, the kids who these vaccines have kept healthy not only go to school; they do well in school. They join the economy. They contribute to their country. And really, this is why improving health through vaccines is part of the formula for helping countries be self-sufficient.
Gavi's vaccination has generated $250 billion in economic benefits in the countries it supports. In fact, Gavi has had such an extraordinary economic benefit that over 19 countries that were Gavi recipients have now graduated, meaning they now fully fund their own immunization programs.
A great example is Indonesia. Since partnering with Gavi, it’s doubled the number of vaccines offered through its routine immunization program—and it’s seen childhood deaths fall to a quarter of what they were before. And now, Indonesia is not only transitioning to be fully self-supportive—it’s also become a Gavi donor.
Of course, this is a challenging time. All the progress we’ve made is at risk. Budgets are tight, and we all have to show our priorities when there’s tough trade-offs to be made.
There’s no denying: this is a global health crisis. Between the U.S. cuts and other funding cuts, in total, aid in total has gone down by 30 billion this year alone. It reinforces the incredible values being shown by the people who are showing up here today and being incredibly generous.
But with the cut in health resources, along with the financial situation a lot of these low-income countries are in, we are going to have a few years where things will go backwards.
As we think about this, think of a mother who will bring a baby wheezing for breath to a help center, and because the vaccines aren't available, that baby will not survive.
Think of a health worker trying to deal with a measles outbreak who, because there's less resources for that primary health care system or vaccines, that measles epidemic will continue.
This is agonizing. I mean, we have to put ourselves in the position of the parents who lose these children and how tough it must be for them to realize that the life could have been saved by a vaccine that costs just 30 cents.
So though our trend lines will briefly go into reverse, I believe that we can come back. I believe that we will resume that incredible progress that you saw.
I don't know if it'll be in two years or four years or six years, but I do know that as we bring these resources back, and we take advantage of an incredible pipeline of innovation, new drugs, new vaccines—lots of amazing things to help with these diseases—we will resume progress.
So everyone here, I'd say, is recommitting themselves, just like the Gates Foundation, to doubling down and staying committed.
You know, I'm not pessimistic. In fact, we have things like polio eradication that we are, as we say, this close to elimination. That'll be a mind-blowing thing. Likewise, malaria: we have tools, a variety of tools that brought together will give us a chance in the next 20 years to completely eradicate that as a disease, just like we're doing with polio.
This is all why the Gates Foundation is pledging $1. 6 billion to Gavi for this next five-year period. Thank you.
And it's why we'll invest billions in making sure that pipeline of new and lower-cost vaccines continues to make Gavi even more effective.
In closing, I think we can reflect on what Nelson Mandela once said: “There can be no keener revelation of a society's soul than the way it treats its children.”
In the last 25 years, Gavi has helped over a billion children live better, healthier lives—thanks to the extraordinary support of partners like you.
If we get this right, this trajectory of progress will continue for decades to come.
Thank you.
The last chapter
My new deadline: 20 years to give away virtually all my wealth
During the first 25 years of the Gates Foundation, we gave away more than $100 billion. Over the next two decades, we will double our giving.

When I first began thinking about how to give away my wealth, I did what I always do when I start a new project: I read a lot of books. I read books about great philanthropists and their foundations to inform my decisions about how exactly to give back. And I read books about global health to help me better understand the problems I wanted to solve.
One of the best things I read was an 1889 essay by Andrew Carnegie called The Gospel of Wealth. It makes the case that the wealthy have a responsibility to return their resources to society, a radical idea at the time that laid the groundwork for philanthropy as we know it today.
In the essay’s most famous line, Carnegie argues that “the man who dies thus rich dies disgraced.” I have spent a lot of time thinking about that quote lately. People will say a lot of things about me when I die, but I am determined that "he died rich" will not be one of them. There are too many urgent problems to solve for me to hold onto resources that could be used to help people.
That is why I have decided to give my money back to society much faster than I had originally planned. I will give away virtually all my wealth through the Gates Foundation over the next 20 years to the cause of saving and improving lives around the world. And on December 31, 2045, the foundation will close its doors permanently.
This is a change from our original plans. When Melinda and I started the Gates Foundation in 2000, we included a clause in the foundation’s very first charter: The organization would sunset several decades after our deaths. A few years ago, I began to rethink that approach. More recently, with the input from our board, I now believe we can achieve the foundation’s goals on a shorter timeline, especially if we double down on key investments and provide more certainty to our partners.
During the first 25 years of the Gates Foundation—powered in part by the generosity of Warren Buffett—we gave away more than $100 billion. Over the next two decades, we will double our giving. The exact amount will depend on the markets and inflation, but I expect the foundation will spend more than $200 billion between now and 2045. This figure includes the balance of the endowment and my future contributions.
This decision comes at a moment of reflection for me. In addition to celebrating the foundation’s 25th anniversary, this year also marks several other milestones: It would have been the year my dad, who helped me start the foundation, turned 100; Microsoft is turning 50; and I turn 70 in October.
This means that I have officially reached an age when many people are retired. While I respect anyone’s decision to spend their days playing pickleball, that life isn’t quite for me—at least not full time. I’m lucky to wake up every day energized to go to work. And I look forward to filling my days with strategy reviews, meetings with partners, and learning trips for as long as I can.
The Gates Foundation’s mission remains rooted in the idea that where you are born should not determine your opportunities. I am excited to see how our next chapter continues to move the world closer to a future where everyone everywhere has the chance to live a healthy and productive life.
Planning for the next 20 years
I am deeply proud of what we have accomplished in our first 25 years.
We were central to the creation of Gavi and the Global Fund, both of which transformed the way the world procures and delivers lifesaving tools like vaccines and anti-retrovirals. Together, these two groups have saved more than 80 million lives so far. Along with Rotary International, we have been a key partner in reviving the effort to eradicate polio. We supported the creation of a new vaccine for rotavirus that has helped reduce the number of children who die from diarrhea each year by 75 percent. Every step of the way, we brought together other foundations, non-profits, governments, multilateral agencies, and the private sector as partners to solve big problems—as we will continue to do for the next twenty years.
Over the next twenty years, the Gates Foundation will aim to save and improve as many lives as possible. By accelerating our giving, my hope is we can put the world on a path to ending preventable deaths of moms and babies and lifting millions of people out of poverty. I believe we can leave the next generation better off and better prepared to fight the next set of challenges.
The work of making the world better is and always has been a group effort. I am proud of everything the foundation accomplished during its first 25 years, but I also know that none of it would have been possible without fantastic partners.
Progress depends on so many people around the globe: Brilliant scientists who discover new breakthroughs. Private companies that step up to develop life-saving tools and medicines. Other philanthropists whose generosity fuels progress. Healthcare workers who make sure innovations get to the people who need them. Governments, nonprofits, and multilateral organizations that build new systems to bring solutions to scale. Each part plays an essential role in driving the world forward, and it is an honor to support their efforts.
Of course, although the Gates Foundation is by far the most significant piece of my giving, it is not the only way I give back. I have invested considerable time and money into both energy innovation and Alzheimer’s R&D. Today’s announcement does not change my approach to those areas.
Expanding access to affordable energy is essential to building a future where every person can both survive and thrive. The bulk of my spending in this area is through Breakthrough Energy, which invests in companies with promising ideas to generate more energy while reducing emissions. I also started a company called TerraPower to bring safe, clean, next-generation nuclear technology to life. Both of these ventures will earn profits if successful, and I will reinvest any money I make through them back in the foundation, as I already do today.
I support a number of efforts to fight Alzheimer’s disease and other related dementias. Alzheimer’s is a growing crisis here in the United States, and as life expectancies go up, it threatens to become a massive burden to both families and healthcare systems around the world. Fortunately, scientists are currently making amazing progress to slow and even stop the progress of this disease. I expect to keep supporting their efforts as long as it’s necessary.
The success in both areas will determine exactly how much money is given to the foundation since any profits they earn will be part of my overall gift.
What the Gates Foundation hopes to accomplish
Over the next twenty years, the foundation will work together with our partners to make as much progress towards our vision of a more equitable world as possible.
The truth is, there have never been more opportunities to help people live healthier, more prosperous lives. Advances in technology are happening faster than ever, especially with artificial intelligence on the rise. Even with all the challenges that the world faces, I’m optimistic about our ability to make progress—because each breakthrough is yet another chance to make someone’s life better.
Over the next twenty years, the foundation’s funding will be guided by three key aspirations:
In 1990, 12 million children under the age of 5 died. By 2019, that number had fallen to 5 million. I believe the world possesses the knowledge to cut that figure in half again and get even closer to ending all preventable child deaths.
We now understand the essential role nutrition—and especially the gut microbiome—plays in not only helping kids survive but thrive. We’ve made huge advances in maternal health, making sure that new and expectant mothers have the support they need to deliver healthy babies. We have new, life-saving vaccines and medicines, and we know how to get them to the people who need them most thanks to organizations like Gavi and the Global Fund. The innovation is there, the ability to measure progress is stronger than ever, and the world has the tools it needs to put all children on a good path.
Today, the list of human diseases the world has eradicated has just one entry: smallpox. Within the next couple years, I expect to add polio and Guinea worm to the list. (When we eradicate the latter, it will be a testament to the late President Jimmy Carter’s leadership.) I’m optimistic that, by the time the foundation shuts down, we can also add malaria and measles. Malaria is particularly tricky, but we’ve got lots of new tools in the pipeline, including ways of reducing mosquito populations. That is probably the key tool that, as it gets perfected and approved and rolled out, gives us a chance to eradicate malaria.
In 2000, the year that we started the foundation, 1.8 million people died from HIV/AIDS. By 2023, advances in treatment and preventatives cut that number to 630,000. I believe that figure will be reduced dramatically in the decades ahead, thanks to incredible new innovations in the pipeline—including a single-shot gene therapy that could reduce the amount of virus in your body so much that it effectively cures you. This would be massively beneficial to anybody who has HIV, including in the rich world. The same technology is also being used to treat sickle cell disease, an excruciating and deadly illness.
We’re also making huge progress on tuberculosis, which still kills more people than malaria and HIV/AIDS combined. Last year, a historic phase 3 trial began that could be the first new TB vaccine in over 100 years.
The key to maximizing the impacts of these innovations will be lowering their costs to make them affordable everywhere, and I expect the Gates Foundation will play a big role in making that happen. Health inequities are the reason the Gates Foundation exists. And the true test of our success will be whether we can ensure these life-saving interventions reach the people who need them most—particularly in Africa, South Asia, and across the Global South.
To reach their full potential, people need access to opportunity. That’s why our foundation focuses on more than just health.
Education is key. Frustratingly, progress in education is less dramatic than in health—there is no vaccine to improve the school system—but improving education remains our foundation’s top priority in the United States. Our focus is on helping public schools ensure that all students can get ahead—especially those who typically face the greatest barriers, including Black and Latino students, and children from low-income backgrounds. At the K-12 level, that means boosting math instruction and ensuring teachers have the training and support they need—including access to new AI tools that allow them to focus on what matters most in the classroom. Given the importance of a post-secondary degree or credential for success nowadays, we’re funding initiatives to increase graduation rates, too.
As I mentioned, having access to a high-quality nutrition source is key to keeping kids’ development on track. Smallholder farmers form the backbones of local economies and food supplies, and they play a key role in making that happen. One of the main ways the foundation helps farmers is through the development of new, more resilient seeds that yield more crops even under difficult conditions. This work is even more important in a warming world, since no one suffers more from climate change than farmers who live near the equator. Despite that, I’m hopeful that we can help make smallholder farmers more productive than ever over the next two decades. Some of the crops our partners are developing even contain more nutrients—a win-win for both climate adaptation and preventing malnutrition.
We’ll also continue supporting digital public infrastructure, so more people have access to the financial and social services that foster inclusive economies and open, competitive markets. And we’ll continue supporting new uses of artificial intelligence, which can accelerate the quality and reach of services from health to education to agriculture.
Underpinning all our work—on health, agriculture, education, and beyond—is a focus on gender equality. Half the world’s smallholder farmers are women, and women stand to gain the most when they have access to education, health care, and financial services. Left to their own devices, systems often leave women behind. But done right, they can help women lift up their families and their communities.
The United States, United Kingdom, France, and other countries around the world are cutting their aid budgets by tens of billions of dollars. And no philanthropic organization—even one the size of the Gates Foundation—can make up the gulf in funding that’s emerging right now. The reality is, we will not eradicate polio without funding from the United States.
While it's been amazing to see African governments step up, it’s still not enough, especially at a moment when many African countries are spending so much money servicing their debts that they cannot invest in the health of their own people—a vicious cycle that makes economic growth impossible.
It's unclear whether the world’s richest countries will continue to stand up for its poorest people. But the one thing we can guarantee is that, in all of our work, the Gates Foundation will support efforts to help people and countries pull themselves out of poverty. There are just too many opportunities to lift people up for us not to take them.
The last chapter of my career
Next week, I will participate in the foundation’s annual employee meeting, which is always one of my favorite days of the year. Although it’s been many years since I left Microsoft, I am still a CEO at heart, and I don’t make any decisions about my money without considering the impact.
I feel confident putting the remainder of my wealth into the Gates Foundation, because I know how brilliant and dedicated the people responsible for using that money are—and I can’t wait to celebrate them.
I'm inspired by my colleagues at the foundation, many of whom have foregone more lucrative careers in the private sector to use their talents for the greater good. They possess what Andrew Carnegie called “precious generosity,” and the world is better off for it.
I am lucky to have been surrounded by many generous people throughout my life. As I wrote in my memoir Source Code, my parents were my first and biggest influences. My mom introduced me to the idea of giving back. She was a big believer in the idea of “to whom much is given much is expected,” and she taught me that I was just a steward of any wealth I gained.
Dad was a giant in every sense of the word, and he, more than anyone else, shaped the values of the foundation as its first leader. He was collaborative, judicious, and serious about learning—three qualities that shape our approach to everything we do. Every year, the most important internal recognition we hand out is called the Bill Sr. Award, which goes to the staff member who most exemplifies the values that he stood for. Everything we have accomplished—and will accomplish—is a testament to his vision of a better world.
As an adult, one of my biggest influences has been Warren Buffett, who remains the ultimate model of generosity. He was the first one who introduced me to the idea of giving everything away, and he’s been incredibly generous to the foundation over the decades. Chuck Feeney remains a big hero of mine, and his philosophy of “giving while living” has shaped how I think about philanthropy.
I hope other wealthy people consider how much they can accelerate progress for the world’s poorest if they increased the pace and scale of their giving, because it is such a profoundly impactful way to give back to society. I feel fulfilled every day I go to work at the foundation. It forces me to learn new things, and I get to work with incredible people out in the field who really understand how to maximize the impact of new tools.
Today’s announcement almost certainly marks the beginning of the last chapter of my career, and I’m okay with that. I have come a long way since I was just a kid starting a software company with my friend from middle school. As Microsoft turns 50 years old, it feels right that I celebrate the milestone by committing to give away the resources I earned through the company.
A lot can happen over the course of twenty years. I want to make sure the world moves forward during that time. The clock starts now—and I can’t wait to make the most of it.
Field notes
The world needs more Nick Kristofs
I loved this journalist’s story of chasing hard problems and holding onto hope.

If you’re a big reader, you can probably point to a book or two that changed the course of your life. For me, it was a 1997 New York Times column by Nicholas Kristof about diarrhea, which was killing three million kids a year.
At the time, I had wealth—and knew I planned to give it away—but no clear mission. Nick’s article gave me one. I faxed it to my dad with a note: “Maybe we can do something about this.”
That ended up setting the direction for what became the Gates Foundation. It didn’t just give us a what—it gave us a how. Nick’s reporting showed us that the biggest challenge in global health isn’t always discovering new breakthroughs. Often, it’s making sure the tools we already have—vaccines, medicines, bed nets, or oral rehydration therapies for rotavirus—reach every child, no matter where they’re born.
Reading Nick’s new memoir, Chasing Hope, brought me back to that moment and showed me how it fit into the bigger story of his life. The book is a deeply personal account of a life spent documenting injustice and refusing to look away, whether it’s genocide in Darfur, refugee camps in Sudan, or the streets of his hometown in rural Oregon.
Nick’s impulse to go where the suffering is, and to make people care, has defined his career. He’s reported from more than 150 countries, covering war, poverty, health, and human rights. He and his longtime collaborator and wife, Sheryl WuDunn, won a Pulitzer Prize for their work. Together and individually, they’ve brought injustices around the world into view for millions of readers.
But Chasing Hope isn’t just a greatest-hits collection of his past reporting. It’s the story of how someone becomes Nick Kristof. He writes about growing up on a sheep and cherry farm in Oregon, driving tractors as a teenager, and nearly becoming a lawyer before deciding on journalism. He also reflects on the toll his career has taken on him, his family, and his capacity for hope.
I’ve known Nick for many years now, and I’ve admired his work since that 1997 rotavirus column. On paper, we don’t seem all that similar. He’s a journalist, I’m a technologist; he tells stories, I talk numbers. But reading Chasing Hope, I was struck by what we have in common: growing up in the Pacific Northwest, learning about the value of service from our parents, thinking globally.
We both attended Harvard and left early—me because I dropped out, him because he graduated in three years before heading to Oxford as a Rhodes Scholar. But neither of us ever stopped learning. I think we both believe the world’s pretty interesting if you remain a student.
Nick’s curiosity didn’t come out of nowhere, and neither did his sense of purpose. His mother was an art history professor and a civic leader who helped influence local politics. His father, a political science professor who fled both Nazism and communism, believed deeply in education and the responsibilities that come with freedom. That kind of upbringing left a mark on him and shaped the kind of journalist he became.
Over decades, he’s built a career reporting on crises that are often ignored because they happen in far-off places, far from centers of power. In Chasing Hope, he recounts his experiences chronicling river blindness in Ethiopia, maternal mortality in Cameroon, and malaria in Cambodia. Through the foundation, I mobilize science, data, and funding to address many of the same global challenges Nick reports on. Our approaches are different, but the underlying questions we ask (and try to answer) are the same: Why are some lives valued less than others? And how can we use the tools we have—information, resources, attention—to close that gap?
Nick has an admirable commitment to nuance, especially when it comes to hard subjects like China. Nick lived there for years, speaks Mandarin, and understands the country in a way most Western commentators don’t. I’ve always appreciated his ability to go beyond the headlines—and focus not just on what’s going wrong, but on what’s changing and why it matters.
Nick is also an optimist, which might sound strange given the kinds of suffering he writes about. But his work is grounded in a belief I share: The right data—or the right story—can move people to act. As Nick puts it, “A central job of a journalist is to get people to care about some problem that may seem remote.” People, when given the chance, want to make things better. Progress, while never guaranteed, is possible.
That optimism feels especially important, if increasingly difficult, right now. Isolationism is on the rise around the world, and governments are cutting back on foreign aid at the very moment when we should be doing more, not less. Millions of lives are at stake. Nick’s work reminds us what’s possible when we care about people beyond our own borders—and what happens when we don’t.
Chasing Hope made me think a lot about what kind of person chooses to run toward the hardest problems—and keep going back until they’re solved. It also made me think the world would be a much better place if there were more Nick Kristofs. In the meantime, we’re lucky to have this one.
Back for the future
I’m heading back to India
This trip will give me the chance to see what’s working, what’s changing, and what’s next—for India and the Gates Foundation.

In a few days, I’ll be traveling to India—my third visit in three years. India is a place where big challenges meet even bigger ambitions, and where innovation is transforming lives at an incredible scale. Every time I’m there, I see firsthand how much progress is being made in public health, agriculture, and technology. And I come away with new ideas, because India is full of smart, ambitious people tackling some of the world’s hardest problems in creative ways.
This visit will also be significant because—as we mark our 25th anniversary—the Gates Foundation’s Board of Trustees is meeting in the Global South for the first time. India is the right place for this milestone. The foundation has been working in the country for more than two decades, partnering with the government, researchers, and entrepreneurs to improve health and development. Today, India is home to some of the most impactful programs we’ve contributed to, from disease eradication and sanitation to women’s empowerment and digital financial services. This trip will give me a chance to see what’s working, what’s changing, and what’s next—for India and the foundation.
India’s track record in public health shows what’s possible. When I visited in 2011, it was one of the last places in the world still fighting polio. But that year, after relentless effort, India recorded its last case—and it’s remained polio-free ever since. Avahan, the HIV prevention program launched by the Gates Foundation two decades ago, is another success story. It pioneered a community-led approach to reduce infection rates that complemented the government’s efforts in high-prevalence states; eventually, management of the program transitioned to the Indian government, becoming part of the country’s broader health strategy.
That same model—leveraging local leadership, innovative solutions and data-driven insights—is now driving India’s fight against tuberculosis. The country has the world’s highest TB burden, but its investment in new diagnostics, AI-powered detection tools, and improved treatment strategies is accelerating progress toward elimination.
India’s success in childhood immunization is another reason I’m eager to return and learn more. Over the past several years, the country has scaled up routine vaccination programs, ensuring every major childhood vaccine is available. It has also used digital dashboards to track vaccine coverage, monitor cold storage, and improve maternal and child healthcare. These efforts have helped drive down mortality rates and create a stronger health system that can respond to new challenges.
India’s global health leadership is also transforming how the country approaches diagnostics and treatment for infectious diseases. As a result, it’s become a leader in low-cost vaccine manufacturing, ensuring that life-saving vaccines are available around the world. Indian companies are also tackling another critical challenge: making diagnostics more affordable. One effort I’m following closely is the push to make a saliva-based TB test for under $2, which could help millions of people in India and globally detect the disease earlier and get treatment faster.
Beyond health, India is also at the forefront of digital transformation. I’ve written before about how digital public infrastructure (DPI)—like Aadhaar and India’s digital payments system—has made it easier for millions of people to access banking, healthcare, and government services. Now, India is using AI-powered DPI tools to help rural health workers improve early disease detection, optimize pregnancy care, and manage patient data more effectively.
AI is also transforming agriculture across the country. When I was in Odisha last year, I saw farmers using AI-powered tools to predict weather patterns, choose crops, and reduce disease risks. I’m looking forward to seeing how much better those tools have gotten in the short time since.
What makes India’s progress so transformative, though, is that it doesn’t just benefit India. During India’s G20 Presidency in 2023, Prime Minister Modi declared his intent to make Indian innovations and know-how available to solve development problems globally. And that’s exactly what is happening. The solutions being developed there, from vaccine manufacturing to AI-powered diagnostics, are being shared with the world. Indian companies are making TB tests that could be game-changing across Africa. They’re developing AI models that could help farmers across Asia. And they’re proving that digital technology can make healthcare work better for everyone, especially the most vulnerable.
At the Gates Foundation, we tackle tough problems by working in close partnership with the people and governments most affected by them. India has been an incredible partner in this work because of the country’s deep expertise and willingness to develop and scale new ideas. The challenges remain: eliminating TB, improving nutrition, expanding access to AI-driven health and development services. But India has shown time and again that progress happens when innovation, local leadership, and investment come together.
That’s why I’m so excited for this trip. I’ll be meeting with government leaders, scientists, and philanthropists who are shaping the future of health and development in India. I’ll be visiting innovators who are working on solutions that could help people in India and around the world. And I’ll get to see how the foundation’s work fits into this bigger story—and how we can continue to support Indian-led efforts to improve lives.
I always leave India inspired. I know this trip will be no different.
The sky’s the limit
The Drone Didis are taking flight
Drones are helping rural women boost their income and India’s agricultural productivity.

I was excited to get a drone for my birthday last year. I couldn’t wait to get it into the air and see what my backyard looked like from the sky. But, as anyone who has used one can tell you, I quickly learned a harsh truth: Flying a drone isn’t easy. It takes a lot of practice and skill.
Maybe it’s time to pull the drone back out, because I was lucky to get a lesson from the experts last month in India. During my visit to Delhi, I met with Sangita Devi, Sumintra Devi, and Kajol Kumari—three Drone Didis from Bihar who are taking India’s agricultural productivity to new heights.
The women I met are part of the Indian government’s Namo Drone Didi program. (Didi is the Hindi word for “sister.”) It was launched in 2023 to help rural women boost their income and boost India’s agricultural productivity—and although the program is still in its early days, I’m already impressed by its results.
Right now, the Drone Didis primarily use their flying skills to fertilize crops. Applying fertilizer via drone has a lot of benefits over doing it by hand. Since you can spray farther away from the plant, the liquid fertilizer becomes more atomized—which means that it turns into finer droplets that cover more area. This benefits both farmers and the environment, because you need significantly less fertilizer and less water to help distribute it. Plus, it’s faster. One Drone Didi can cover as much as five acres in the same time it would take five people to cover half an acre.
I cannot wait to see how the program expands in the years ahead. The Indian government has plans to equip the drones with advanced sensors and imaging technology. This will allow Drone Didis to use real-time data to deliver targeted interventions to improve the quality and quantity of farmers’ crops. They will be able to detect diseases and pests, assess soil moisture levels, monitor crop growth, and more.
I’m equally excited to track how the Drone Didi program continues to empower women across India. Every Didi is affiliated with a self-help group, or SHG. The plan is to provide nearly 15,000 drones to SHGs across India by the end of next year.
In the United States, where I live, self-help groups are usually associated with mental health. In India, they’re a form of mutual aid. Each SHG is small—most are around 12 people, although some are as big as 25—and brings together women to support each other socially and financially. They pool their savings, access microloans at lower interest rates, and solve problems in areas like health and education.
The Didis I met with were longtime members of SHGs organized by JEEViKA, an organization in Bihar that works to lift people from rural areas out of poverty. During our time together in Delhi, Kajol told me about how JEEViKA helped her open her own shop three years ago, where she sells seeds and fertilizers. She loves being an entrepreneur, and when she was approached about becoming a Drone Didi, she knew it would do wonders for her business.
Each Didi attends a training program in Hyderabad or Noida, where they are taught how to pilot the drone and apply fertilizer effectively. (I was surprised to hear that learning to fly is apparently easier and takes less time than learning to fertilize!) Other women in their SHGs are trained as drone technicians, ready to repair the machines if any problems arise.
In the less than two years, the Drone Didi program is already transforming the lives of its pilots. Kajol is using the extra income she’s earned to expand her shop offerings and build a warehouse to store her stock. She also plans to send her children to a better school. Sangita’s family couldn’t afford a bicycle before she became a Drone Didi—today, she is the proud owner of an auto rickshaw.
Sumintra hopes that, when people see someone like her flying a huge drone, it changes their perception of what women are capable of. Like many women in her area, she married very young and was expected to stay home with her children. Today, her kids call her “Pilot Mummy” and dream about her flying airplanes one day.
I hope you think of the Didis the next time you hear the buzz of a drone above you at a wedding or a park. It’s remarkable how one piece of technology can reshape what is possible in a community. Kajol told me that people sometimes look at her and say, “She’s flying too high! What will she do next?”
Her response? “This is just the beginning. Wait and see what’s coming.”

Ancient gains
Could a grain older than the wheel be the future of food?
Lost crops like fonio could help us fight climate change and malnutrition.

What grain did your family grow up eating? I’m from the United States, where wheat and corn are king. But if I had been born in East Asia, I probably would’ve eaten a lot more rice as a kid.
If you grew up in West Africa, you might have eaten an ancient grain called fonio. Fonio has been feeding families in West Africa for more than 5,000 years, longer than any other cultivated grain on the continent. That makes it older than toilets, the wheel, and even writing. It’s a super small grain with a texture that reminds me a bit of couscous when cooked in hot water. Its nutty taste is delicious on its own but is also good when ground into flour.
Fonio is just one part of a much bigger family of remarkable ancient grains: the millets. Perhaps you’ve heard of finger millet. It’s a staple in Uganda and parts of Kenya and Tanzania, and it’s beloved in India where it is called ragi. Or maybe you’ve heard of teff, a longtime favorite in Ethiopia where it’s used to make injera.
Millets have been around for centuries, but they’re currently experiencing a resurgence—both for consumers who enjoy their taste and for farmers who appreciate how reliable they are to grow.
Fonio, in particular, is like farming on easy mode. You wait until a good rain comes, lightly till the soil to loosen it up, and then scatter the seeds on the ground. Two months later, you harvest the grain.

Farm work
On Africa’s farms, the forecast calls for adaptation and innovation
In Kenya, I visited with a smallholder farmer using new tools and practices to fight back against climate change.

I planted drought-tolerant seeds, fed and weighed chickens, and used a mobile phone to monitor weather forecasts and local crop prices.
These were a few of the chores I was given during my visit with Mary Mathuli, a smallholder farmer in rural Kenya.
I stopped at her home in Makueni County, south-east of Nairobi, during my recent trip to Kenya to better understand how farmers like Mary are faring in the face of climate change.
I arrived expecting to hear her talk about the record droughts and smaller harvests many farmers are experiencing throughout Africa.
Instead, to my surprise, she led me out to her fields to show off the innovations that are allowing her to continue to grow crops and earn an income to support her family, despite the drastic changes in rainfall and weather patterns.
A natural teacher, Mary encouraged me to learn by doing. She put me to work so I could understand how these new agricultural inputs and practices can make a big difference in their lives.
This experience taught me a couple important lessons.
First, my farming skills—like holding a chicken and swinging a hoe—need some work.
Second, and more importantly, I got a personal reminder of how resourceful and resilient African smallholder farmers like Mary are. Battered by years of drought and other extreme weather patterns, they are developing new skills and embracing new technologies to adapt to some of the toughest conditions for growing crops and raising livestock.
To be clear, African farmers face huge challenges due to climate change. Although sub-Saharan Africa accounts for only about four percent of the world’s carbon emissions, the continent is bearing the brunt of climate change impacts. Climate-related losses on many African farms are more than double those seen globally. In Makueni County, where Mary farms, yields of maize have been falling since 1994, largely due to changes in the weather.
While more innovation is needed to help Africa’s smallholder farmers keep pace with the threats posed by climate change, Mary and other farmers in Kenya are adopting some incredible new tools and practices that can limit crop losses and help their farms thrive even in extreme weather:
As farms go, Mary’s farm is quite small. Just about 4 acres, which is typical for farms in Africa. Still, she packs a lot of activities in this space, growing commercial and subsistence food crops and rearing poultry and livestock. In sub-Saharan Africa, more than half of the population works in agriculture. Together, they produce about 80 percent of the continent’s food supply. And most of the people doing the backbreaking farm work—like the chores I performed—are women.
I was impressed by Mary’s entrepreneurial spirit and her optimism. She appeared to seize every opportunity to try out new technologies and agricultural practices. It’s one of the reasons why she was trained as a model farmer and Village Based Advisor by the Cereal Growers Association, an organization that works with smallholder farmers to help improve their productivity. In this role, Mary provides guidance to several hundred farmers in her community, showing them how to use drought-tolerant seeds, raise chickens, and adopt other climate adaptation agricultural strategies.
She is clearly doing a good job in this role because more than 90 percent of farmers in her area have embraced one of the new adaptation practices.
I look forward to hearing how the seeds I planted with Mary are doing, despite the disappointing rains in recent months. I can’t imagine them in better hands than hers.
Thanks so much for the visit, Mary!
Food for thought
What it will really take to feed the world
In his latest book, one of my favorite authors argues that solving hunger requires more than producing more food.

In the introduction to his latest book, How to Feed the World, Vaclav Smil writes that “numbers are the antidote to wishful thinking.” That one line captures why I’ve been such a devoted reader of this curmudgeonly Canada-based Czech academic for so many years. Across his decades of research and writing, Vaclav has tackled some of the biggest questions in energy, agriculture, and public health—not by making grand predictions, but by breaking down complex problems into measurable data.
Now, in How to Feed the World, Vaclav applies that same approach to one of the most pressing issues of our time: ensuring that everyone has enough nutritious food to eat. Many discussions about feeding the world focus on increasing agricultural productivity through improved seeds, healthier soils, better farming practices, and more productive livestock (all priorities for the Gates Foundation). Vaclav, however, insists we already produce more than enough food to feed the world. The real challenge, he says, is what happens after the food is grown.
This kind of argument is classic Vaclav—questioning assumptions, forcing us to rethink the way we frame problems, and turning conventional wisdom on its head. His analysis is never about the best- or worst-case scenarios; it’s about what the numbers actually tell us.
And the numbers tell a striking story: Some of the world’s biggest food producers have the highest rates of undernourishment. Globally, we produce around 3,000 calories per person per day—more than enough to feed everyone—but a staggering one-third of all food is wasted. (In some rich countries, that figure climbs to 45 percent.) Distribution systems fail, economic policies backfire, and food doesn’t always go where it’s needed.
I’ve seen this firsthand through the Gates Foundation’s work in sub-Saharan Africa, where food insecurity is driven by low agricultural productivity and weak infrastructure. Yields in the region remain far lower than in Asia or Latin America, in part because farmers rely on rain-fed agriculture rather than irrigation and have limited access to fertilizers, quality seeds, and digital farming tools. But even when food is grown, getting it to market is another challenge. Poor roads drive up transport costs, inadequate storage leads to food going bad, and weak trade networks make nutritious food unaffordable for many families.
And access is only part of the problem. Even when people get enough calories, they’re often missing the right nutrients. Malnutrition remains one of the most critical challenges the foundation works on—and it’s more complex than eating enough food. While severe hunger has declined globally, micronutrient deficiencies remain stubbornly common, even in wealthy countries. One of the most effective solutions has been around for nearly a century: food fortification. In the U.S., flour has been fortified with iron and vitamin B since the 1940s. This simple step has helped prevent conditions like anemia and neural tube defects and improve public health at scale—close to vaccines in terms of lives improved per dollar spent.
One of the most interesting parts of the book is Vaclav’s exploration of how human diets evolved. Across civilizations, people independently discovered that pairing grains with legumes created complete protein profiles—whether it was rice and soybeans in Asia, wheat and lentils in India, or corn and beans in the Americas. These solutions emerged from practical experience long before modern science could explain why they worked so well.
But just as past generations adapted their diets to available resources, we’re now facing new challenges that require us to adapt in different ways. Technology and innovation can help. They’ve already transformed the way we produce food, and they’ll continue to play a role. Take aquaculture: Once a tiny industry, it’s grown over the past 40 years to supply more seafood for the world than traditional fishing—a scalable way to meet global protein demands. The Green Revolution is another example. Beginning in the 1960s, innovations in higher-yielding crops, more effective fertilizers, and modern irrigation prevented widespread famine in India and Mexico. These changes were once seen as unlikely, too.
New breakthroughs could drive even more progress. CRISPR gene editing, for instance, could help develop crops that are more resilient to drought, disease, and pests—critical for farmers facing the pressures of climate change. Vaclav warns that we can’t count on technological miracles alone, and I agree. But I also believe that breakthroughs like CRISPR could be game-changing, just as the Green Revolution once was. The key is balancing long-term innovation with practical solutions we can implement immediately.
And some of these solutions aren’t about producing more food at all—they’re about wasting less of what we already have. Better storage and packaging, smarter supply chains, and flexible pricing models could significantly reduce spoilage and excess inventory. In a conversation we had about the book, Vaclav pointed out that Costco (which might seem like the pinnacle of U.S. consumption) stocks fewer than 4,000 items, compared to 40,000-plus in a typical North American supermarket.
That kind of efficiency—focusing on fewer, high-turnover products—reduces waste, lowers costs, and ultimately eases pressure on global food supply, helping make food more affordable where it is needed most.
How to Feed the World had a lot to teach me—and I’m sure it will teach you a lot, too. Like all of Vaclav’s best books, it challenges readers to think differently about a problem we thought we understood. Growing more and better food remains crucial—especially in places like sub-Saharan Africa, where there simply isn’t enough. But as the world’s population approaches 10 billion, increasing agricultural productivity alone won’t solve hunger and malnutrition. We also need to ensure that food is more accessible and affordable, less wasted, and just as nutritious as it is abundant.
After all, the goal isn’t to make more food for its own sake—it’s to feed more people.

Alphabet soup
You’ve probably never heard of CGIAR, but they are essential to feeding our future
No other institution has done as much to feed our world as CGIAR.

What’s for dinner?
It’s a question asked every day in homes around the world. No other organization has done as much to ensure families—especially the poorest—have an answer to that question as CGIAR, the world’s largest global agricultural research organization.
More than 50 years ago, CGIAR’s research into high-yielding, disease-resistant rice and wheat launched the Green Revolution, saving more than a billion people from starvation. In the years since then, their work on everything from livestock and potatoes to rice and maize has helped reduce poverty, increase food security, and improve nutrition.
Never heard of CGIAR? You’re not alone. It’s an organization that defies easy brand recognition. For starters, its name is often mistaken for “cigar,” suggesting a link to the tobacco industry. And it doesn’t help that CGIAR is not a single organization, but a network of 15 independent research centers, most referred to by their own confusing acronyms. The list includes CIFOR, ICARDA, CIAT, ICRISAT, IFPRI, IITA, ILRI, CIMMYT, CIP, IRRI, IWMI, and ICRAF, leaving the uninitiated feeling as if they’ve fallen into a bowl of alphabet soup.
It’s too bad that more people don’t know about CGIAR. Their work to feed our hungry planet is as important now as it’s ever been. By 2050, as the world’s population gets bigger and incomes increase (which causes dietary changes like eating more meat), global food demand is expected to increase by 60 percent. Meeting this challenge is made tougher by climate change, which is affecting food production in every corner of the globe. Farmers are under assault from shifting rainfall, more frequent and extreme droughts and floods, and severe pest and disease outbreaks among crops and livestock.
The people who are most affected by these changes today are the world’s smallholder farmers. About 500 million farming households, in South Asia and sub-Saharan Africa, earn their living by raising crops and livestock on small parcels of land. These families have the fewest resources to cope with the many impacts of a warming climate.
I’ve been writing a lot this year about why reducing emissions from all sectors of our economy, including agriculture and electricity generation, is critical in our fight against climate change. But it’s equally important for the world to stay focused on helping vulnerable populations, like smallholder farmers, prepare for the disruptive impacts of climate change. We owe it to them. The people who will suffer most from climate change, especially in sub-Saharan Africa, are the least responsible for emitting these greenhouse gases. According to an Africa Progress Panel report, an average Ethiopian would have to live for 240 years to equal the carbon footprint of the average American.
I’m now co-chairing the new Global Commission on Adaptation, which is playing a key role in building government and public support for efforts to reduce the impacts of climate change on communities most at risk. We will need CGIAR’s research to help supply farmers with a steady stream of climate-smart crop varieties.
A great example of a CGIAR innovation helping smallholder farmers adapt to climate change is its drought-tolerant maize program. More than 200 million households in sub-Saharan Africa depend on maize for their livelihoods. Maize productivity in Africa is already the lowest in the world. And as weather patterns have become more erratic, farmers are at greater risk of having smaller maize harvests, and sometimes no harvest at all.
In response to this challenge, CGIAR’s International Maize and Wheat Improvement Center or CIMMYT, with funding from our foundation, USAID and the Howard Buffett Foundation, developed more than 150 new maize varieties that could withstand drought conditions. Each variety is adapted to grow in specific regions of Africa. At first, many smallholder farmers were afraid of trying new crop varieties instead of more commonly planted ones. But as CIMMYT worked with local farmers and seed dealers to share the benefits of these new varieties, more and more farmers adopted drought tolerant maize. The results have been life changing for many farming families.
In Zimbabwe, for example, farmers in drought-stricken areas using drought-tolerant maize were able to harvest up to 600 kilograms more maize per hectare than farmers using conventional varieties. The additional harvest was enough to feed a family of six for 9 months. For farming families who chose to sell their harvests, it was worth $240 in extra income, giving them much-needed cash to send their children to school and meet other household needs.
CIMMYT, in partnership with another CGIAR center, the International Institute of Tropical Agriculture or IITA, has gone on to develop other maize varieties for farmers who are not only vulnerable to drought, but also poor soils, disease, pests, and weeds. These varieties are expected to give farmers up to 30 percent greater yields and help them fight malnutrition.
CGIAR’s team of more than 8,000 scientists and staff around the world are also developing other tools to help farmers adapt to unpredictable weather and diseases. They have created a smart phone app that allows farmers to use the camera on their phone to identify specific pests and disease attacking cassava, an important cash crop in Africa. There are also new programs to use drones and ground sensors to help wheat and sugarcane farmers determine how much water and fertilizer their crops need.
We will need many new ideas like these to help farmers be prepared to meet the challenges of our changing climate. If they are, we will all have an answer to the question “What’s for dinner?” for years to come.

Farm aid
A warmer world will hurt this group more than any other
We need to help the world’s poorest people adapt to climate change.

I’ve spent a lot of time over the last month talking about climate change. Whether it’s on my book tour, in media interviews, or just during conversations with colleagues, it’s been great to have so many thoughtful conversations with people about how we prevent the worst effects of climate change.
Most of the questions I’ve gotten are about how we get to zero greenhouse gas emissions. Mitigation is the biggest climate problem we need to solve, and it’s been great to see it get so much attention. But I’ve noticed there’s one key topic that people don’t ask about as much: how we can help the world adapt to climate change.
I understand why. I dedicated five chapters of the book to mitigation and only one to adaptation. (In retrospect, I wish I had written more about the subject.) But there’s a reason I named my book “How to Avoid a Climate Disaster” and not “How to Stop Climate Change:” Our climate is already changing.
You just need to look at last month’s freeze in Texas and last year’s wildfires in California to see that extreme weather events are becoming more common. The scary thing is that these events aren’t the only (or even the most devastating) way a warming world is making life more difficult for people. The biggest damage is happening too gradually to make headline news, mostly in places near the Equator—and no one is more at risk than the world’s poorest people.
About two-thirds of those living in poverty work in agriculture, often relying on the food they grow to feed their families. A warmer world will be problematic for relatively well-off farmers in America and Europe, but potentially deadly for low-income farmers in Africa and Asia.
The closer you live to the Equator, the worse the effects of climate change will be. Droughts and floods will become more frequent, wiping out harvests more often. Livestock will eat less and produce less meat and milk. The air and soil start to lose moisture, leaving less water available for plants; in South Asia and sub-Saharan Africa, tens of millions of acres of farmland will become substantially drier.
When you’re already living on the edge, any one of these changes could be disastrous. We’re likely going to see a situation for these farmers where, instead of your crop getting wiped out every ten years, it gets wiped out every four years. If you don’t have money saved up to buy imported food—which is the case for most smallholder farmers—your children will likely become malnourished and more susceptible to disease.
The worst impact of climate change in poor countries will be to make health worse—which is yet another reason why we need to help the poorest improve their health. This starts with raising the odds that malnourished children will survive by improving primary healthcare systems, doubling down on malaria prevention, and continuing to provide vaccines for conditions like diarrhea and pneumonia. We also need to ensure that fewer children are malnourished in the first place by helping poor farmers grow more food.
This is a problem we can help solve with innovation. We need better methods and tools to grow food, just like we need to find zero-carbon ways to move around and generate electricity. No other organization is in a better position to create the innovations that will help poor farmers adapt to climate change in the years ahead than CGIAR, a global partnership that helps make plants and animals more resilient and productive. (I’ve written about how amazing CGIAR is before.)
Our foundation first got involved with CGIAR more than a decade ago, when we supported their work to develop drought- and flood-tolerant varieties of staple crops like maize. We’re already seeing big improvements in places like Zimbabwe. Farmers in drought-stricken areas there who used drought-tolerant maize were able to harvest up to 500 more pounds per acre than farmers who used conventional varieties—producing enough to feed a family of six for nine months.
CGIAR and other organizations are also creating tools to help farmers adapt to unpredictable weather, like sensors that tell you when to plant seeds and phone apps that help identify pests. Poor farmers need more advances like these, but to provide them, we need to invest more money in agricultural R&D. Doubling CGIAR’s funding so it can reach more farmers is one of the main recommendations by the Global Commission on Adaptation, which I led along with former UN secretary-general Ban Ki-moon and former World Bank CEO Kristalina Georgieva. (Other recommendations include shoring up water infrastructure and building a stronger safety net to help farmers recover faster.)
If we don’t take steps now to help farmers adapt, we’re setting ourselves up for a humanitarian and geopolitical disaster. The U.S. military predicts that climate change will become a huge driver of global instability. When people can’t grow enough food to feed themselves, they often leave those areas for places that can better support their families. We’re going to see more “climate refugees” move to cooler regions as the world gets warmer. The Department of Defense is already thinking about where a warmer climate could cause conflicts that they would be asked to intervene in.
It’s deeply unfair that the people who contribute the least to climate change will suffer the worst from its effects. Extreme poverty has plummeted in the past quarter century, from 36 percent of the world’s population in 1990 to 10 percent in 2015 (although COVID-19 is a huge setback that is undoing a great deal of progress). Climate change could erase even more of these gains, increasing the number of people living in extreme poverty by 13 percent.
Rich and middle-income countries are causing the vast majority of climate change, and we need to be the ones to step up and invest more in adaptation. The world’s poorest deserve our help, and they need more of it than they’re getting.

Net gains
Planes, trains, and smartphones
The future of public infrastructure is digital, efficient, and for everyone.

Almost thirty years ago, I wrote a book called The Road Ahead, about the transformative potential of the internet and other new digital technologies. Back then, I envisioned a world where online payments and e-government would change how we interact with money, services, and each other. Today, much of that has become a reality, in part due to the development of digital public infrastructure. In my recent travels around the world, I’ve seen up close how DPI is revolutionizing the way entire nations serve their people, respond to crises, and grow their economies. And at the Gates Foundation, we see it as an important part of our efforts to help save lives and fight poverty in poor countries.
There are a few core components that constitute DPI: digital ID systems that securely prove who you are, payment systems that move money instantly and cheaply, and data exchange platforms that allow different services to work together seamlessly. These systems and platforms are to the digital world what roads, bridges, and power lines are to the physical one—an underlying structure that connects people, data, and money online. Strong DPI can propel a country forward by making it easier for people to access essential services, participate in the formal economy, and improve their lives. On the flip side, DPI that is poorly implemented (or simply non-existent) can slow a country’s development and perpetuate inefficiencies and inequities.
In the 21st century, digital public infrastructure is proving to be as important for progress as its brick-and-mortar predecessors—and the effects have been impressive around the world, wherever it’s been embraced.

Accounting for accounts
Digital tech is turning the unbanked into the banked
More people have accounts than ever. Here’s what we need to do next.

In the worst days of COVID-19, when people around the world were out of work and struggling to pay for food and housing, many national governments came to the same conclusion about the best way to offer immediate help: send people cash. More than 200 countries introduced emergency cash transfer programs or expanded existing ones; India, for example, transferred money to 300 million people, 200 million of whom were women, in the weeks after its first lockdown. Brazil reached 70 million people with emergency transfers.
Imagine the risk involved in making these payments with paper money during a pandemic. Government workers would have to physically deliver these payments, potentially exposing them and everyone they encountered to the virus. In addition, the whole process would be expensive and time-consuming at a time when people need help as quickly as possible.
Fortunately, most governments didn’t have to resort to in-person payment. They were able to deposit cash transfers directly into people’s accounts—allowing them to give crucial support without paper bills changing hands. And during the pandemic, even more users were brought into the digital fold. For example, after financial regulators in West Africa temporarily allowed people to open accounts by text or telephone, more than 8 million signed up for accounts while their countries were in lockdown.
Globally, transferring so much money without cash was possible thanks to more than a decade of painstaking work by governments, financial service providers, nonprofits, and other partners. Today, about three quarters of people worldwide have an account at a financial institution or through a mobile money provider. That’s a 50 percent increase in the past ten years, and the growth has not just been in higher-income countries. Developing countries have increased 71 percent in that time.
This growth is great news because it means that more low-income people—and especially low-income women—are being empowered to use products that let them make and receive payments, save and borrow money, and get insurance. Both research and experience show that this financial inclusion helps people exit and stay out of poverty. And using digital technology to do it is a low-cost way to build economic resilience and reduce extreme poverty, which is why it’s an essential part of the Gates Foundation’s strategy. We have granted several hundred million dollars to partners who are helping low- and middle-income countries build digital financial systems.
Whenever I talk to friends about this work, they’re surprised to learn that roughly 1.4 billion adults can’t or don’t use any type of formal financial account, and most of those unbanked people live in low- and middle-income countries. One reason is that analog banking requires buildings, piles of paperwork, security guards, and tellers, making the cost per transaction so high that it’s not economical for a company to serve people with low balances and small transactions. As a result, people create ingenious informal banking methods—doing things like pooling cash with family and neighbors or creating community savings groups. As creative as these solutions are, they don’t allow people to build assets or move money instantly. And they are often risky—cash stashed under a mattress can be stolen, for example.
Today, the proliferation of mobile phones means that you no longer need so much expensive infrastructure to provide modern financial services. With digital technology, costs are low enough that it makes economic sense for companies to serve more of the people whom the old system has ignored.
An early example was M-PESA in Kenya, which let people living in cities send money to their relatives in rural areas efficiently and inexpensively. As it caught on, it was eventually used to make payments in shops. Likewise, India’s Universal Payment Interface allows users to make instant digital payments to each other at extremely low cost; it now includes 323 financial service providers throughout the country and handles nearly 6 billion transactions each month. During the pandemic, more than 80 million adults in India made their first digital payment to a merchant.
Yet even the exemplar countries aren’t reaching everyone who needs digital banking. That’s why the World Bank (with support from the foundation) runs the Global Findex database, a comprehensive survey of how adults borrow, save, and send money and manage risks. The Findex has been updated periodically since 2011, and the latest version was just published earlier today. Using data gathered from 128,000 adults in 123 economies, it highlights steps that will expand formal banking to everyone in the world who wants it.
I eagerly read an early copy of the Findex report as soon as I had the chance, and I’m glad I did. I recommend the report to anyone, especially policymakers, who wants more people to benefit from financial inclusion. When the world knows more about where inclusion is growing and where it isn’t, we’re better equipped to make sure we’re reaching the people who are still left out.
One Findex finding that jumped out to me is the gender gap. Although the world has made progress in empowering women to use formal financial services as much as men do, there’s still work to do. In developing countries, the gap was 9 percent in 2017 and 6 percent in 2021. The world can do better. Leaders should focus even more directly on expanding account ownership and use among women.
Another section of the report looks at a crucial question: What prevents the people who are still unbanked from joining the formal system? Knowing the answer will make it easier to create services that will work for them.
To find out, the researchers behind the Findex did extensive surveys of the unbanked. Their top explanations: The accounts are still too expensive, a family member already has one, banks are too far away, or they don’t have enough money to use an account. So making the accounts even more affordable, accessible, and appealing needs to be a priority. Introducing digital payments via mobile phones is a great way to start: Between 2014 and 2021, the percentage of people in Ghana using formal banking services went up 28 points, and virtually all of the increase was driven by people signing up for mobile-enabled digital payments.
I’ve heard people argue that there’s a simple way to automatically expand financial inclusion: introduce digital currencies, and specifically cryptocurrencies. But that idea isn’t rooted in an understanding of what poor people require—the kind of understanding that the Findex provides.
In many areas where the unbanked live, many transactions are still done in cash, so even people with digital accounts need the ability to convert digital money into paper money quickly, and vice versa. But today, that’s extremely difficult to do with cryptocurrencies, particularly in rural areas. In addition, cryptocurrencies don’t solve the problem of identification; buyers and sellers would still need to be able to prove they are who they say they are.
When it comes to financial inclusion, the most important thing is to consider what poor people require. That means creating secure financial systems that identify who is making transactions, and that are interoperable, so that a person using one system can make transactions with someone on another system. It also means updating regulations so they protect consumers while encouraging innovation.
I’m excited about the great progress that’s documented in this year’s Findex. More people around the world, including more women and low-income people, have and use bank accounts than ever before. A lot of people are still excluded, but we have a roadmap that is feasible without billions of dollars of extra money to build systems that empower them. By following the roadmap, we can help them lift themselves out of poverty and make the world a fairer place.

Two countries, five days
Highlights of my trip to Nigeria and Ethiopia
A few photos from my latest visit to Africa.

I’ve just wrapped up a busy five-day trip to Ethiopia and Nigeria. It’s the kind of trip that’s both tiring and energizing at the same time. Even though I stay in touch with a lot of partners in both countries—the Gates Foundation has been funding work in them for more than 15 years—there’s nothing quite like visiting to see the work in action.
Whenever I get home from a trip like this, friends are curious to hear how it went. Here’s what I’m telling them. From 2000 to 2019 or so, Ethiopia and Nigeria led the way on dramatic improvements in health and poverty that rippled across Sub-Saharan Africa. Since then, the pandemic, extreme weather, and political and economic instability have set both countries back, along with much of the rest of the continent. But as I saw on this trip, there’s great work going on in both places that makes me optimistic about their future, and Africa’s.
I want to share a few photos from the week. Thanks to everyone who shared their time and insights with me, including Prime Minister Ahmed of Ethiopia, Nigerian health minister Muhammad Ali Pate, and a special guest who came along for the trip: the amazing musician Jon Batiste. The foundation will be working with African partners even more in the future, and based on what I saw this week, my next visit will be just as inspiring.

Production diary
Behind the scenes of my new Netflix series
I had a lot of fun filming What’s Next?, which you can watch now.

I've always thought of myself as a student trying to get to the bottom of things. A good day for me is one where I go to sleep with just a little bit more knowledge than I had when I woke up in the morning. So, when I am deciding how to spend my time these days, I usually ask myself three questions: Will I have fun? Will I make a difference? And will I learn something?
My new Netflix Series, What’s Next? The Future with Bill Gates, is out today. And when I think back on the process of working on it over the last two years, the answer to all three questions is a resounding “yes.”
I had an amazing time working with the super talented director, Morgan Neville. Morgan directed one my favorite documentaries, Best of Enemies, which is about Gore Vidal’s and William Buckley’s debates during the 1968 U.S. presidential election. Morgan also won an Oscar for his terrific film 20 Feet from Stardom.
As you might guess from the title, What’s Next? is a show about the future. I’m very fortunate to get to work on a number of interesting problems. Between fighting to reduce inequities through the Gates Foundation, leading Breakthrough Energy’s work on the climate crisis, and my continued engagement with Microsoft, I have a front seat to some of the biggest challenges facing us today.
I feel extremely grateful to have had the opportunity to work with and learn from some truly incredible people during the making of this show. (I’m hesitant to even use the word “work” because the process was so much fun!) My hope is that people watch What’s Next? and feel like they’re joining me on my learning journey.
Each episode focuses on a different challenge: artificial intelligence, climate change, misinformation, disease eradication, and income inequality. I sat down with some of the big thinkers and innovators who are pushing for progress. Some of them have different ideas than I do about how to tackle these challenges, and I loved getting to hear their perspectives. It was an eye-opening experience.
I got to have conversations on camera with familiar faces like Dr. Anthony Fauci, Open A.I. co-founder Greg Brockman, and the groundbreaking director James Cameron. And I made a lot of new friends as well—including an ingenious malaria researcher from Burkina Faso named Abdoulaye Diabaté, young climate activists who impressed me with their intelligence and passion, and an amazing group of people from across the Bay Area who overcame tremendous adversity in their path from poverty to stability.
There also were dozens of people who participated in the series with standalone interviews, like my friend Bono and the brilliant Mark Cuban—each of whom brings an inspiring and grounded view of the challenges we’re facing. My hope is that, together, we can combat the doomsday narratives that so often surround these issues.
It’s hard to pick which discussion I learned the most from. But three conversations will always stand out in my memory: the ones with Lady Gaga, Senator Bernie Sanders, and my younger daughter, Phoebe.
Going Gaga
I couldn’t help but feel a little nervous.
I was in Palm Desert, CA, preparing to have a filmed conversation with Lady Gaga for our episode about misinformation. Being around famous people doesn’t normally affect me. But I’m a big fan of A Star is Born—especially its music—and I was aware of her reputation as an outsized personality. I couldn’t wait to hear what she had to say.
Luckily, I had nothing to worry about. I was blown away by how thoughtful Gaga was. She made me laugh with the outrageous stories of how she’s been the subject of misinformation in the past—and inspired me with some of the ways she thinks about the topic.
In the early years of her career, one of the most persistent internet rumors about Gaga was that she was actually a man. It became so mainstream that reporters would ask about it during interviews. She refused to confirm or deny it. Instead, Gaga turned it back on the interviewer and asked, “Would it matter if I was?”
On the day of our Netflix conversation, I had been filming earlier with my two sisters, Kristi and Libby. So I asked them to come and watch the conversation between Lady Gaga and me.

Start spreading the news
Amazing stories I wish everyone knew
Meet some of the heroes who are fighting poverty and saving lives.

Have you ever heard a story that was so cool you couldn’t help telling everyone you met about it? Something you knew and wished that everyone else did too?
That’s how I feel about the people whose work I get to learn about through the Gates Foundation. Every day, around the world, they save lives and help people lift themselves out of poverty. Some are scientists. Others are educators, nurses, midwives, or advocates. Their work is so inspiring to me that I’ve committed virtually all of my wealth to supporting it.
When I see how much passion people like Josephine have for helping themselves and their neighbors, I’m inspired to help too. I hope these stories will be as inspiring for you as they are for me.

More than a job
For Eva Nangalo, saving mothers and babies is a calling
She’s a midwife, teacher, and advocate—and she’s changing childbirth in Uganda.

Officially, Uganda’s maternal mortality rate is double the global average. But because that number doesn’t count those who give birth at home—in a country where poverty, distance, stigma, and distrust are all barriers to medical care—Eva Nangalo believes the real one may be much higher.
That’s why, as a midwife determined to eliminate these deaths altogether, she’s spent the past 23 years working to make hospital deliveries both more safe and more common.
For Nangalo, this is more than a job. It’s her life’s work, and something she’s felt called to do for as long as she can remember. “I was created to be a midwife, born to be a midwife, trained to be a midwife,” she said. “It’s what is in my DNA. That’s what I am.”
Working the night shift at Nakaseke General Hospital in rural central Uganda and tending to her family’s farm while off the clock, Nangalo is known for sleeping maybe one or two hours, if that, a day. When the power goes out in the middle of a delivery—which happens often—she uses the flashlight on her cellphone to get the job done. She even keeps her hair short rather than style it the way she’d prefer.
In her own words: “I’ve wanted my hair to be like other women. But then I think of the one dollar saving a mother’s life.”
That isn’t theoretical. Nangalo regularly reaches into her own pockets to ensure that expecting mothers have the transportation they need to get to the hospital in the first place—and the food, milk, and medicine they and their babies need to survive not only childbirth but also what comes next. She once tore a piece of her own bedsheet to give to a mother who didn’t have one at home.
It’s no wonder she’s made a name for herself—literally—among the women she’s served, with many choosing to name their daughters after her.
Her advocacy efforts—and their effects—are broad and far-reaching. Understanding the fears and misconceptions that exist in Uganda around healthcare facilities, she uses the radio to reach skeptics and explain the merits of hospital deliveries and the higher risks of fatal infection and bleeding inherent to home births. She helped establish a newborn clinic in Nakaseke, improving the safety of childbirth at the hospital and increasing the number of families served. She even pushed the government to make good on its own policies and open a health facility in every sub-county.
It’s no exaggeration to say that Eva Nangalo is making childbirth in Uganda safer for everyone involved.
“The future looks bright,” one colleague said, “if we have more and more people like Eva.” Fortunately, she’s working to ensure that’s exactly what happens.

The worst tragedy
Why do children die?
The toughest question I’ve ever had to answer.

Twenty-five years ago, I encountered a question that I have thought about literally every day since: Why do children die?
Before I tell you what drew me to this mystery, I want to acknowledge that child mortality is not an easy subject to talk about. As a parent, I can’t imagine what it would be like to lose a child. It is shocking even to see the words “children” and “die” used in the same sentence.
But I think “why do children die?” is one of the most important questions ever. It is hard to think of a measure of how a society is doing that reveals more than whether it is protecting its children, and especially its most vulnerable children. And the better we understand why children die, the more we can do to save them.
The very good news is that the world has made phenomenal progress in this area over the past several decades. Since 1990, the number of children who die every year has fallen by more than half! If progress on child mortality is a good measure of the state of the world, then—despite the huge global setbacks of the past few years, including COVID-19—the state of the world has improved dramatically. And based on what I know about innovations that are still to come, we can look forward to even more progress in the years ahead.
My introduction to the subject came 25 years ago, when I read a New York Times article about the health problems caused by unsafe drinking water in low- and middle-income countries. I was shocked to learn that every year, 3.1 million people—nearly all of them children—died of diarrhea, often because they had drunk contaminated water. Diarrhea kills 3.1 million children?, I thought. That can’t be true, can it? But it was.
I had to know more. What other major inequities did I not know about?
I read everything about global health that I could find, and I spoke to as many experts as I could. I learned that researchers define child mortality as the death of anyone under the age of 5. They use that age because the first five years are the riskiest time of childhood, when kids are the most vulnerable.
Learning about the history of child mortality helped me put the statistics in context. In 1950, some 20 million children died. In 1990, it was down to 12 million children, even though more babies were being born. By 2000, the number had dropped to fewer than 10 million. By 2019, it was below 5 million. Virtually all of these deaths occur in low- and middle-income countries.
So the next question was, why were so many children dying?
Around 18 percent of the deaths were caused by non-communicable conditions, such as cancer and cardiovascular problems. The large majority—82 percent—of the deaths were caused by communicable diseases, such as diarrhea and malaria, and health problems that their mothers experienced—and exacerbated by risk factors including malnutrition. (This 18:82 ratio still holds true today.)
On one hand, this was heartbreaking. The worst killers were all things that people in rich countries considered just an unpleasant episode (such as diarrhea) or never experienced at all anymore (such as malaria). In other words, although it was obviously true that children were dying because of deadly diseases, that was only part of the explanation. They were also dying because of where they were born.
On the other hand, it was encouraging to learn that such a large share of the deaths was preventable. When I saw the breakdown of diseases, I thought: Here is our road map. This is what the Gates Foundation should be working on. With the right team, partners, and funding, we could help the world move through the list, systematically going after the worst killers. The solutions that already existed could be made more affordable and delivered to people in low-income countries. The ones that didn’t exist could be invented.
Here is the chart as it looks today:
As you can see, pneumonia is the top preventable cause, but the story here is one of real progress. In 2000, it took the lives of more than 1.5 million children, but by 2019, the number was around 670,000—still an awful number, but a reduction of more than 55 percent. The innovation related to pneumonia that’s going on today is so exciting that I made a separate post and video about it.
Diarrhea is another example of progress. In two decades, its death toll has dropped 58 percent. A key reason is the use of low-tech interventions like oral rehydration solution (sugar water, essentially), which replaces lost electrolytes. Governments also ran large-scale sanitation programs to cut down on the spread of bacteria. And scientists developed an affordable rotavirus vaccine, and the world came together to deliver it. Between 2010 and 2020, this vaccine prevented more than 200,000 deaths. By 2030, it will have prevented more than half a million deaths.
Even though the overall number of deaths has gone down by half, the relative positions of the top three killers have not changed. They are the same today as in 1990: neonatal disorders, pneumonia, and diarrheal diseases. As you can see in this graphic, the fourth slot is where there has been a huge shift. In 1990, it was occupied by measles, responsible for half a million deaths. Today, it’s malaria that is in the fourth slot—not because malaria deaths went up (they actually went down), but because measles deaths fell by a whopping 87 percent.
Why? Vaccines. Since 2000, Gavi, the Vaccine Alliance has provided measles vaccines to more than 500 million children—half a billion!—through routine immunization and special vaccination campaigns. (This is just one example of the magic of vaccines—although unfortunately vaccination rates have dropped because of the pandemic and other factors.) And malaria may not be #4 on that list for long, thanks to innovations like malaria vaccines, improved insecticide-treated bed nets, and sugar baits.
Many groups deserve credit for the decades of progress I’ve described in this post. Countries with high disease burdens have launched massive vaccination campaigns, strengthened their health systems, and shared best practices with each other. Wealthy countries generously give aid that supports these efforts. Pharmaceutical companies have contributed technical expertise and made products affordable for low- and middle-income countries. Foundations including the Gates Foundation have stepped up with additional funding for innovative ideas. (At the foundation, we have staff and partners dedicated to each slice of the pie you see above.)
Although it’s still true that too many children do not live to see their fifth birthday, the world is moving in the right direction. If everyone keeps doing their part, we can move even faster and save even more lives. Because of COVID and other setbacks, the United Nations’ goal to cut childhood deaths in half again to below 3 million by 2030 will be missed, but it can still be achieved the following decade.
At a time when war and pandemic are in the news every day, it is important to look for reasons to be hopeful. The world’s opportunity—and ability—to save children’s lives is surely one of those reasons.

Bad air
A big threat to malaria eradication
Climate change could stall the world’s amazing progress on health.

It’s mind-blowing how much health has improved for the world’s poorest people over the past two decades. Malaria deaths, for example, have dropped by more than a third. Eradicating the disease has become a realistic goal.
Unfortunately, climate change threatens to slow or even reverse this progress. As temperatures go up and extreme weather events become more common, it will get harder to do things like provide bed nets, get rid of malaria-carrying mosquitoes, and offer basic health care in the world’s most vulnerable communities.
I’m optimistic that the world can avoid a climate disaster. But that effort can’t come at the expense of continuing progress on health care including malaria efforts.
If we fight only climate change and stop working on health, then we might reduce carbon emissions but allow malaria to make a comeback. Eradication would become even harder. No one will be better off in a world with fewer carbon emissions but more illness and death.
In this video, I talk more about the connection between climate change and malaria and explain why I’m optimistic that we can solve both problems.

The life of Neandersquito
This scientist uses old insects to help fight malaria
Mara Lawniczak has an ingenious approach to studying mosquito evolution.

Of all the things I thought would help fight malaria, 100-year-old mosquitoes would not have been high on the list. Then I learned about the work of Dr. Mara Lawniczak.
An evolutionary geneticist at the Wellcome Sanger Institute in the United Kingdom, Mara has spent much of her career trying to understand how the genomes of various mosquito species have changed in response to humans’ attempts to kill them. When, where, and how fast has it happened? What does that say about how they might evolve in the future?
In recent years, genetics has become an increasingly important tool for fighting malaria. Because mosquitoes breed so fast (a female can lay thousands of eggs in her lifespan of a couple of weeks), they evolve rapidly, at least compared to humans. By studying their genes, researchers are able to understand things like how they develop resistance to insecticides, crucial information that helps humans stay one step ahead.
After a few years of studying mosquitoes’ genomes, Mara had grown frustrated by the fact that the only insects available for study were ones that had been captured recently. Without DNA from their ancestors, there was no way to know how their genomes had responded to decades of human attacks. “We were often saying, ‘If only we could look into the past,’” Mara says. “And then it suddenly struck me: I'm sure there are historical collections of mosquitoes around.”
She was right. The Natural History Museum in London has a collection of 34 million insects from all over the world, carefully collected and preserved. Among the collection is a large sample of mosquitoes dating from 1936, when a British entomologist named H.S. Leeson spent a year in East Africa capturing and cataloguing the insects in the hope of learning more about malaria. Leeson didn’t know it at the time—DNA wouldn’t be discovered until the 1950s—but his collection of mosquitoes would become a vast source of genetic material that someone like Mara could study.
Mara reached out to the museum’s curators. They wanted to help, but there was a problem: Extracting DNA from the insects would require Mara to grind them up. Since the museum’s mission is to preserve its collection for future generations, they couldn’t let her do that.
So Mara and her colleagues invented a way around the problem. Working with the museum’s team, they developed a novel way to extract DNA from mosquitoes without damaging the specimen.
They affectionately call this work Project Neandersquito. It’s not because the mosquitoes date from the time of Neanderthals, some 40,000 years ago—this isn’t Jurassic Park, where they extract dinosaur DNA from a prehistoric mosquito trapped in amber. It’s because the mosquitoes they’re studying are 1,000 or 2,000 generations removed from modern ones, just as Neanderthals are more than 1,000 generations removed from modern humans.
Mara’s team has made some surprising finds. For example, because mosquitoes started developing resistance to the insecticide DDT in the 1950s, they expected to see genetic mutations for resistance appearing around the same time. But they didn’t. “We still don't see them even as late as the 1980s,” she says. “So the mosquitoes were somehow making themselves resistant to DDT in ways that we still don't really understand.”
They also hope to get insight into what's coming. “How fast can mosquitoes evolve? And as we throw new control initiatives at them, how quickly are they going to get around them?” Other labs are now using the process devised by the Lawniczak Group to do their own research.
Project Neandersquito is just one of the ways Mara and her team are using genomics to advance the fight against malaria. A different project, the Malaria Cell Atlas, is providing new genetic data that could inform the effort to make better malaria drugs and vaccines. Another project is designed to make it easier and cheaper to identify a mosquito’s species using its DNA—it’s surprisingly hard to do just by looking—as well as whether it’s carrying the parasite that causes malaria, and even which species of the parasite it has. Ultimately, the project’s goal is to help governments get data that will help them get the most out of their anti-malaria efforts.
Mara would be the first to say that these are just a few examples of the tools the world needs to eradicate malaria. It’s going to take global cooperation from governments, the private sector, and academia. And now we can add natural history museums to the list.

Guest post
The malaria geneticist cultivating the next generation of African scientists
Why Dr. Charles Wondji moved from a prestigious UK university to open a lab in Cameroon.

Each year, I love sharing stories from around the world about the incredible work being done to fight malaria. Sometimes, though, those stories are best told firsthand. That’s why I invited Professor Charles Wondji—a malaria researcher, mosquito geneticist, and executive director of the Centre for Research in Infectious Diseases in Cameroon—to share his.
Dr. Magellan Tchouakui, Cameroon, Medical Entomology and Vector Control
Dr. Tchouakui is an expert in assessing the impacts of insecticides on major African malaria vectors’ abilities to survive and reproduce. He’s passionate about putting that research to use, and leads the testing of many companies’ novel insecticide formulations to improve bed nets and indoor-residual sprays.
Dr. Mersimine Kouamo, Cameroon, Functional Genomics
Dr. Kouamo employs tools such as transgenesis to “knock down” certain genes in mosquitoes, allowing her to study the genes’ functions and understand which ones enable the mosquitoes to withstand insecticide exposure. She is also a role model to younger female scientists.
Dr. Leon Mugenzi, Rwanda, Molecular Genetics of Vectors
Dr. Mugenzi’s interest is in providing and improving the tools used to control the spread of malaria. During his PhD work at CRID, he designed the first DNA-based diagnostic tool to detect metabolic resistance in mosquitoes to insecticides, which helps prolong the effectiveness of bed nets.

Target acquired
The newest weapon against mosquitoes: computer vision
The tech behind self-driving cars is also helping fight malaria.

Can computers see? The answer is complicated. I've been following the field of computer vision for decades—ever since Paul Allen and I started dreaming about what you could do with a personal computer—and we're only now reaching the point where they can really understand visual inputs. We still have a long way to go, but the ability of computers to see things is already revolutionizing many parts of our lives. It makes autonomous vehicles possible. It’s used to read x-rays quickly and accurately, and it’s what allows a mobile phone to translate street signs from one language to another.
Lately I’ve been especially enthused about a different application (and one my teenage self never would’ve imagined caring about): scanning pictures of mosquitoes.
Mosquitoes are responsible for spreading malaria, which kills more than 600,000 people every year and is a major focus of the Gates Foundation’s health work. Although scientists have learned a lot about them in the past few decades, one challenge has been especially stubborn: telling one mosquito from another. There are around 3,500 different species of them, and many look alike. Even a highly trained entomologist has to examine one for several minutes under a microscope to identify it accurately.
Why do we care about mosquito species? Most importantly, because different species can carry different diseases, and some don’t carry any diseases at all. (The ones that carry malaria belong to the genus Anopheles.) There are other differences too: Some bite people indoors, while others feed outdoors. Some dine at dusk while others take their meals during the day. And only females bite—the blood gives them the energy needed to lay eggs.
All this variation means we need different tools for different mosquitoes. For example, indoor insecticides and bednets work well against species that primarily bite indoors. But for the ones that mainly live and feed outside, you’ll need to take other steps too, such as eliminating the outdoor spaces where they breed.
Fortunately, some novel uses of computer vision are supercharging the process of identification. They’re not only helping us know our opponent, they’re helping us target its weak spots, save more lives, and move even closer to eradicating malaria.
One of the most exciting innovations is called VectorCam—an app that lets someone with minimal training identify mosquito species in a matter of seconds.
VectorCam was developed by Dr. Soumya Acharya and his team of bioengineers at Johns Hopkins University, with support from Uganda’s malaria control program, Makerere University, and the Gates Foundation. Using a smartphone, the VectorCam app, and an inexpensive lens attached to the phone, you simply take a picture of a mosquito and get it identified right away. The app can distinguish among the different species that transmit malaria. It can also determine the sex of the mosquito and, if the insect is a female, whether it has recently fed on blood or developed eggs. And with further refinement, VectorCam could identify species that carry other diseases, like dengue and Zika.

Urban invader
The world’s newest weapon against malaria? Mosquitoes
A city-dwelling mosquito threatening Africa sparks innovation in the fight against malaria.

About 10 years ago, the African country of Djibouti had nearly succeeded in wiping out malaria. The country’s leaders hoped that getting rid of the disease would help them attract new investment, development, and tourism.
Then suddenly the disease roared back. Cases surged from just 27 in 2012, to more than 73,000 in 2020—a huge number for this East African nation of just one million people.
The cause?
A highly invasive mosquito that had migrated from South Asia and the Arabian Peninsula into Africa.
This pest—the Anopheles stephensi mosquito—has now emerged as one of the biggest threats to malaria elimination in sub-Saharan Africa. Since establishing a beachhead in Djibouti, An. stephensi mosquitoes have been detected in Ethiopia, Sudan, Somalia, Kenya and as far away as Nigeria and Ghana, in West Africa. According to one study, if this mosquito is left unchecked an additional 126 million people on the continent will be at risk of malaria.
What makes An. stephensi particularly dangerous is where it has chosen to reside. Unlike other malaria-carrying mosquitoes in Africa that primarily breed in rural areas, An. stephensi thrives in urban environments. Cities are already home to 40 percent of the population in sub-Saharan Africa and continue to experience rapid growth, creating a fertile habitat for this mosquito. Making matters worse, An. stephensi has been found to be resistant to many of the insecticides used to control mosquito populations. And they bite in the evening before bedtime—not in the middle of the night like other mosquitoes—making bed nets less effective as protection.
But this story doesn’t end here.
In 2018, the government of Djibouti, in search for a new approach to combat these urban invaders, heard about a biotechnology company called Oxitec that has a potentially game-changing solution to mosquito control.
The fight against mosquitoes and the diseases they carry has always been a game of cat and mouse. Humans develop new interventions—like bed nets, insecticides, and treatments—to protect themselves from mosquitoes. Mosquitoes, meanwhile, have an incredible capacity to adapt, allowing them to eventually dodge or develop resistance to the latest control methods. Then humans respond with more innovations to outsmart the mosquitoes. And so on.
Oxitec, however, aims to change this game from cat versus mouse to mouse versus mouse. Or in this case, mosquito versus mosquito. Oxitec specializes in using mosquitoes to fight other mosquitoes. With its genetic technology, Oxitec has already developed mosquitoes to effectively combat the dengue fever–carrying mosquito, Aedes aegypti, in Brazil. Now Oxitec plans to use the same technology to help African governments control An. stephensi and reduce the spread of malaria.
Here’s how Oxitec’s technology would work against An. stephensi mosquitoes: Oxitec male mosquitoes carry a special gene to prevent their female offspring from surviving into adulthood. (Only female mosquitoes bite and spread malaria.) Released into the wild, the male Oxitec mosquitoes mate with wild female mosquitoes. All the female offspring die. All the male progeny, which don’t bite, will survive and go on to mate with other wild females. With sustained releases of male Oxitec mosquitoes, more females die off, dramatically reducing the mosquito population and the spread of malaria. After the mosquito releases stop, however, because half of the gene’s carriers (the females) cannot survive, the gene steadily declines and disappears from the mosquito population within a few generations.
Genetic technology like Oxitec’s understandably raises many questions. Is it safe? What are the lasting environmental impacts? Here’s what’s important to know:
Because it’s passed through mating, the gene the Oxitec male mosquitoes carry only targets the An. stephensi mosquitoes. It doesn’t have any impact on other insects and cannot be established in the local ecosystem. After evaluating the potential risk of genetically modified mosquitoes, the U.S. Food and Drug Administration in 2016 and the EPA in 2022 have confirmed that the Oxitec mosquitoes do not pose a threat to humans or the environment. More than one billion Oxitec mosquitoes have been released worldwide, with no negative impacts. In Brazil, the Oxitec Aedes aegypti mosquitoes have been so successful in reducing the spread of dengue fever that they are in demand by communities, governments, and businesses in Brazil. Homeowners can even buy a kit to raise the mosquitoes in their own backyards. (If you want to learn more about this technology, I encourage you to visit the Oxitec website and the Centers for Disease Control and Prevention.)
Last year, the government of Djibouti formed a partnership with Oxitec, Association Mutualis (a non-profit public health organization in Djibouti), and the Djibouti National Malaria Control Programme to use this new technology to defeat An. stephensi.
No Oxitec mosquitoes have been released in Djibouti during the current pilot phase of the project. But the government of Djibouti expects to move forward with the first releases of Oxitec mosquitoes next year in Djibouti’s capital city, where 70 percent of the population live.
This solution is being pursued with the support of the people of Djibouti. The government of Djibouti, Oxitec, and its local partners have been working together to educate and engage the public about this technology, going door to door to listen to their concerns, and ensuring all the communities’ questions have been addressed before moving forward with the release of the mosquitoes. Local support has been outstanding to date.
To end malaria, we need many new tools and innovations to reduce the burden of this disease and move the world closer to eradication. I’m excited about the potential of Oxitec’s technology to help Djibouti and the rest of Africa achieve this goal.

Welcome to Mosquito City
It’s always buzzing in Mosquito City
A city where researchers study how to repel, attract, and kill the world’s deadliest animal.

When’s the best time to kill mosquitoes?
While they’re making love—at sunset.
No kidding.
This is just one of many fascinating discoveries being made at a place called Mosquito City. Located in the swamplands of central Tanzania, the “city” is home to the world’s largest captive colony of mosquitoes used for researching ways to combat malaria and other mosquito-borne diseases. Day and night scientists work to better understand mosquito behavior (like when and where they enjoy having sex) as well as cutting-edge approaches to trap, repel, and most importantly, kill them.
I first learned about Mosquito City during a trip to Africa several years ago when I met scientists from Ifakara Health Institute, a Tanzanian health research organization which runs the site. While I haven’t had the opportunity to visit, Fredros Okumu, Ifakara’s chief scientist, offered a behind-the-scenes look at some of the research underway there in this video. If you’re wondering how they get enough blood to feed all the mosquitoes, watch for the moment when Fredros puts his arm in a cage containing more than 500 very hungry mosquitoes for a feed! (For larger mosquito colonies, too big for one human to feed, a cow is on the mosquitoes’ dinner menu.)
Mosquito City is located in a region of Tanzania that’s hot, humid, and swampy. In other words—perfect conditions for its primary residents. Malaria has been so widespread in this part of the country—once infecting 80 percent of the population—that one meaning of the name of the local town, Ifakara, is, “the place people go to die.”
Fortunately, malaria deaths are on the decline in recent years. One reason is the use of insecticide-treated bed nets, which remain one of the most effective means to control the disease. (New bed net distribution efforts like the one that just launched in Benin are helping to ensure every person at risk of malaria is protected by one.)
Still, much more needs to be done to fight the disease, especially as mosquitoes become resistant to some of the pesticides used to control them. That’s why scientists at Mosquito City are working to better understand mosquito behaviors and find ways to outsmart them.
“It's kind of a love- hate relationship. If you can't beat them, you join them for now, but then you can kill them from the inside. And that's what we try to do here at the Mosquito City,” Fredros says.
Fredros and his team are studying one of the deadliest mosquito species, Anopheles funestus. In southeastern Tanzania, it is responsible for nearly 9 out of every 10 cases of malaria even though other species of mosquito are far more common. And yet, it is one of the least understood species of mosquitoes because it is difficult to raise in a lab environment. Our foundation is supporting the Ifakara Health Institute’s research into its behavior so they can mount a targeted campaign against them.
One promising approach may be killing them while they are mating. Ifakara scientists learned that mosquitoes, including Anopheles funestus, have favorite locations—like rice fields, trash heaps, and banana trees—to mate. The male mosquitoes appear at their favorite mating spots at sunset to begin a ritualistic flight dance, drawing in the females. Because these mating events occur at predictable times and locations, researchers are experimenting with regularly targeting these swarms with pesticides, dramatically reducing the mosquito populations and malaria transmission.
As the researchers dig deeper into the unique characteristics of different mosquito species, it’s become more important to be able to quickly identify them. Once they understand which species is posing the greatest threat, they can choose the best methods to eliminate them. But identifying mosquito species and other indicators, like age, can be a laborious process. At Mosquito City, scientists are working on some alternative identification approaches that would accelerate their research. One is to use their buzzing sound to identify them. Another option uses infrared spectroscopy. Mosquitoes have a unique electromagnetic signal. By crushing the abdomens of mosquitoes and analyzing them under a spectrometer, researchers can identify the species and age of the mosquito.
Many of the innovations coming out of Mosquito City are designed to meet the immediate needs of the local community, who work in small farming villages and spend most of their day outdoors. Researchers have developed a variety of mosquito traps, some mimicking the odor of sweaty feet, a smell that mosquitoes find irresistible. They’ve created a range of mosquito repellents too, including furniture treated with repellent that allows people to sit outside in the evening and stay protected. They’ve even developed a line of sandals which will keep mosquitoes at bay from the sweatiest feet, protecting their owner from bites.
What will the team at Mosquito City think of next? I can’t wait to find out.
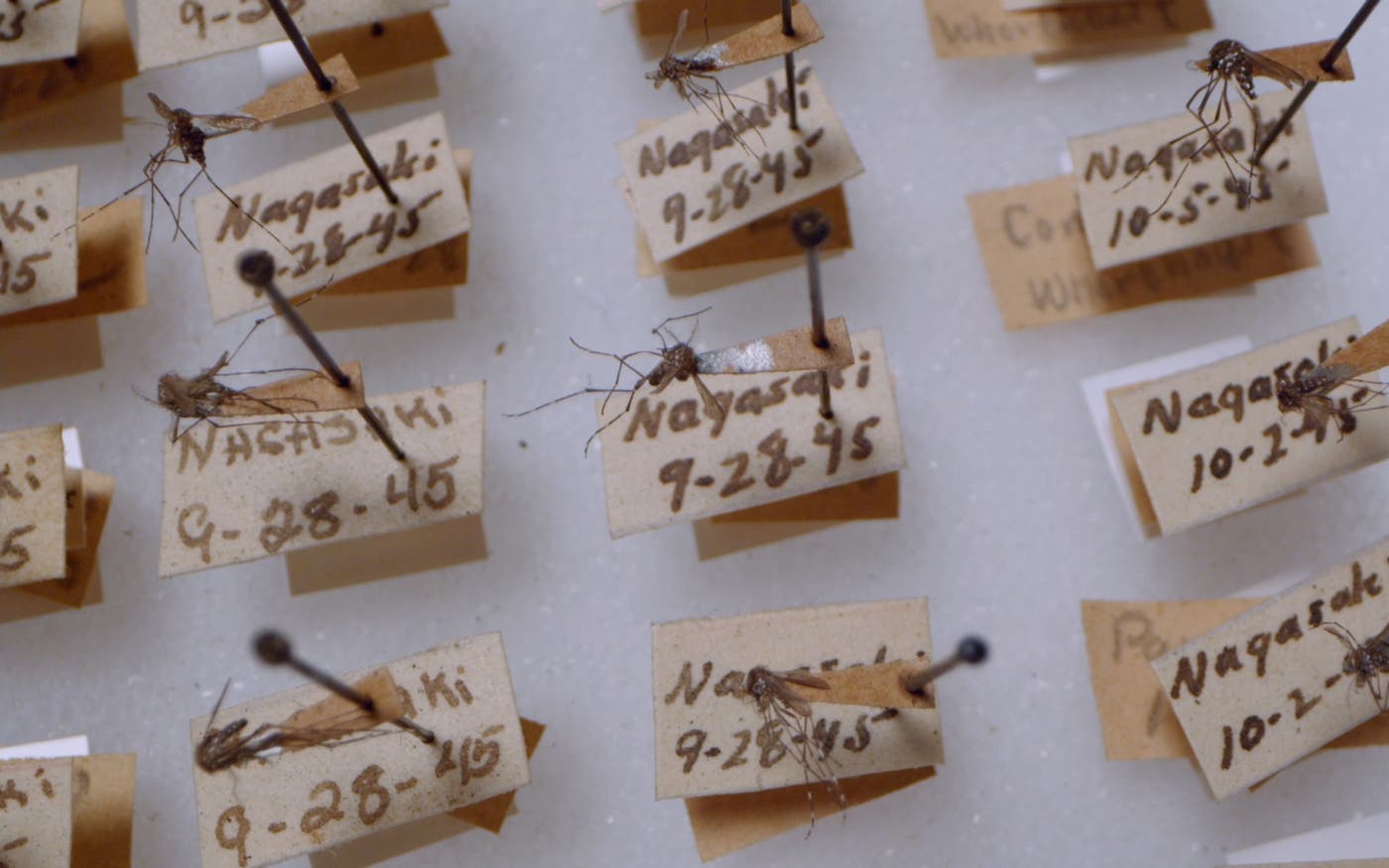
Know your enemy
The U.S. military versus the mosquito
Finding ways to protect soldiers from mosquitoes is a top priority at the Walter Reed Army Institute of Research.

The most dangerous foe U.S. soldiers may have ever encountered is the mosquito, which has caused more casualties than bombs or bullets during the nation’s conflicts.
One of the first military expenditures by the Continental Congress was $300 for quinine to protect General George Washington’s troops from malaria. During the Civil War, there were over a million cases of malaria in Union troops alone. In World War II, there were nearly 700,000 cases of malaria. In Vietnam, 50,000 cases. And more recently, of all the American soldiers deployed in Afghanistan, one out of every 20 of them battled malaria.
Finding ways to protect soldiers from the mosquito—the world’s deadliest animal—is a top priority at the U.S. Department of Defense’s Walter Reed Army Institute of Research (WRAIR).
I expect most people have never heard about WRAIR—or, if they have, they may be confusing it with the more familiar but separate institution, the Walter Reed National Military Medical Center, where U.S. presidents visit wounded troops and go for medical treatment.
It’s too bad more people don’t know about the work being done at WRAIR. Since its founding in 1893, WRAIR has been a global research leader into new malaria drugs, mosquito control, and more recently, vaccines, to protect people from mosquito-borne diseases. This research benefits the lives of not only American soldiers, but also billions of people living in areas where mosquito-borne diseases are a threat. That’s why our foundation collaborates with WRAIR on a range of research projects in malaria and other diseases that endanger the lives of people living in some of the world’s poorest areas.
Here’s one of many incredible facts that speak to WRAIR prominence in malaria research: WRAIR has contributed to the discovery and development of all FDA-approved malaria drugs, including primaquine, mefloquine, atovaquone/proguanil (Malarone), tafenoquine, and doxycycline. If you’ve ever traveled to an area where malaria is prevalent you’ve probably been prescribed one of these drugs for protection. And because of the spread of malaria drug resistance, WRAIR continues to explore new drugs to stay one step ahead of this threat.
WRAIR, in partnership with the Smithsonian Institute, also manages the world’s largest mosquito collection, which currently has more than 1.7 million specimens. Some of the oldest were collected by Walter Reed, the Army major who helped discover that yellow fever is transmitted by mosquitoes. WRAIR is named in his honor.
This large mosquito collection allows WRAIR researchers to “know their enemy,” by giving them a deep understanding of the huge variety of mosquito species that populate the globe so they can mount the most effective defenses against them.
The first line of defense for soldiers is their clothing and WRAIR has developed uniforms treated with insecticides to protect them. Then, there are mosquito nets and various repellents, including ones that double as camouflage paint.
Highly effective vaccines against malaria and other mosquito-borne disease are also a priority at WRAIR. WRAIR developed the first-ever malaria vaccine in conjunction with GlaxoSmithKline. Researchers at WRAIR also led the development of a Zika vaccine.
One of the most surprising and important areas of research at WRAIR are the human malaria infection challenge trials. As part of this program, WRAIR recruits volunteers who agree to be bitten by malaria-infected mosquitoes, exposing themselves to a curable form of the disease to test the effectiveness of various interventions. This might sound scary, but the trials are extremely safe. The volunteers are carefully monitored and are quickly cured before they become too ill. In the last 30 years, WRAIR has performed over 100 trials on over 2,200 volunteers. Thanks to this research, WRAIR has greatly accelerated the development of experimental vaccines and malaria drugs.
What’s most exciting at WRAIR is the research that will help us all prepare for the threats of the future, including climate change, which will increase the spread of mosquito-borne diseases.
As Col. Brian Evans, WRAIR’s chief entomologist, says, “The challenge is always evolving and the role of WRAIR is to keep up with that, to stay ahead of the game.”
Thanks to their incredible work for more than 125 years, WRAIR has done just that.

Releasing Hope
This factory breeds 30 million mosquitoes per week. Here’s why.
These mosquitoes are allies in the fight against dengue and other deadly viruses.

Inside a two-story brick building in Medellín, Colombia, scientists work long hours in muggy labs breeding millions and millions of mosquitoes. They tend to the insects’ every need as they grow from larvae to pupae to adults, keeping the temperature just right and feeding them generous helpings of fishmeal, sugar, and, of course, blood.
Then, they release them across the country to breed with wild mosquitoes that can carry dengue and other viruses threatening to sicken and kill the population of Colombia.
This might sound the beginnings of a Hollywood writer’s horror film plot.
But it’s not.
This factory is real.
And the mosquitoes being released don’t terrorize the local population. Far from it. They’re actually helping to save and improve millions of lives.
Here’s how they do it: The mosquitoes being produced in this factory carry bacteria called Wolbachia that block them from transmitting dengue and other viruses, such as Zika, chikungunya and yellow fever, to humans. By releasing them to reproduce with wild mosquitoes, they spread the bacteria, reducing virus transmission and protecting millions of people from illnesses.
I’ve written before about these amazing Wolbachia mosquitoes, including last year when a new study showed how effective they could be in preventing diseases. The randomized controlled trial conducted in Yogyakarta, Indonesia, found that Wolbachia-carrying mosquitoes reduced the number of dengue cases in the city by 77 percent and dengue hospitalizations by 86 percent. In a new study in Medellín, dengue cases have declined by 89 percent since Wolbachia mosquitoes started being released in 2015.
These results are a huge breakthrough, offering proof that this new technology will protect entire cities and countries against the threat of mosquito-borne diseases. The World Mosquito Program, which is leading the Wolbachia effort, is now releasing these mosquitoes in 11 countries: Brazil, Colombia, Mexico, Indonesia, Sri Lanka, Vietnam, Australia, Fiji, Kiribati, New Caledonia, and Vanuatu.
And what’s remarkable about the Wolbachia mosquitoes is that once enough of them are released to offer disease protection, it’s a solution that’s self-sustaining. Over time, families will be spared the heartbreak of losing loved ones and communities won’t need to spend money on prevention and treatment for these mosquito-borne diseases, freeing up funds for other health priorities.
The World Mosquito Program aims to spread Wolbachia among Aedes aegypti mosquitoes, a tropical mosquito that is a host for dengue, yellow fever, and other viruses. (Malaria is spread through a parasite carried by the Anopheles mosquito and is not a focus of the Wolbachia effort.) With climate change, there is an urgency to the World Mosquito Program’s work. As global temperatures rise, Aedes aegypti mosquitoes, are finding more regions of the world habitable, increasing the spread of these diseases. The biggest risk is posed by dengue, which infects more than 400 million people each year and kills 20,000.
The demand for these lifesaving mosquitoes continues to grow and that means the World Mosquito Program needs to produce hundreds of millions of Wolbachia mosquitoes. That brings us back to the factory in Medellín, which is currently the world’s largest mosquito breeding facility in the world, producing more than 30 million mosquitoes per week. Other World Mosquito Program sites around the world are also breeding Wolbachia mosquitoes, but Colombia’s is currently the largest.
Until now, killing or repelling mosquitoes with insecticides, bed nets, and traps has been the priority, not mass producing them. As difficult as it is to kill mosquitoes, raising them by the millions may be even harder. Mosquitoes must be bred, fed, and housed under ideal conditions for them to grow and reproduce. The factory in Medellín has been perfecting the process and improving its efficiency so they can breed and release Wolbachia mosquitoes on a large scale.
The centerpiece of the mosquito factory is a colony of Wolbachia mosquitoes, called the brood stock, from which all future populations of Wolbachia mosquito offspring are bred. The brood stock offspring are then raised to create millions of eggs, which hatch when put in water and become larvae. Fed with fish meal, the larvae grow to become pupae, which then become adults. To thrive, adults need sugar (check out this story about how researchers in Zambia are exploiting mosquito’s craving for sugar to create a new bait that will control the spread of malaria) and blood, which the team sources from expired stocks at blood banks.
Once the factory has bred millions of eggs and adult mosquitoes, they are ready to be released. The eggs are packaged in small gelatin capsules, each containing 300 eggs, which are given to residents to drop in water to hatch. The advantage of egg releases like this is that the eggs can easily be transported long distances and they can be hatched as needed. The factory also releases adult mosquitoes by the thousands from the back of motorcycles roving the city. The World Mosquito team is also experimenting with releases from drones. The adult releases allow the Wolbachia mosquitoes to immediately begin mating with the wild mosquito population and spreading the virus-blocking bacteria.
It’s exciting to see how far the World Mosquito Program has come. Years ago, the idea of releasing mosquitoes as an ally in the fight against diseases struck many people as crazy. But support for this innovative solution has caught on in communities around the world. These amazing mosquitoes are taking flight and saving lives.

The nose knows
Could perfume be our secret weapon in the war on mosquitoes?
Mosquitoes use their sense of smell to find new victims. A Swiss fragrance company is hoping to thwart them.

Are you a mosquito magnet? If you don’t seem to get your unfair share of mosquito bites every summer, chances are you know someone who does. Some people are just more attractive to the pests than others.
The reason why is probably how you smell. Mosquitoes rely on their sense of smell to find their targets, and they’re drawn to certain odors naturally produced by the human body. Although some people may be a little more attractive, the unfortunate truth is that we all smell like a delicious meal to mosquitoes. You can hide yourself for a while using a bug spray like DEET or treating your clothes with permethrin. But if you want sustained protection, you have to add another step to your routine, which not everyone has the time to do or can afford.
There’s good news on the horizon, though: A company called dsm-firmenich is working to make repelling mosquitoes as easy as washing up in the morning.
I actually visited dsm-firmenich’s lab in Geneva back in 2016, when I checked out their innovative work to improve sanitation for the world’s poorest by reducing toilet odors. The nutrition, beauty, and health company is one of the world’s largest manufacturers of flavors and fragrances. Most of their products are used to make our food taste better and our household products smell more appealing, but they also have a history of using their scent expertise to fight disease transmission. Their latest efforts are focused on stopping mosquitoes, because the diseases they carry kill hundreds of thousands of people each year, most of whom are children in low-income countries.
The team’s goal is simple: Incorporate scents that repel mosquitoes into everyday products. After doing extensive research into the household products used most frequently in places where mosquito-borne diseases are common, they decided to focus mostly on bar soap and powdered laundry detergent. (They’re also thinking about other things like body lotion and body cream.) These products are already scented with a fragrance—what if that fragrance also helped keep mosquitoes away?
The idea is that you gain an added halo of protection without having to add any new steps to your daily routine or buy any new products. No one at dsm-firmenich thinks this kind of protection will be a silver bullet, but their hope is that, when combined with other proven tools like bed nets, people can significantly and sustainably lower their risk of catching deadly diseases like malaria and dengue.
Making a bar soap that gives you all-day protection against mosquitoes is a lot more complex than just infusing it with citronella. The scientists in Geneva started by identifying a wide array of scent ingredients that keep the pests away and are commonly used to create perfumes. Some of these ingredients are true repellants, giving off a smell that causes mosquitoes to fly in the opposite direction. Others block receptors in the mosquito’s brain that usually perceive and draw them to humans.
As they were combining the ingredients to create new fragrances, the team knew they had to keep a human-centered design approach in mind. The best candidates wouldn’t necessarily be the most effective—they also had to smell clean and fresh. I love the smell of cheeseburgers, but I don’t think I’d want my laundry to smell like them every day even if they protected me from mosquitoes!
To test the most promising odors, researchers used a tool I know all too well: The arm-in-cage test, where a human puts their arm—which has been coated in the fragrance being studied—into an enclosed area filled with hundreds of mosquitoes. Sensors track how the mosquitoes respond and whether they’re biting the arm. The team considered any test with two mosquito bites a failure.
Behavioral tests like those being done in collaboration with the Swiss Tropical and Public Health Institute are still ongoing, but they’ve already revealed some surprising results. One of the most effective fragrances so far smells like lily-of-the-valley, a light floral scent that is commonly used in perfumery. It’s exactly the kind of fresh scent that people like in their soaps and laundry detergents. The team’s early results indicate that some lily-of-the-valley odors could be as effective as DEET when used at certain doses.
The next step is the most difficult, and it remains to be seen whether it will succeed. The mosquito experts at dsm-firmenich have handed off the best scent candidates to the company’s product formulation experts and perfumers, who are now looking for ways to make them last all day in consumer products.
It’s a tall order. Scent ingredients are fragile, and activities like scrubbing your hands or washing your clothes cause them to vanish quickly. (Think about how quickly that freshly laundered smell can fade from your clothes.) A perfume that protects you from mosquitoes all day will likely end up being the result of a whole lot of innovation and a complex combination of different scents, rather than one single ingredient. And, of course, the final result has to smell good enough that people are willing to use it every day.
Still, I’m optimistic the scent wizards in Geneva will find a way. The Gates Foundation is supporting their research with the hope that, one day, people in high-risk areas will gain more mosquito protection without having to do any extra work or spend any extra money. When the world gives children and families more tools to protect themselves, we save lives—and take the bite out of the world’s deadliest animal.

Sweet dreams
Sugar Fix
Mosquitoes love blood, but did you know they have an even bigger sweet tooth?

Everyone knows mosquitoes have a taste for blood, but did you know they have an even bigger sweet tooth?
Mosquitoes love sugar.
Just as humans are drawn to the sweet smell of a chocolate shop or bakery, mosquitoes find the smell of sugar irresistible.
All mosquitoes need sugar to survive. Female mosquitoes consume blood to lay eggs, but both male and female mosquitoes require sugar for energy. In fact, even though mosquitoes buzzing in your ears may appear single-minded about biting you, they need sugar more often than they need blood.
Exploiting this craving, researchers have developed a lethal new tool to kill mosquitoes and protect people living in areas at high risk for malaria and other mosquito-borne diseases.
Here’s how it works: In nature, mosquitoes get sugar from flower nectar and plants. But scientists have developed a tempting bait that lures mosquitoes with a highly attractive fruit scent. When they land on it to get their sugar fix, the mosquitoes begin feasting on a sweet meal laced with insecticide. Not long after, they drop dead, reducing mosquito populations and, researchers hope, the spread of malaria in the communities where the traps are used.
While other insects, like bees and butterflies, may also be drawn to the bait’s sweet scent, the bait is just lethal for mosquitoes. A protective membrane, only accessible to mosquitoes, covers the bait and prevents other insects from feasting on the deadly meal inside.
This new mosquito control tool, called Attractive Targeted Sugar Baits or ATSBs, developed by Westham Co., is simple to use, affordable, and has the potential to be a game changer in the effort to eradicate malaria.
And it couldn’t arrive soon enough.
Over the past two decades, the world has dramatically reduced the global burden of malaria, preventing 1.7 billion cases and saving 10.6 million lives. This progress has been attributed, in large part, to the widescale use of long-lasting insecticide-treated bed nets, which protect people from bites while they sleep, and indoor residual spraying, which kills mosquitoes that land on insecticide-treated walls and ceilings in homes.
As effective as these tools have been, both mosquitoes and the malaria parasite are constantly evolving, sometimes making these interventions less effective. We’ve seen this again and again with resistance to insecticides and malaria drugs. And that’s why it’s critical that the world continues to innovate with new ways to prevent the spread of malaria.
In response to the widespread use of bed nets and indoor insecticide spraying, mosquitoes have changed their behaviors, according to some researchers. In some areas, instead of seeking their blood meals only inside homes after bedtime, malaria-carrying mosquitoes are now biting outside homes, and earlier in the evening, when people will often cook and socialize.
And this is how the sugar baits fit in.
By attracting mosquitoes outside, sugar baits offer a highly effective mosquito control tool for households. About the size of a sheet of notebook paper, sugar baits can be easily installed with a hammer and a nail. Two baits hung on the adjacent outside walls of a home are enough to offer months of protection.
In studies conducted in Mali in 2016 and 2017 researchers found that the sugar baits dramatically reduced mosquito populations and malaria cases in the communities where they were used.
A more recent modeling analysis predicted that sugar baits, when used to complement long-lasting insecticide-treated bed nets and indoor spraying, could reduce malaria cases by 30 percent in areas with high malaria burdens.
In 2020, there were an estimated 241 million malaria cases. A 30 percent reduction in malaria cases would be a huge breakthrough and save many lives.
That’s why our foundation has been supporting the development of sugar baits, including sponsoring a large-scale field trial currently underway in Kenya, Mali, and Zambia. So far, the results have confirmed the effectiveness of the bait stations.
If all goes well with the trials, sugar baits could be available for widespread use as soon as next year.
No need to sugarcoat it. For the millions of people at risk of malaria around the world, that would be welcome news.

Benin in front
Full coverage: Bed nets for Benin
Its bed net distribution system will help save lives from malaria and other diseases too.

If you’ve ever traveled to a part of the world where there’s a risk of malaria or other mosquito-borne disease, you probably slept under a mosquito net.
The gauzy fabric creates a physical barrier that protects you from mosquitoes. At the same time, you serve as bait in a deadly trap. Treated with potent insecticides, the net kills mosquitoes that land on it during their futile efforts to bite you.
It’s a remarkably simple tool, but it’s proven to be one of the most effective weapons we have against malaria. Increased bed net use is largely responsible for the more than 50 percent drop in malaria deaths worldwide since 2000.
Still, more needs to be done to ensure that communities at highest risk of malaria have access to them.
That’s why I’m excited that the government of Benin this year launched a new, innovative approach to distributing bed nets to their population.
Using smartphones, real time data collection, satellite mapping and other surveillance techniques, Benin’s distribution program will give health officials the data they need to provide full bed net coverage to the country.
Benin is faced with one of the highest burdens of malaria in the world. The West African country of nearly 12 million people has about 2 million cases each year. If successful, this new bed net distribution effort will save thousands of lives and serve as a blueprint for other high burden malaria countries to follow.
As you might imagine, distributing bed nets to every household is a massive logistical effort involving thousands of people—from truck drivers to health workers. And the job is made even harder in Benin where exact population numbers are uncertain.
For many years, Benin’s distribution campaigns were run with pencil and paper systems. Health officials used thick ledgers to keep track of the names and addresses of residents and how many beds nets they needed. It was time-consuming and often inaccurate. No one knew exactly how many nets would be needed or if they reached their intended destinations. As a result, many families were missed during the distribution, putting them at higher risk of malaria because they lacked the protection of a bed net.
But this year’s distribution is different. In partnership with Catholic Relief Services and our foundation, Benin’s national malaria program created a new, digitized distribution system that is more accurate and efficient in getting bed nets into the homes of all households in the country.
In many ways, this effort is based on the lessons the global health community has learned in the fight against polio. As vaccinators sought to immunize every child against polio in India and Nigeria, they would sometimes miss households, especially in remote areas. But with satellite mapping and better data collection, health workers were able to quickly identify gaps in vaccination coverage and reach every home.
Benin’s new bed net distribution operates in much the same way. Walking door to door, health workers make home visits throughout the country and perform a brief census: the number of people living there, including number of children and pregnant women, number of bed nets needed, etc. Using cell phones, they enter this information into a database. They also give each household a uniquely coded voucher to redeem at a nearby distribution center where they can collect their bed nets.
On the distribution day, people come to collect their nets and get lessons on the proper way to set up and care for them. As people arrive to redeem their vouchers for the nets, the malaria team has real time data on which households have received their nets and which ones have not. This data—which can be reviewed on a digital map—allows the malaria team to quickly identify any problems with their delivery system. It also gives health workers detailed information about which households need to be targeted for follow up to ensure they all have nets.
I admit none of what I’ve just described may sound that revolutionary. But in global health, I’ve learned again and again that saving lives is the result of getting the smallest details—from the temperature of a vaccine to the address of a beneficiary—right. And Benin’s new digitized bed net distribution program does just that by giving the government a powerful tool to manage a complex job.
And with this new digital distribution system in place, Benin can use it as a platform to manage other big health campaigns—like vaccinating against meningitis and door-to-door efforts to eliminate neglected tropical diseases.
I’m looking forward to hearing more about Benin’s progress in the fight against malaria and other diseases because of this new system—and I hope other countries will learn from their success.

Ancient country, new ideas
India’s innovations are still changing the world
I’m excited to see the latest breakthroughs during my visit this week.

I’ve been visiting India since the 1990s, and I’m on my way to visit again this week. Over the years, I’ve learned about its rich history and visited some of its stunning monuments, including the Taj Mahal.
But when I think about India’s most important contributions to the world, these are not the first things that come to mind. India’s greatest gift is its ability to innovate.
This country has a long history of important breakthroughs. (Mathematicians in ancient India are widely credited with introducing the decimal system for numbers.) More recently, India has made advances that are saving and improving millions of lives in India and around the world. The Gates Foundation has been a partner in some of these efforts, and I’m visiting this week to learn about how we can continue working with India to help its ideas and inventions reach everyone who needs them, no matter where they live. This will be a main topic when I meet with Prime Minister Modi this week.
Health is one area where India is making a big difference. This country is the world's largest producer of vaccines—it supplies more than 60 percent of all vaccines distributed by Gavi, the organization that has helped vaccinate more than 1 billion children in lower-income countries. Indian companies pioneered the creation of high-quality, low-cost vaccines and drugs, leading the world in making affordable treatments for diseases like HIV/AIDS as well as vaccines for rotavirus, pneumococcal pneumonia, and COVID. The government has helped deliver huge supplies of vaccines to its own people and to other low- and middle-income countries, and now it’s looking to do the same for medical devices and diagnostics.
Thanks in large part to India, developing countries now get new medicines and vaccines much faster than they used to. I rank these efforts as one of the most important health achievements ever. (We’ve made progress, but we’re not done. The world should still do more to shrink the gap between when a drug or vaccine becomes available in rich countries and when it reaches lower-income ones.)
Another area where I admire India’s innovative spirit is what’s known as digital public infrastructure, or DPI. In short, DPI refers to the digital platforms and tools that help deliver various services. India’s biometric identity program, Aadhaar, covers more than 1.4 billion people, allowing them to take advantage of all kinds of government services without needing a photo ID. UPI, a digital payment system that ensures that the person you’re doing business with is who they say they are, processes more than 12 billion transactions a month.
During my trip I’ll get to see India’s DPI in action. I’ll visit an agricultural monitoring center in the state of Odisha where government officials use DPI to give farmers real-time guidance. Thanks to Aadhaar, this center is able to maintain a registry of 7.5 million farmers—even if they don’t own land—and their crops, so officials can keep track of who is growing what (and, therefore, what kind of farming advice they need). It has also developed a chatbot that makes it easy for farmers to get the latest information about their crops, using AI to tailor content to their particular needs and in their local language.
This service’s pest-management program now reaches more than 4 million farmers, and since it began in 2018, the volume of crops that participating farmers lose to pests every year has dropped by 90 percent. Now others—including other states in India as well as Ethiopia, Sri Lanka, and the World Bank—are looking to learn from Odisha’s experience with this service as well as its biometric ID and digital payments systems.
I'm also looking forward to learning more about how India is addressing urban poverty, especially among women. It has one of the fastest-growing urban populations in the world, and more than 100 million people there live in slums, where it’s hard and often impossible to get even basic services like health, education, and clean water. Women are particularly vulnerable because they face discrimination and violence.
This week, I’ll visit a low-income community in Odisha where a government program is helping women get the skills to fulfill government construction contracts. Since 2018, this program has helped 22,000 groups of women deliver on more than 52,000 projects including building roads, drains, and toilets.
This program could be a model for other countries that are facing similar challenges. The women who participate in it are partners in creating the projects: They get training in engineering, accounting, negotiating contracts, and other skills, and they’re involved in planning the project, making a budget, doing the construction, and doing maintenance on whatever they build. I'm looking forward to meeting a few women who are part of this program so I can hear about the challenges they face and the successes they’ve had.
India’s capacity to innovate will also become increasingly important to stopping climate change. Indians are already being affected by higher temperatures and less-predictable weather, and eliminating the greenhouse gases that are causing the problem is a huge scientific challenge. So it’s great that India is ramping up its ability to invent, manufacture, and deploy climate breakthroughs. The government is investing in research to raise the productivity of crops and livestock even in a warmer climate, and it’s expanding its plans for clean energy.
These are just a few of the ways in which India's innovations are changing the world. I could list many more, and I’m sure I’ll learn about a few new ones during my visit. I’m looking forward to speaking with government leaders, CEOs, and students who will drive innovation in India. This country has a lot to offer, and I'm optimistic that it will continue to lead the way in creating a more equitable world.

Exemplary
Lessons in lifesaving from Brazil
What the biggest country in South America can teach the world about healthcare.

I’ve been a big fan of Brazil for a while. I first visited back in 1995 when Microsoft was building out our operations there, including working with one of the national banks to launch home banking. And some of my favorite family trips have been to the Amazon, whose river, basin, and rainforest come up often during conversations on climate change. But it wasn’t until I began working in public health that I started appreciating just how impressive the country’s track record in this area is—and how much the rest of the world could learn from it.
In roughly three decades, Brazil has cut maternal mortality by nearly 60 percent, slashed under-five child mortality by 75 percent—far outpacing global trends—and increased life expectancy by almost a decade. None of these achievements was accidental. Instead, they’re the result of long-term, laser-focused investments Brazil has made in its primary healthcare system that other countries can learn from and emulate.
The story starts in the late 1980s. Two decades under military dictatorship had turned Brazil into one of the least equitable countries in the world. In 1985, the country became a democracy; a few years later, it created a universal health system.
In the decade that followed, deaths from non-communicable diseases and maternal, neonatal, and nutritional causes all started to decline, and life expectancy rose. With an increase in primary healthcare services, even hospitalizations dropped.
But it’s one thing to guarantee healthcare. It’s another thing to fund it—and another thing entirely to make sure it reaches the people who need it most. While Brazil had been making progress, there was much more to do. So at the turn of the century, the government accelerated its efforts and took steps to close the gaps in its healthcare system, including a dramatic increase in healthcare spending. One of the most important steps was massively expanding the size and scope of its community health worker (CHW) program.
Community health workers are trained public health professionals who work within communities, especially in remote or underserved areas. While their roles vary around the world based on local needs, they generally include things like disease tracking, vaccine drives, and basic health screenings.
In Brazil, CHWs had already shown they could improve public health access and outcomes during a pilot program in the Ceara state. As federal funding for primary healthcare increased, almost fivefold in fifteen years, the ratio of CHWs tripled.
Today, Brazil has over 286,000 CHWs who serve almost two thirds of the population—almost 160 million people. Each one visits about 100-150 households a month, offering guidance on health and hygiene, advocating for preventive care, following up after medical appointments, collecting socioeconomic data, and helping people navigate other government services.
In Brazil, CHWs act as the front door to the world’s largest universal free public healthcare system, and their impact has been transformative. They’re credited with further cutting child mortality and pushing immunization coverage to near-universal levels. (Unfortunately, the pandemic impacted vaccination rates, but there are efforts underway to bring them back up.)
The country’s Bolsa Familia program—which provides cash transfers to poor families if they meet certain conditions, including vaccination for children and prenatal care—deserves credit too. Expanded in tandem with primary healthcare, Bolsa Familia is just one of the many social programs Brazil has built out over the past few decades that have helped lift almost a fifth of the country’s population out of poverty. But it’s also helped broaden healthcare access and usage by giving people an incentive to enter the healthcare system—which is how Bolsa Familia has contributed to reductions in child mortality as well.
I’ve been able to learn about these initiatives through the Gates Foundation's partnership with Brazil's Ministry of Health—which has focused on combatting malaria, improving vaccine production, leveraging local brainpower to address global health issues, and documenting the impact of social and health programs through data sciences. And I’ve been really impressed.
Of course, despite all the progress that’s been made in recent decades, Brazil still faces challenges. Financial crises and austerity budgets have led to cuts in healthcare spending, for example, and there are still districts where poorer residents have no access to CHWs.
But Brazil’s healthcare system doesn’t have to be perfect to serve as proof of what happens when a country invests strategically in care for its most vulnerable: The returns are often far-reaching and life-changing.
That is why Brazil is highlighted by the Exemplars in Global Health program, which I helped launch in 2020. The program's mission is to identify countries that have made remarkable progress on health problems, understand the keys to their success, and share those insights globally so others can make similar progress. By that standard, Brazil has a lot to teach.
That’s not to say any country can or should replicate Brazil’s approach exactly, since no two countries are alike. But with the right mix of investment and innovation, Brazil has made great strides in becoming a healthier place for its people. If the country continues on that path and keeps doing what it’s done well already, and if other countries follow—or simply forge their own paths with Brazil in mind—we’ll have a healthier world, too.

Rise to the challenge
5 of the coolest innovations I saw in Senegal
I got to meet with amazing scientists working on the next big breakthrough while I was in Dakar.

I had an amazing trip to Senegal last month. I always love getting the chance to travel and see the remarkable work the foundation’s partners are doing firsthand. These visits leave me more energized than ever to go to work every day—and my time in Senegal was no exception.
Senegal is a particularly interesting country to visit, because it has made exemplary progress improving the health of its people thanks to a focus on community-led care and many years of smart policymaking. Some of the statistics are mind-blowing: Since 1992, the country has cut its stunting rate in half. Since 2000, the number of Senegalese children who die before their 5th birthday has dropped by 70 percent. And since 2005, the number of women giving birth in health facilities has increased from 62 percent to 80 percent. It’s the perfect place to talk about progress.
One of the highlights of my visit was a trip to the Institut Pasteur de Dakar, or IPD—a research center that has been pushing the frontiers of global health for nearly a century. The facility does it all: IPD plays a key role in monitoring for disease outbreaks in the region; produces millions of diagnostics every year; serves as an educational hub for the next generation of health workers and biomanufacturing workers; and will soon resume manufacturing vaccines.
It was inspiring to meet with brilliant Senegalese scientists who are doing remarkable work to keep their country healthy. Senegal’s health transformation is, in large part, a testament to their dedication and deep understanding of their communities, and I loved talking to them about how they’re constantly evolving to meet the needs of the moment. For example, when COVID hit in 2020, IPD quickly built up a test manufacturing facility. They’re now in the process of expanding that capacity so they can produce other essential tests, like one for measles and rubella.
I was also excited to attend the annual meeting of the Grand Challenges initiative in Dakar last month. The Gates Foundation launched Grand Challenges 20 years ago with a single goal in mind: to identify the biggest problems in health and give grants to the researchers who might solve them. Our hope was to inspire more brilliant scientists to think more ambitiously about transforming health in low-income countries. We hoped to create a scientific community that had support to sustain R&D for the benefit of billions of people whose health needs had been neglected.
In 2003, we put forth 14 Grand Challenges. The initial list included developing a vaccine that didn’t require refrigeration, creating a TB treatment for latent infection, and inventing a needle-free drug delivery system. In the years since, we’ve issued more than 200 challenges—and we even launched our first AI-specific call-to-action earlier this year.
I was lucky to spend a lot of time in Senegal with amazing scientists working on the next big breakthrough. Here are 5 of the coolest innovations I saw:
- An AI trainer that teaches health workers in India how to treat high-risk pregnancies. Here’s a devastating statistic: One woman dies in childbirth every 2 minutes. Amrita Mahale and the team at ARMMAN are using artificial intelligence to improve the odds for new mothers in India. Their large language model will one day teach health workers how to treat high-risk pregnancies. The training chatbot can be used in both English and Telugu, and the coolest part is that it automatically adjusts to the experience level of the person using it. Whether you’re a brand-new nurse or a midwife with decades of experience, ARMMAN’s trainer can arm you with the knowledge needed to save lives.
- A low-cost mRNA vaccine platform that puts manufacturing where it’s needed most. mRNA vaccines helped prevent millions of deaths during the height of the COVID pandemic. A company called Quantoom developed a new platform that will make it cheaper and easier to build and run factories that can be adapted to make different mRNA vaccines. I was proud to announce that the foundation is investing $40 million to scale up local mRNA vaccine manufacturing in low- and middle-income countries—which includes funding for IPD to use Quantoom’s platform. This will increase supply, lower costs, guard against the possibility of vaccine hoarding in emergencies, and provide a path for local scientists to discover and develop their own vaccines.
- A new way of tracking mosquitoes on the molecular level to stop malaria. Cases of mosquito-borne diseases like malaria are increasing for the first time in decades. Although climate change is a big contributor, other reasons include conflicts and drug resistance. Fortunately, Isabella Oyier at the Kenya Medical Research Institute is fighting back against mosquito evolution. She uses molecular epidemiology to track mosquitoes who have the genes that cause drug resistance and integrate it into national malaria surveillance and monitoring efforts. This will give stakeholders more insight into where resistance is spreading—and how to stop it.
- A novel approach to treating a common microbiome disorder. Our bodies are home to more microbial cells than human cells, and the good bacteria in our microbiome play an essential role keeping bad bacteria in check. When that balance is off, you get diseases like bacterial vaginosis—a common disorder that, among other problems, can make women more susceptible to HIV infection or more likely to give birth preterm. Today’s treatments are not very effective, so I was excited to talk to Meilin Zhu and her team about a new approach they’re exploring. It uses oleic acids to inhibit the growth of a “gateway” bacteria that can lead to more bad microbes, as well as promote the growth of the good bacteria. This research is still in its early stages, but it’s promising.
- A new drug development platform that will make us better prepared for the next pandemic. Although the world made remarkable progress on vaccines when COVID struck, the same can’t be said for therapeutics. The team at Decoy Therapeutics is working to speed up the process of developing drugs with their promising new biologic platform. The idea is that lipopeptide molecules could be used to inhibit a virus’ fusion machinery and prevent it from infecting cells. If Decoy’s research pans out, scientists could one day use the platform to design therapies for novel viruses within days or even hours.
My time in Senegal reaffirmed my belief in the power of science and innovation. There is no question that our world faces some difficult problems. But when brilliant scientists dedicate their talents to taking on the world’s biggest challenges, progress becomes possible, and we move closer to a future when all people lead healthy lives.
The big picture
On the road in Nigeria and Niger
These were some of my favorite moments from the last week in West Africa.

Have you ever visited a place you haven’t been in a while, and it somehow manages to feel both new and familiar? That’s how I feel every time I go back to Nigeria.
It was amazing to return to Lagos and Abuja this week. I’ve been fortunate to spend a lot of time in Nigeria over the last two-plus decades, but it’s been nearly five years since my last visit due to the pandemic. Nigeria—and especially Lagos—is one of the most dynamic, vibrant places in the world, and I am always blown away by how much it's changed. At the same time, I loved getting to catch up with old friends and reconnect in person with longtime partners. (Remote meetings are great, but it’s nice to meet face-to-face on occasion.)
This week also marked my first-ever trip to Niger. Our foundation has been working with talented Nigeriens for years to help ensure children's health and prevent the spread of polio, and it was exciting to see the country for myself and talk about the future of that work.
It was a great week. These were some of my favorite moments:

Photo Album
My trip to India in pictures
Why my travels in India made me optimistic about the future.

I just returned from my visit to India, and I can’t wait to go back again.
I love visiting India because every trip is an incredible opportunity to learn.
During my travels last week in Mumbai, Delhi, and Bangalore, I met some amazing people, including political leaders, bureaucrats, philanthropists, and scientists, who taught me how they are using the power of innovation, science, and collaboration to find solutions to the world’s health, climate, and development challenges.
Along the way, I met a teen bridge champion, had fun conversations with two of India’s most popular YouTubers, and I even drove an electric rickshaw!
But instead of telling you about it, let me show you. Here are some photos from my trip and some of the stories behind them:

Multitasking
My message in India: To fight climate change, improve global health
Climate change and global health are inextricably linked. We need to make progress on both problems at the same time.

I’m headed back to India next week. Although I’ve spent a lot of time there over the years—doing everything from checking out toilets to visiting a village that’s home to the one poorest, most underserved castes in India—I haven’t been back since before the pandemic. I can’t wait to see how much progress has been made in that time.
This essay originally ran in the Times of India and Dainik Jagaran. You can read it here:
More than two decades ago, I set out to give the vast majority of my resources back to society. My goal from the beginning was to help reduce the awful inequities I saw around the world.
When I started this work, my biggest focus was global health, because it’s the worst inequity in the world and it’s a solvable problem. That’s still the case today. But as time went on—and as the disastrous consequences of a warming world became more evident—it became clear that you can’t improve life for the world’s poorest without also tackling climate change.
Climate change and global health are inextricably linked. Hotter temperatures will make poverty reduction harder by increasing food insecurity and the prevalence of infectious diseases and diverting resources away from those who need them the most. It’s a vicious cycle. The poorer a community is, the more vulnerable it is to climate change. And the more impacted a community is by extreme weather events, the more entrenched in poverty it becomes. To break the cycle, we need to make progress on both problems at the same time.
When I talk to people about this, I often hear the same response: “There isn’t enough time or money to solve both at the same time.” But this idea that we can only tackle one thing at a time is just wrong. I’m stubborn in my belief that with the right innovations and delivery channels to get them to the vulnerable, we’re capable of making progress on lots of big problems at once—even at a time when the world faces multiple crises. There is no better proof than the remarkable progress that India has accomplished.
Consider the field of next-generation chickpea plants currently growing at the Indian Agricultural Research Institute, or IARI, in Pusa. Chickpeas are a staple crop in India. They provide an important source of income for many smallholder farmers, and families across the country rely on them for nutrition. But the chickpea harvest is threatened by climate change. Higher temperatures could reduce yields by as much as 70 percent, putting lives and livelihoods at risk.
So, the Gates Foundation joined hands with India’s public sector and CGIAR institutions to support the work of researchers at IARI. They found a new solution: chickpea varieties that have more than 10% higher yields and are more drought-resistant. One variety is already available to farmers, and others are currently in development at the institute. As a result, India is better prepared to keep feeding its people and supporting its farmers even in a warming world. It’s no exaggeration to say that India’s agricultural future is growing right now in a field in Pusa.
One of the reasons why challenges like climate, hunger, and health seem insurmountable is that we don’t yet have all the tools to solve them. But I’m optimistic that one day soon we will, thanks in part to innovators like researchers at IARI.
India as a whole gives me hope for the future. It’s about to become the world’s most populous country—which means you can’t solve most problems there without solving them at scale. And yet, India has proven it can tackle big challenges. The country eradicated polio, lowered HIV transmission, reduced poverty, cut infant mortality, and increased access to sanitation and financial services.
How did they do it? India has developed a world-leading approach to innovation that ensures solutions reach those who need them. When the rotavirus vaccine—which prevents the virus that causes many fatal cases of diarrhea—was too expensive to reach every child, India decided to make the vaccine themselves. They worked with experts and funders (including the Gates Foundation) to build factories and create large-scale delivery channels to distribute the vaccines. By 2021, 83 percent of 1-year-olds had been inoculated against rotavirus—and these low-cost vaccines are now being used in other countries around the world.
There is no question today’s challenges will test the limits of that ingenuity and cooperation. India is on the frontlines of climate change. But the progress it has made on health will make its people more resilient and provide helpful insights for how to tackle other major challenges. And the pace of its development, its skill in rolling out large-scale programs, and its people’s innovative expertise mean that India can be a key part of making progress on today’s biggest challenges.
I’m going to India next week to see firsthand the work being done by innovators and entrepreneurs. Some are working on breakthroughs that will help us mitigate the effects of climate change, like the work being done by Breakthrough Energy Fellow Vidyut Mohan and his team to turn waste into biofuels and fertilizers in remote agricultural communities. Others are finding new ways to help people adapt to a warmer world, such as IARI’s efforts to create more drought-tolerant crops. I’m looking forward to seeing the progress that’s already underway by both the Gates Foundation’s and Breakthrough Energy’s amazing partners.
Like every other country on the planet, India has limited resources. But it has shown us how the world can still make progress in spite of that constraint. By collaborating and trying novel approaches, the public, private, and philanthropic sectors can turn limited resources into big pools of funding and knowledge that lead to progress. If we work together, I believe we can fight climate change and improve global health at the same time.

Back in China
I’m visiting the country after four years away
I’m seeing first-hand some of the innovations that could contribute to global progress.

I want to share a few impressions from my time in China. I just had a meeting with President Xi, in which we discussed the importance of addressing global health and development challenges, like health inequity and climate change, and how China can play a role in achieving progress for people everywhere.
As part of my work with the Gates Foundation, I’ve tried to visit China, India, countries in Africa and Europe, and Washington D.C. each year. On these trips, I’d talk to researchers, government leaders, advocates, and other experts who are working on inequities in health and development. I’d always learn a lot, returning inspired by what I saw and heard.
It’s great to be able to resume these regular visits. This was my first trip to China in four years, and immediately after this trip, I’m headed to West Africa for the first time in five years. And I went to India in March.
On each trip this year, I have a key message: Over the past two decades, the world made significant strides in reducing poverty and improving health outcomes, but COVID was a big setback and even reversed progress on some global goals like reducing poverty and fighting TB and malaria. Many African countries, for example, are particularly impacted by overlapping challenges, including the effects of climate change, high food prices, escalating poverty rates, surging infectious diseases, and significant debt pressures.
Even though the challenges facing many African countries are complex, I’m optimistic that innovation in health, agriculture, digital finance, and energy will help improve lives there. I’m looking forward to meeting leaders and young people helping to accelerate progress when I visit West Africa.
Solving these problems requires innovation—both new tools and new ways of doing things. China has eliminated diseases, including polio and malaria, within its borders, developed drugs like artemisinin that have saved millions of lives around the world from malaria, made great strides in poverty reduction, and has made significant investments in clean energy and climate adaptation. So I was looking forward to seeing what’s changed since my last visit four years ago.
One highlight was my visit to the Global Health Drug Discovery Institute, an organization our foundation helped establish six years ago in partnership with the Beijing Municipal Government and Tsinghua University. GHDDI represents a productive way for public and private partners to work together on discovering new medicines for diseases that disproportionately impact the world’s most vulnerable populations but have applications for the world. I spoke about the institute’s work on TB and malaria yesterday, and we also extended our partnership over the next five years.
I also got to visit the National Crop Genebank of China. This facility is a prominent crop research center and also serves as a long-term preservation storage space for seeds so that scientists around the world have access to important genetic data. During my visit, I met with agricultural scientists who are working with their counterparts worldwide, particularly in Africa, on new rice varieties that help farmers increase their productivity and minimize the need for fertilizers, pesticides, and irrigation.
The benefits of their work have reached millions of farming households across Asia and Africa. The continued investment in technology and innovation within the agricultural sector has played a significant role in the increase in agricultural productivity throughout China. What excites me even more is China’s commitment to share their expertise and innovative practices with low-income countries. By assisting farmers in adapting to climate change, increasing their income, and combating food crises, they are making a substantial contribution to global food security.
The genebank and GHDDI are just two examples of the promising work the foundation has seen in China in the more than 15 years we’ve been partnering here. And there will be more opportunities for China and others to step up later this year, including a summit on development financing in Paris, a meeting of the G20 in New Delhi, and the COP28 climate conference in Dubai.
I’m convinced that if the world works together to address climate change, health inequity, and food security we can make extraordinary progress. And I’m looking forward to exploring new opportunities for collaboration and innovation that will make a better future for everyone.

Incredible innovation
A promising new vaccine candidate to protect children from their #1 killer
More than 670,000 children die from pneumonia every year. A new vaccine could save many lives.

The leading cause of death among children under age 5 often begins with little more than a cough.
Followed by chills, fever, and nausea.
And then as the child’s lungs get flooded with fluid, each breath becomes a desperate gasp for air.
What I’m describing is known as pneumonia, an acute respiratory condition that kills over 670,000 children every year.
And here’s a sentence I find difficult to write: Nearly all those deaths could have been prevented.
Access to vaccines, diagnostic tools, and treatments can protect children from deadly pneumonia. But these solutions are often not available or accessible in many low- and middle-income countries, where children are at greatest risk.
Even as child deaths have declined by nearly 50 percent over the past two decades, deaths from pneumonia have remained stubbornly high.
That’s why our foundation is focused on improving access to and development of vaccines that can prevent it.
One of the most exciting areas of progress is the development of a powerful new vaccine designed to protect children against pneumococcal bacteria, which is the leading cause of deadly pneumonia. Of the 670,000 children who die from pneumonia ever year, pneumococcal pneumonia is responsible for killing 400,000 of them.
What makes this new vaccine unique is that it is designed to protect against 25 different types of pneumococcal bacteria, more than any other available vaccine. Existing pneumococcal vaccines protect against about half as many types of pneumococcal pneumonia. To address the remaining deaths from pneumococcal pneumonia, vaccines that offer broader protection like this new vaccine will be needed.
The vaccine, called IVT-PCV25, is being developed by Inventprise, a small biotechnology company based outside Seattle. I recently took a tour of their new vaccine manufacturing plant and got an update on their progress.
It was amazing to see the innovations underway at Inventprise. Making a vaccine that is effectively 25 vaccines in one is an extremely complex challenge. Past efforts to add more strains of pneumococcal bacteria to vaccines using conventional technologies have resulted in vaccines that didn’t produce a strong enough immune response. Inventprise intends to overcome this obstacle with its proprietary vaccine technology that is designed to guard against many types of pneumococcal bacteria without any decline in protection.
Inventprise’s new factory, supported by a grant from our foundation, is a highly automated facility that marks an important step forward in Inventprise’s development of the vaccine. Clinical trials of the vaccine are expected to begin later this year.

Across the finish line
Makoy Samuel Yibi won’t stop until the world eradicates its next disease
Guinea worm once infected 3.5 million people every year. Thanks to heroes like Makoy, that number dropped to 13 last year.

When you see someone suffering from a terrible disease, it’s hard not to imagine a world where no one has to feel this way ever again. But the problem with eradication is that it’s really, really hard. The fewer cases remain, the more difficult it is to find them. That’s why, in all of human history, we’ve only eradicated two diseases: smallpox and the cattle disease rinderpest.
That might change soon.
The world is close to eradicating Guinea worm disease, a debilitating and painful condition that once devastated an estimated 3.5 million people in Africa and South Asia every year. Thanks to heroes like Makoy Samuel Yibi, that number dropped to 13 people in 2023.
As the national director of the South Sudan Ministry of Health’s Guinea Worm Eradication Program, Makoy helped reduce the number of cases in his country last year to just two. That’s a remarkable accomplishment by any standard, but it’s truly impressive when you consider the circumstances he and his team have faced: civil wars, the COVID-19 pandemic, the political changes brought by South Sudan’s decision to become an independent country in 2011, and the fact that the nation was once home to 90 percent of the world’s Guinea worm cases.
I recently caught up with Makoy at the COP climate conference in Dubai, where we both participated in an event focused on ending neglected tropical diseases, or NTDs, like Guinea worm. When you meet him in person, it’s hard to imagine a better person for the job. Makoy is passionate, brilliant, and laser-focused on making life better for the people of South Sudan. So I was surprised to learn that, as a young man, he never imagined a career in health.
Makoy was born in Terekeka County, a rural area located on the shores of the West Nile in southern Sudan. When he was a young man, Makoy had one primary focus: avoiding military service, which could be extremely dangerous. A chance meeting with a general from Terekeka resulted in a position with the national health department. A measles outbreak was ravaging parts of Sudan at the time, and Makoy’s first assignment was to travel from village to village providing care.
“What struck me,” he recalls, “was that, in every household we went to, we found at least half of the household was down with Guinea worm.”
The Guinea worm is a particularly nasty parasite. It’s unlikely to kill you, but the disease it causes—which is also called dracunculiasis, or “afflicted with little dragons”—can incapacitate you for months at a time and leave you permanently disabled. That can have devastating consequences if your family counts on you to grow the food you eat and sell it to make a living, as many people in South Sudan do.
The way the disease works is horrifying. If a person drinks water contaminated with Guinea worm larvae, the larvae enter the digestive system and mate. The impregnated female worm grows, undetected by the body’s immune system. Around a year later, the infected person will start to feel an itch somewhere on their body (usually the lower leg or foot). After a couple days, a painful blister appears and eventually bursts. The worm—which is now about one meter long—slowly starts to emerge from the wound.
This can take weeks or even months, and the pain it causes is excruciating. The wound can get infected, which could result in permanent disfigurement or even require amputation. And people often endure multiple worms emerging at the same time. Makoy has seen patients with as many as 40 worms.
And here’s the most insidious part: One of the few ways to relieve the pain of the blister is by soaking it in cold water, like a pond or a puddle. But that’s exactly what the worm wants. As soon as it touches water, it releases its larvae, starting the cycle anew. The Guinea worm is scarier and more efficient than any monster in a horror movie.
Makoy has seen countless times how devastating Guinea worm can be. “This is a situation where you see serious disruption of the livelihood of the community,” he says. “You see people going through a cycle of hunger because they don’t have enough. They have lost the window of cultivation. They’re not able to tend to their cattle, and there’s nothing they can do.”
There is no cure or treatment for Guinea worm, and yet, the world is on the doorstep of eradicating it. How? Through a series of highly effective interventions and a network of incredibly dedicated health workers.
Makoy’s team has built a network of volunteers in virtually every village in the country, who report rumors of Guinea worm cases. They spend every day searching for cases, getting the word out, and building trust in a country where more than 60 languages are spoken.
Makoy and his colleagues investigate every single rumor, no matter how remote. During the rainy season when the majority of cases happen, he often spends days hiking through the Sudd or up a mountain with all of his supplies on his back just to reach his destination. Last year, in a country the size of France with less than 100 miles of paved road, the team responded to nearly all of the 50,000 rumors they received within 24 hours.
Once the team finds a confirmed case, they make the patient as comfortable as possible and do what is called “controlled immersion.” This means soaking the affected area in a bucket of water and encouraging the worm to come out.
Makoy also spends a lot of time preventing people from getting Guinea worm in the first place. His team distributes free water filters and educates communities about safe water practices. The system they’ve built to support this work has strengthened health systems across the country, providing a platform for delivering other health services like childhood vaccination.
Makoy’s team has had a tremendous partner in all of this work: former U.S. President Jimmy Carter and the Carter Center. In 1995, when Makoy was first starting his public health journey, President Carter negotiated what remains the longest humanitarian ceasefire in history when he helped convince both sides of the Second Sudanese Civil War to lay down their arms and allow health workers access to treat Guinea worm and other diseases, like polio and river blindness. Today, the Carter Center continues to lead the global eradication campaign’s march to zero. The Gates Foundation is proud to support the Carter Center as part of our overall efforts to tackle NTDs. (You can learn more about Makoy’s partnership with the Carter Center in a new film called The President and the Dragon that is coming out later this year.)
Eradication is now within sight, although it won’t be easy to eliminate the last few cases. South Sudan previously reported no Guinea worm in 2018, but cases were subsequently discovered after a peace agreement was reached in the South Sudanese Civil War. And Guinea worm has recently been detected in dogs and other animals, mainly in Chad. Eradication will require stopping all transmission, both human and animal.
But Makoy Samuel Yibi is optimistic we can get there—and so am I. His determination to root out every last case makes me hopeful that we will someday soon celebrate the end of Guinea worm disease.
“In the places where Guinea worm has been eliminated,” he says, “you can actually see how communities have been energized. They are more active, and they are productive. The communities are now empowered to be more self-sufficient, because they don’t have to worry about Guinea worm.”
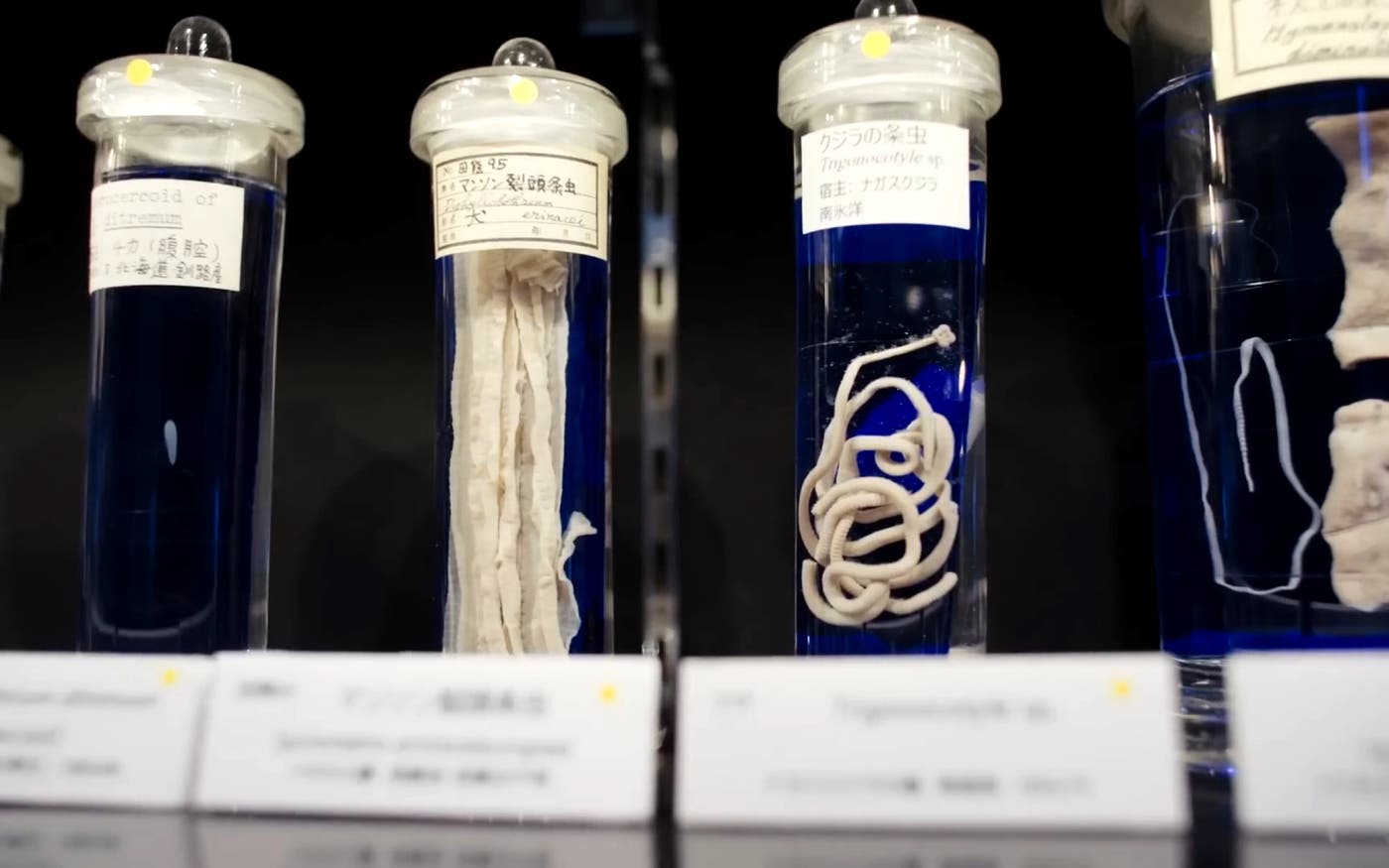
Ick!
What’s gross and better to see on an empty stomach? This museum in Tokyo
Welcome to the bizarre, creepy, and endlessly fascinating exhibits at the world’s foremost parasite museum.

You may want to skip lunch—and probably avoid sushi for dinner—when visiting the world’s foremost museum of parasites in Tokyo.
At the quirky and endlessly fascinating Meguro Parasitological Museum, which I toured during my trip to Japan in August, you’ll find hundreds of stomach-turning displays featuring creepy parasite specimens.
Some of the strangest-looking ones have resided inside the bodies of fish, turtles, pigs, and other animals. But by far the most horrific specimens are the parasites that have chosen humans as their hosts.
What steals the show is the world’s longest tapeworm. In 1986, this garden-hose length parasite was discovered living in the small intestine of a Japanese man. He had dined on a piece of raw salmon that was infected with a tapeworm egg smaller than a grain of rice. Over the next three months it grew and grew until it reached 29 feet long! (If you’re a follower on my Instagram account, you may have gotten a glimpse of this impressive specimen.)
The man who recovered the tapeworm from this unfortunate patient was Dr. Satoru Kamegai, the founder of Meguro Parasitological Museum. A physician, Dr. Kamegai started practicing medicine after World War II. At the time the country’s water and sanitation systems were in ruins and many people throughout Japan suffered from parasitic diseases. Dr. Kamegai became fascinated by the strange world of parasites and started collecting them from his patients. In 1953, he opened a small museum to display his findings and raise awareness of these creatures. Dr. Kamegai passed away in 2002, but the museum has continued to operate as a private research and educational facility.
Today, the museum has a collection of 60,000 different parasites, about 300 of which are on display in the two-story collection. Entrance to the museum is free and it draws a steady stream of visitors. It even has a gift shop with parasite-themed t-shirts, pens, and jewelry. (I picked up a t-shirt with the famous tapeworm on it.)
While I had a busy trip to Japan, I took time to stop at this museum because of our foundation’s efforts to reduce the burden of so-called neglected tropical diseases, many of them caused by parasites. More than 1 billion people suffer from these overlooked diseases with often difficult to pronounce names, including dracunculiasis (Guinea worm disease), human African trypanosomiasis (sleeping sickness), visceral leishmaniasis (black fever), onchocerciasis (river blindness), and schistosomiasis (snail fever).
These diseases can cause anemia and blindness, stunt children’s growth, lead to cognitive impairments, complicate pregnancies, and result in thousands of deaths each year. And it’s not uncommon for people living in extreme poverty to suffer from more than one of these diseases at the same time, affecting their ability to go to school or make a living.
Our foundation works with partners on the treatment and control of these diseases. One of the most successful efforts has been mass drug administration, which seeks to treat everyone against a disease—even if they are not actually infected or show any symptoms. I observed this incredible work in Tanzania, where I joined a group of health workers going from house to house to distribute medicine to wipe out lymphatic filariasis, one of the world’s most painful and debilitating diseases.
The good news is that there’s been a lot of progress in reducing parasitic diseases around the world. But there’s still more work to be done. That makes this museum a great place for people to learn about where these diseases still exist and the incredible work that’s going on to wipe them out.
If you happen to be in Tokyo, I encourage you to visit.
Neglected no more
A massive success
How to stop disease by treating everyone—even healthy people.

Health workers have an unusual tool for fighting disease that turns our old thinking about treatment on its head. I saw it at work recently in a remote hilltop village in Tanzania, where I joined a group of health workers going from house to house to distribute medicine to wipe out lymphatic filariasis, one of the world’s most painful and debilitating diseases.
At each home, one health worker told the family about the swollen limbs, disfigurements, and other symptoms of the parasitic disease. Another carried a tall stick to measure the height of each family member to determine the correct dosage. Then, if they were willing to be treated, the parents and children took their pills and washed them down with a cup of water before our team moved on to the next house.
What was surprising about this effort is that none of the people who took the medicine were sick.
The village I visited was participating in what’s known as a mass drug administration campaign, which seeks to treat everyone against a disease—even if they are not actually infected or show any symptoms. Typically, of course, the sick are the ones who get treated, not the people who are healthy. But when it comes to combating some diseases, like lymphatic filariasis, it’s critical for health workers to try to treat the entire at-risk population to break the cycle of transmission. If not, the disease could continue to be spread by those who are not aware they are infected.
Ten countries have successfully eliminated lymphatic filariasis in this way, including Togo, which this year became the first country in sub-Saharan Africa to wipe out the disease. Still, more than 800 million people in 52 countries worldwide remain threatened by lymphatic filariasis.
Mass drug administration is not only effective against lymphatic filariasis, but also other neglected tropical diseases, including schistosomiasis, onchocerciasis, trachoma, and soil-transmitted helminths. These diseases go by names that are largely unknown and often difficult to pronounce. But it should be easy to understand why we should all care about them. They afflict people living in the poorest countries and cause untold suffering.
Lymphatic filariasis is one of the worst of these diseases. It’s caused by a parasite that’s spread by mosquitoes, and in the severest cases people may develop swollen limbs, a thickening of the skin known as elephantiasis, or other severe disfigurements. Beyond the pain and disabilities they experience, people affected by the disease are often ostracized by their communities and are unable to work, sinking them deeper into poverty.
To combat lymphatic filariasis, health officials could test everyone and then treat only those people who are infected. But testing the population for these diseases would be expensive and slow. The medicines used for treatment (ivermectin and albendazole), however, are inexpensive and have no side effects, making mass treatment a more effective approach to protect people from the disease. (And thanks to the generosity of the many pharmaceutical companies, billions of doses of these and other medicines combating neglected tropical diseases are being donated for free.)
Like many countries running mass drug administration programs, Tanzania’s biggest challenge is treating enough of its population at risk of the disease. To break the cycle of transmission, health workers must treat at least 65 percent of the population every year for 5 to 10 years. As you might imagine, meeting this target year after year is not easy.
Health officials must have strong public awareness campaigns, thousands of trained health workers, a well-organized supply chain to distribute medicines to the remotest corners of the country, and regular disease surveying to track their progress. At the same time, the program provides treatment and care for people who are suffering from the debilitating symptoms of the diseases.
Walking from door to door in the village with the health workers, I was struck that perhaps the most important element of the program is trust. Taking the medicine is strictly voluntary, making it important that the health workers distributing it earn the confidence of the community. The health workers I met certainly had. They were knowledgeable, passionate about their work, and clearly cared about the community they were serving. At each home, they took the time to explain the goal of the program and address any of the villagers’ questions or concerns. Thanks to their hard work the latest survey of lymphatic filariasis in their district showed that the cycle of transmission had been broken. For the first time, the village was not at risk of the disease.
By 2020, Tanzania hopes to eliminate lymphatic filariasis entirely within its borders. Based on what I saw in this village, I’m optimistic they will.
24:00:00
Record-breaking generosity
On January 30, 2017, a group combatting neglected diseases did something extraordinary. Guinness World Records took notice.

Page through the Guinness Book of World Records and you’ll learn that a lot can happen in 24 hours.
On February 14, 2004, Dan Meyer of Davis, California, set the record for the longest paperclip chain by an individual in 24 hours. Length: 5,340 feet. Total number of paper clips: 54,030.
On June 4, 2011, Nabi Salehi, a barber in London, set the record for giving the most consecutive haircuts in 24 hours. Total haircuts: 526.
And on January 30, 2017, another achievement—one that will improve millions of lives—was added to the Guinness World Record list. A group fighting neglected tropical diseases—including Guinea worm, river blindness, and elephantiasis—set the record for most drugs donated in a 24-hour period. Total number of drugs: 207,169,292!
This week in Geneva, I was excited to participate in the ceremony to celebrate the group that achieved this incredible feat, Uniting to Combat Neglected Tropical Diseases, a coalition of drug companies, governments, health organizations, charities, and other partners who work to reduce the burden of tropical diseases that impact the world’s poorest.
On January 30th, they organized drug manufacturers, warehouse workers, delivery drivers, government officials, and health workers to deliver this historic number of donated drugs on four continents for distribution to people living in the remotest parts of the world.
What’s truly amazing is that the 207 million drugs donated on January 30th represent just a small amount of this group’s generosity. Since 2012, when United to Combat Neglected Tropical Diseases signed a declaration to control or eliminate 10 of the worst neglected diseases, they have donated 7 billion treatments. I’m grateful to the pharmaceutical companies that have been making these donations year after year: Bayer, Eisai, Gilead, GSK, Johnson & Johnson, MSD, Merck KGaA, Novartis, Pfizer, and Sanofi.
Thanks to the efforts of these drug companies and their partners millions of people are receiving the medicines they need to cure and protect them from these diseases. These diseases are in retreat and the world is moving closer to the day when they will be eliminated altogether.
Of course, all world records get challenged. And I for one will be thrilled for the day when this record for drug donations gets broken. So will the millions of families around the world who need them.
Warning!
Neglected no more
These diseases may be difficult to pronounce, but it should be easy to see why everyone should care about them.

Warning: you may find what I’m about to write disturbing.
Imagine a fly infected with parasites bites you. First you get a fever, then headaches, joint pains, and itching. Eventually, when the parasites cross the blood-brain barrier, you lose your mind, you can’t control your muscles, and then you lose your life.
Now, imagine you drink a glass of water. The water contains tiny fleas containing even tinier larvae. The larvae mate and grow in your body. One year later, a painful blister forms on your foot. The head of a worm pokes out. It’s 3-feet-long and takes weeks to remove.
Finally, imagine a mosquito bites you. It’s infected with tiny larvae. They set up camp in one of your lymph nodes, where they mate and nest, causing your leg to eventually swell to 10 times its size.
Sound horrific? Well, I haven’t told you the most disturbing part. I’m not making up these diseases (Human African trypanosomiasis, Dracunculiasis, and Lymphatic filariasis). They are just three of more than a dozen tropical diseases that afflict some of the poorest people in the world. As I write this, more than a billion people suffer from at least one of them.
These diseases go by names that are largely unknown and often difficult to pronounce.
Still, it should be easy to understand why we should all care about them. Spread by worms and insects, they disfigure and disable people living in the remotest areas of the world, keeping children out of school and parents from being able to work. In the worst cases, they kill. And all of them can be prevented—if the world continues to work together to end them.
I am in Geneva, Switzerland this week for a meeting to raise awareness and continue support for the fight against these overlooked diseases. Collectively, they’ve been dubbed “Neglected Tropical Diseases,” but lately they’ve been getting some of the attention they deserve.
Five years ago, Uniting to Combat Neglected Tropical Diseases, a group of pharmaceutical companies, governments, health organizations, charities, and other partners, came together to treat and prevent these diseases. They set a goal to control or eliminate at least 10 of them by 2020. Today, there’s a lot of progress to celebrate. Fewer people are suffering from them, and many countries are on their way to eliminating them altogether.
Here are some examples of the progress that’s been made.
Dracunculiasis (also known as Guinea worm), the parasitic disease I described above in which a large worm grows inside its victims, is nearing its end. In 1985, the disease afflicted an estimated 3.5 million people in 21 countries in Africa and Asia. Last year, thanks to the work of Uniting to Combat NTDs, The Carter Center, and other partners the number of Guinea worm cases has been reduced by more than 99 percent to 25 cases.
Lymphatic filariasis, also known as elephantiasis, is thepainful, disfiguring disease spread by mosquitoes. Five years ago, 1.5 billion people needed preventive drug treatment to protect them from the disease. Since then, it has been eliminated in six countries and reduced in 18 others.
Human African trypanosomiasis (HAT), commonly known as sleeping sickness, is also in retreat. Cases have declined by more than 90 percent, from 26,000 cases in 2000 to 2,733 in 2015.
What’s driving this progress? It’s been the result of drug donations by pharmaceutical companies and generous commitments by donors and governments. More than one billion people were reached with NTD treatments in 2015 alone—across nearly 150 countries.
New innovations for testing and treatment have also made a big difference. For example, the diagnostic test for sleeping sickness used to require electricity, bulky equipment, and refrigeration, making it difficult to deliver to remotest areas of the world. Now, a simple finger-prick blood test allows health workers to test for the diseases. And new smartphone-based mapping tools could make it easier to map these diseases so health workers can target their treatment efforts in real time down to the household level.
Still, there’s a lot of work to be done. We need continued support from donor governments to finish the job. We need more research on improved drugs and tests to help make it easier to treat people quickly. And we must support the frontline health workers who have the tough job of delivering the drugs in the hardest to reach regions of the world.
If the world keeps up the fight against these diseases, we can improve the lives of millions of the poorest families. They won’t be neglected anymore.
Take Action
Help us eliminate these debilitating diseases that afflict the world’s poorest by supporting The END Fund. The END Fund is a GiveWell Top Charity.

Wrapping up 2018
What I learned at work this year
Thoughts on Alzheimer’s, climate change, polio, and more.

Every Christmas when I was a kid, my parents would send out a card with an update on what the family was up to. Dad’s law firm is growing, Mom’s volunteer work is going strong, the girls are doing well in school, Bill is a handful.
Some people think it is corny, but I like the tradition. These days, at the end of each year, I still enjoy taking stock of my work and personal life. What was I excited about? What could I have done better?
I thought I would share a few of these thoughts as 2018 concludes.
One thing that occurs to me is that the questions I am asking myself at age 63 are very different from the ones I would have asked when I was in my 20s.
Back then, an end-of-year assessment would amount to just one question: Is Microsoft software making the personal-computing dream come true?
Today of course I still assess the quality of my work. But I also ask myself a whole other set of questions about my life. Did I devote enough time to my family? Did I learn enough new things? Did I develop new friendships and deepen old ones? These would have been laughable to me when I was 25, but as I get older, they are much more meaningful.
Melinda has helped broaden my thinking on this point. So has Warren Buffett, who says his measure of success is, “Do the people you care about love you back?” I think that is about as good a metric as you will find.
It may sound grand, but I think the world is slowly going through a similar transition to a broader understanding of well-being. For most of human history, we have been focused on living longer by fighting disease and trying to grow enough food for everyone. As a result, life spans have gone up dramatically. Technology has played a key role in that through vaccines, medicines, and improved sanitation.
We still need a lot of innovation to solve problems like malaria or obesity, but we are also going to be focusing more on improving the quality of life. I think this will be the thrust of many big breakthroughs of the future. For example, software will be able to notice when you’re feeling down, connect you with your friends, give you personalized tips for sleeping and eating better, and help you use your time more efficiently.
There are not the same clear measures of these things as there are for diseases, and there may never be. But there is nascent work in this field and I think it is going to accelerate.
As I look back on the year, I am also thinking about the specific areas I work on. Some of this is done through our foundation but a lot of it (such as my work on energy and Alzheimer’s work) is not. What connects it all is my belief that innovation can save lives and improve everyone’s well-being. A lot of people underestimate just how much innovation will make life better.
Here are a few updates on what’s going well and what isn’t with innovation in some areas where I work.
Alzheimer’s disease
I saw two positive trends in Alzheimer’s research in 2018.
One is that researchers focused on a new set of ideas about how to stop Alzheimer’s.
The first generation of theories, which dominated the field for years, emphasized two proteins called amyloid and tau. These proteins cause plaques and tangles in the brain, clogging up and killing brain cells. The idea was to stop the plaques and tangles from forming. I hope these approaches pay off, but we have not seen much evidence that they will.
In the past year, researchers have doubled down on a second generation of hypotheses. One theory is that a patient’s brain cells break down because their energy producers (called mitochondria) wear out. Another is that brain cells break down because part of the immune system gets overactivated and attacks them.
This is a great example of how improving our understanding of biology will reduce both medical costs and human suffering.
The other trend this year is that the Alzheimer’s community focused on getting more and better access to data. We’re working with researchers to make it easier for them to share information from their studies broadly so that we can better understand questions like how the disease progresses.
Over the past few years, the U.S. government has dramatically stepped up funding for Alzheimer’s research, from $400 million a year to over $2 billion a year. There is also a big push to create better diagnostics.
The only problem where I don’t yet see a clear path forward yet is how to develop more efficient ways to recruit patients for clinical trials. Without a simple and reliable diagnostic for Alzheimer’s, it’s hard to find eligible people early enough in the disease’s progression who can participate in trials. It can take years to enroll enough patients. If we could find a way to pre-screen participants, we could start new trials more quickly.
But there is so much momentum in other areas—scientific tools, better diagnostics, improved access to data—that as long as we can solve the recruitment problem, I am confident that we will make substantial progress in the next decade or two.
Polio
I thought we would be closer to eradicating polio today than we are. Unfortunately, there were more cases in 2018 than in 2017 (29 versus 22).
I underestimated how hard it would be to vaccinate children in places where there’s political violence and war. Families move around to escape fighting, which makes it hard to keep track of children and make sure they get all the doses of the vaccine. Or sewage systems get destroyed, allowing the virus to spread as children come into contact with an infected person’s excrement.
This is a key reason why Afghanistan and Pakistan have never been free of polio—in fact they are the only two countries that have never been free of polio.
I spend a lot of time on polio, part of it talking to the funders to make sure they continue their commitment even though eradication is taking longer than any of us would like. I remind them of the huge benefits of success, and the risk that the disease will return in a big way if we don’t finish the job.
I also remind them what a difference innovation is making. We’re now able to test sewage samples to track the virus and find the source before an outbreak starts. And the global health community is finding creative ways to work in war zones, having stopped outbreaks in Syria and Somalia in recent years.
Finally, I am hopeful about a new oral vaccine being tested in Belgium and Panama. The results should be out in 2019, and if this one proves effective, it would overcome some of the problems with previous oral vaccines when they’re used in places where few children are immunized. The new vaccine could be in use as soon as 2020.
Despite all the challenges, I am still optimistic that we can eradicate polio soon.
Energy
Global emissions of greenhouse gases went up in 2018. For me, that just reinforces the fact that the only way to prevent the worst climate-change scenarios is to get some breakthroughs in clean energy.
Some people think we have all the tools we need, and that driving down the cost of renewables like solar and wind solves the problem. I am glad to see solar and wind getting cheaper and we should be deploying them wherever it makes sense.
But solar and wind are intermittent sources of energy, and we are unlikely to have super-cheap batteries anytime soon that would allow us to store sufficient energy for when the sun isn’t shining or the wind isn’t blowing. Besides, electricity accounts for only 25% of all emissions. We need to solve the other 75% too.
This year Breakthrough Energy Ventures, the clean-energy investment fund I’m involved with, announced the first companies we’re putting money into. You can see the list at http://www.b-t.energy/ventures/our-investment-portfolio/. We are looking at all the major drivers of climate change. The companies we chose are run by brilliant people and show a lot of promise for taking innovative clean-energy ideas out of the lab and getting them to market.
Next year I will speak out more about how the U.S. needs to regain its leading role in nuclear power research. (This is unrelated to my work with the foundation.)
Nuclear is ideal for dealing with climate change, because it is the only carbon-free, scalable energy source that’s available 24 hours a day. The problems with today’s reactors, such as the risk of accidents, can be solved through innovation.
The United States is uniquely suited to create these advances with its world-class scientists, entrepreneurs, and investment capital.
Unfortunately, America is no longer the global leader on nuclear energy that it was 50 years ago. To regain this position, it will need to commit new funding, update regulations, and show investors that it’s serious.
There are several promising ideas in advanced nuclear that should be explored if we get over these obstacles. TerraPower, the company I started 10 years ago, uses an approach called a traveling wave reactor that is safe, prevents proliferation, and produces very little waste. We had hoped to build a pilot project in China, but recent policy changes here in the U.S. have made that unlikely. We may be able to build it in the United States if the funding and regulatory changes that I mentioned earlier happen.
The world needs to be working on lots of solutions to stop climate change. Advanced nuclear is one, and I hope to persuade U.S. leaders to get into the game.
The next epidemic
In 1918, the Spanish flu killed 50 million people worldwide. It still ranks as one of the deadliest natural disasters ever.
I had hoped that hitting the 100th anniversary of this epidemic would spark a lot of discussion about whether we’re ready for the next global epidemic. Unfortunately, it didn’t, and we still are not ready.
People rightly worry about dangers like terrorism and climate change (and, more remotely, an asteroid hitting the Earth). But if anything is going to kill tens of millions of people in a short time, it will probably be a global epidemic. And the disease would most likely be a form of the flu, because the flu virus spreads easily through the air. Today a flu as contagious and lethal as the 1918 one would kill nearly 33 million people in just six months.
I have been studying this for several years. To be prepared, we need a plan for national governments to work together. We need to think through how to handle quarantines, make sure supply chains will reach affected areas, decide how to involve the military, and so on. There was not much progress on these questions in 2018.
The good news is that there has been progress toward a vaccine that would protect you from every strain of the flu. This year I visited the U.S. National Institutes of Health in Maryland and got an update from some of the people leading this work.
The challenges of making a universal flu vaccine are fascinating. All strains of the virus have certain structures in common. If you’ve never been exposed to the flu, it’s possible to make a vaccine that teaches your immune system to look for those structures and attack them. But once you’ve had the flu, your body obsesses over the strain that got you sick. That makes it really hard to get your immune system to look for the common structures.
So it is clear how we could make a universal vaccine that would protect anyone (such as the very young) who has never been exposed to the flu before. But for anyone who has already had the virus, it is a lot harder. The problem is a long way from being solved, but new research money is coming in and more scientists are working on it.
To make the most of these scientific efforts (some of which our foundation is funding), the world needs to develop a global system for monitoring and responding to epidemics. That is a political matter that requires international cooperation among government leaders. This issue deserves a lot more focus.
Gene editing
Gene editing made the news in November when a Chinese scientist announced that he had altered the genes of two baby girls when they were embryos. What is unprecedented about his work is that he edited their germline cells, meaning the changes will be passed down to their children. (The other, less controversial type of gene editing involves somatic cells, which aren’t inherited by future generations.)
I agree with those who say this scientist went too far. But something good can come from his work if it encourages more people to learn and talk about gene editing. This might be the most important public debate we haven’t been having widely enough.
The ethical questions are enormous. Gene editing is generating a ton of optimism for treating and curing diseases, including some that our foundation works on (though we fund work on altering crops and insects, not humans). But the technology could make inequity worse, especially if it is available only for wealthy people.
I am surprised that these issues haven’t generated more attention from the general public. Today, artificial intelligence is the subject of vigorous debate. Gene editing deserves at least as much of the spotlight as AI.
I encourage you to read up on it whenever you have a chance. Keep an eye out for articles in your news feed. If you are willing to read a whole book, The Gene by Siddhartha Mukherjee is very well done. This story is one to follow, because big breakthroughs—some good, some worrisome—are coming.
Looking ahead
I am making a resolution for 2019.
Although I have never been one for New Year’s resolutions, I have always been committed to setting clear goals and making plans to achieve them. As I get older, these two things look more and more like the same exercise. So I am making a resolution for 2019. I am committing to learn and think about two key areas where technology has the potential to make an enormous impact on the quality of our lives, but also raises complex ethical and social considerations.
One is the balance between privacy and innovation. How can we use data to gain insights into education (like which schools do the best job of teaching low-income students) or health (like which doctors provide the best care for a reasonable price) while protecting people’s privacy?
The other is the use of technology in education. How much can software improve students’ learning? For years we have been hearing overheated claims about the huge impact that technology would have on education. People have been right to be skeptical. But I think things are finally coming together in a way that will deliver on the promises.
I will be posting updates on these and other issues on the Gates Notes.
In the meantime, Melinda and I are working on our next Annual Letter. The theme is a surprise, though it is safe to say we’ll be sharing some positive trends that make us optimistic about the future. We’ll send the letter out in February.
I hope you have a happy and healthy start to 2019.
A true data farm
Can the Wi-Fi chip in your phone help feed the world?
I recently visited an amazing farm near Seattle that uses data to grow better harvests.

I recently visited a remarkable farm in Carnation, Washington, just 25 miles from downtown Seattle.
At first glance, Dancing Crow Farm looks like any other farm. There are rows of crops and, at least when I was there, the field was dusty. There were farm implements and freshly picked peppers piled up under a lean-to. But if you talk to Sean Stratman—the man responsible for this plot—it quickly becomes clear what makes his farm so special: Sean knows more about his land than almost any other farmer on earth.
Dancing Crow Farm is the pilot site for FarmBeats, an amazing new project that hopes to make farmers more productive by arming them with data. When most people think of groundbreaking digital technology, they don’t picture soil sensors. But a farmer who knows the temperature, pH, and moisture level of his soil can make all sorts of informed decisions that save money and boost yield.
For example, fertilizer works better when it’s applied to moist soil. But how do you know when to fertilize? Soil that feels dry is often still damp below the surface. You’ll end up fertilizing more often than necessary if you go by touch alone. But if you know exactly how much moisture is in your soil at any given moment, you can fertilize only when you need to. You use less and save money.
The problem is that most existing digital platforms that provide this kind of information are expensive. Sensors can cost hundreds of dollars each, and each one only covers 10 meters. The cost is so prohibitive that only the very richest farmers can afford them.
A team of researchers at Microsoft—led by researcher Ranveer Chandra, who I talk to in the video above—wants to change that. In FarmBeats, they’ve developed a series of innovations that might one day put data in the hands of even the poorest farmers.
The main innovation is in how FarmBeats sensors transmit data. Most farms have poor or no access to the Internet. In the United States, 20 percent of people living in rural areas don’t have access to even the slowest broadband speeds. Most farm data systems require expensive transmitters to connect, but FarmBeats relies on a clever workaround: it uses TV white space.
White spaces are unused TV broadcast spectrum. If you’ve ever watched an old TV, you’ve seen white spaces before. They’re the “snow” you’ll sometimes see while flipping through channels. These gaps in spectrum are plentiful in the remote areas where most farms are located, so data can be sent over them the same way that data gets transmitted via broadband.
Here’s how FarmBeats works: The whole system is powered by solar panels. You place a small number of sensors—one every couple hundred meters, instead of 10 meters—in the ground. You then attach your smart phone with the camera facing down to either a drone (if you have money to spare) or a helium balloon (if you don’t).

You walk around the fields with the camera, creating an aerial map of the farm. Data from both the sensors and the phone are transmitted via TV white space to your computer, where an edge device stitches everything together into a data map.
The data generated by FarmBeats has been a game changer for Sean and Dancing Crow Farm. He can use up to 30 percent less water for irrigation and 44 percent less lime to control soil pH. Information on soil temperature and moisture levels has helped him better time the planting of seeds, so he gets a more productive harvest. Because Dancing Crow Farm is located next to a river, flooding is a problem. FarmBeats’ aerial imaging capabilities precisely document flooding patterns, so he’s able to better plan what he plants where. The system even helped Sean identify parts of the farms where inadequate drainage was affecting the quality of beans.
It’ll be at least a year before every component of FarmBeats is available to the public—and even longer before the cost comes down enough for broad adoption (the current version is much cheaper than other farm data systems but still too expensive for poor farmers to afford). But I’m hopeful that one day this technology could be available to every farmer everywhere, including the most remote parts of Africa.
Even as they continue working on the current version, the FarmBeats team is already working on the next generation of their technology. They just released a paper demonstrating for the first time that Wi-Fi signals can be used to collect soil data. Using only their smart phones and super cheap RFID tags buried in the ground, any farmer could get important information about their land—no special, high tech equipment required.
The Wi-Fi technology is still theoretical, but I’m glad brilliant minds are thinking about how we can help the poorest farmers gather data and increase yield. Even small gains in productivity could mean the difference between affording to send your kids to school or not. And for farmers who rely on the food they grow to feed their family—where the size of your harvest is a matter of life or death—FarmBeats could be a literal lifesaver.
More than three-quarters of the world’s poor rely on agriculture to earn a living. If we’re going to win the fight against poverty, we must help farmers—and I believe that FarmBeats could be a powerful tool.
Just the facts, Max
Memorizing these three statistics will help you understand the world
Why we should be optimistic but not complacent.

One of my favorite websites is OurWorldInData.org. Based at the University of Oxford, it uses statistics—on everything from health and population growth to war, the environment, and energy—to give you phenomenal insight into how living conditions are changing around the world. I asked its founder, Oxford economist Max Roser, to share three facts from the site that everyone should know. Here’s what Max had to say. – Bill Gates
In the past few years, it has become easy to find many of the important statistics on global development with a quick online search. And since it is now so easy to find the information you need, many argue that it doesn’t make sense to actually remember these statistics. ‘Just look them up when you need them!’ they say.
I disagree with this. Yes, for some details, it makes sense to just search for them when you need them. But for the large global developments, it is important to know some basic statistics that describe living conditions currently and the direction of change that we have seen over the past few decades. Knowing the facts on global changes gives you the context for the daily news and allows you to make sense of new information that you learn. And it must be the basis for political debate, so that we can discuss what we should and shouldn’t do as a society.
And so I compiled a short list of three facts about global living conditions that I want to remember. Each of them describes the current situation and the direction of change.
Fact #1: Since 1960, child deaths have plummeted from 20 million a year to 6 million a year.
Imagine how awful it must be to see your child die.
Then consider that every minute this happens to about 11 parents. This is the number of children, younger than five years of age, who die—on average—every single minute. Eleven deaths every minute for 24 hours add up to 15,500 deaths per day, or 5.6 million deaths per year.
Do we just have to accept that? Is that just how the world is?
Clearly no. We are very much able to drive positive change. Look at the chart below. The same UN data that shows us that 5.6 million are dying today also shows us that in the 1950s and 60s the world saw around 20 million children dying every year.
One key reason why we struggle to see progress in the world today is that we do not know how very bad the past was.
Both are true at the same time: The world is much better than in the past and it is still awful.
To bring this to mind I need to know both statistics: When someone says we can sit back and relax because the world is in a much better place, I point out that 11 children are still dying every minute. We cannot accept the world as it is today. And when I feel hopeless in the face of this tragedy, I remember that we reduced annual child deaths from 20 million to 5.6 million in the last fifty years.
So I am remembering the current extent of child mortality and the direction of change that we have seen: The number of child deaths is falling; there were 3.5-times as many child deaths 50 years ago. But child deaths are still extremely common; 11 children are dying every minute.
Fact #2: Since 1960, the fertility rate has fallen by half.
The chart below shows the key statistic to understand about world population growth: the global fertility rate—the average number of children per woman in the world. When the fertility rate is close to 2 children per woman, so that every couple is on average replaced by about two children, population growth is slow. But until the late 1960s, each woman had on average more than 5 children, and at such high fertility rates, population growth is fast. At that time the world population increased by 2 percent every year.
The availability of contraceptives allows parents to have only as many children as they want. And that number changes as people’s income goes up. From decades of demographic research, we know that women decide to have fewer children as they get access to better education and better opportunities in the job market. We also know that when child mortality falls, so that families do not need to fear that their children will die, they consequently decide to have fewer children in the first place.
Improvements in conditions for women and the health of children have driven a rapid reduction in fertility rates across the world. In fact, the global fertility rate has halved in the last 50 years, from more than 5 children per woman to fewer than 2.5 children. The world population growth rate has also halved in the last 50 years and is just above 1 percent.
The statistic that I remember on population growth is the one that tells me that rapid population growth is coming to an end in this century. In the last 50 years the global fertility rate has fallen from 5 children per woman to less than 2.5 children per woman. In fifty years the fertility rate has halved.
Fact #3: 137,000 people escaped extreme poverty every day between 1990 and 2015.
Living in poverty means that many of the most essential things in life are out of reach. People in poverty tend to lack decent shelter and basic healthcare, and they often struggle to afford adequate food supplies.
People are considered to live in ‘extreme poverty’ if they have to get by on less than 1.90 international-dollars per day, which is a currency that corrects for price differences between countries and inflation.
In this definition of poverty, the term extreme poverty is clearly appropriate: this is a very low poverty line.
When you ask people whether the world is making progress against extreme poverty, the majority of us believe things are getting worse—that the number of people in extreme poverty in the world is rising.
The opposite is true. Both the number and the share of people in extreme poverty is falling:
In 1990, 1.86 billion people were living on less than 1.90 international-$ per day—more than every third person in the world. Twenty-five years later, the number of people living in extreme poverty has more than halved to 706 million, every tenth person.
This is a very large transformation. It means that, on average, every day for the past 25 years 137,000 fewer people were living in extreme poverty than the day before. On every day in the last 25 years there could have been a newspaper headline reading, “The number of people in extreme poverty fell by 137,000 since yesterday.”
This is the statistic I remember: Today every 10th person is living in extreme poverty—706 million people. An unacceptably large number of people. But we should also know that the trend is moving in the right direction. The number of people in extreme poverty is falling. It is possible to end extreme poverty.
Remembering these facts about the world brings to mind why I think it is important to get engaged in global development. The statistics on the current state of the world make clear that we cannot be complacent about the world as it is today. Especially because progress is uneven, and in sub-Saharan Africa progress has been slower, but is not absent. The statistics on global change over time tell us that it is possible to work for a better world. The number of child deaths is dropping. The challenges of rapid population growth will not continue indefinitely. And the number of people in extreme poverty is falling.
Let’s continue in this direction. Our past successes should encourage us to work for more progress.
Lifesavers
What kangaroos can teach us about saving lives
A simple, low-cost intervention can have a huge impact on newborn health.

I write a lot about new inventions that are improving people’s health and saving lives around the world. But some breakthrough ideas don’t involve any new technology at all. Let me tell you about one of my favorite examples—a solution that is readily available, requires no special equipment, and is so cheap any government can support it.
It’s called kangaroo mother care—continuous skin-to-skin contact between mothers and low-birth weight or premature babies. Combined with exclusive breastfeeding, this practice prevents neonatal deaths by regulating the baby’s temperature, accelerating weight gain, and reducing the risk of infections. What’s more, it encourages mother-infant bonding at a critical time of the child’s development.
Two Colombian pediatricians, Edgar Rey and Hector Martinez, developed kangaroo mother care in the 1970s. The doctors were struggling to care for preterm infants in Bogota, where few incubators were available. Looking for a solution, they drew inspiration from how kangaroos care for their young. Baby kangaroos, born the size of a lima bean, develop inside the pouch on their mother’s belly where they can feed and stay warm.
Years later, study after study has proven the benefits of skin-to-skin contact between mothers and their newborns. For preterm babies, it’s even better than warming them in an incubator. And even as new lifesaving technologies are introduced to facilities to support newborns, kangaroo mother care is an opportunity to keep mothers at the center of their baby’s care.
When kangaroo care has been adopted on a national scale, the impact is truly remarkable. Rwanda, for example, cut its newborn mortality rate by 30 percent between 2008 and 2015, largely due to the spread of kangaroo mother care along with encouraging exclusive breastfeeding and cutting the umbilical cord in a hygienic way.
Surprisingly, despite its clear benefits, kangaroo mother care is not practiced widely. But it should be. Every year, about 2.7 million newborns die during their first month of life. The majority of newborn deaths occur in parts of the world where there are no hospitals or clinics nearby, and no access to skilled birth attendants.
Many of these lives could be saved with simple, affordable health interventions like kangaroo mother care. Our foundation, along with many other organizations, have been working to spread the word about kangaroo mother care with policymakers and health officials so more parents can be trained to use this lifesaving practice.
If you need another reason to be convinced of the power of kangaroo mother care: A recent study found that this practice is a gift that keeps on giving. Kangaroo mother care had “significant, long-lasting social and behavioral protective effects” on children as they entered young adulthood. Parents who practiced kangaroo mother care were more protective and nurturing, and their children were less likely to miss school and less likely to be aggressive or hyperactive. These positive effects were still present in the children 20 years later! Now that’s a smart investment in our children’s future.
Business boost
Giving foreign aid helps America’s economy
Investing in the health of the world’s poor is good for U.S. companies

I’m a big fan of America’s investments in the health and well-being of the world’s poor. Unfortunately, not everyone feels the same way. In fact, some in Washington D.C. have proposed dramatic cuts in foreign assistance.
That would be a terrible mistake. Last month I wrote about how foreign aid helps keep Americans safe. In this post, I want to show how smart health and development programs promote America’s economy, and how cutting back on these investments could backfire on American workers.
(As I said in my previous post, these security and economic arguments aren’t what inspired Melinda and me to get involved in global health. What inspired us was the chance to save children from dying of preventable diseases. But over the years I’ve come to see the connection to America’s security and economy as well.)
I start from the simple premise that everyone is better off when there are more middle-income countries in the world. As a country climbs up the economic ladder, you see concrete improvements in the lives of its people. Richer countries are less likely to go to war and more capable of preventing global epidemics. And they can afford to buy more products from other countries, including the United States.
Here’s one example from my experience with Microsoft. From our earliest days, we intended to expand into markets beyond the United States. In 1986, we chose Tokyo for the site of our first foreign office. That bet paid off phenomenally well. For a time, we sold more software in Japan than anywhere else.
You may be thinking, “Of course an ambitious software company would want a foothold in Japan.” But it wasn’t always so obvious. Just a few decades before we opened our Tokyo office, Japan had been devastated by World War II. Its economy and infrastructure lay in ruins. How did they recover? Among other things, through smart aid programs from the United States and others. By the 1980s Japan’s economy was booming, and the country presented a great opportunity for companies like us. To this day, sales there are a key part of Microsoft’s success and these sales have produced many jobs in Japan and America alike.
Microsoft’s experience in Japan is part of a larger trend that’s still going on today, as more countries join the ranks of the middle class. Countless U.S. companies are doing business in places that used to get American aid but have become self-sufficient, including South Korea, Brazil, Mexico, Vietnam, and Thailand.
Here’s another way that U.S. investments abroad help American businesses: by connecting them directly with new customers and suppliers. America’s chief aid agency, USAID, uses its expertise to encourage private companies to collaborate on projects. For example, they have worked with Cargill and Land O’Lakes to help dairy farmers in East Africa raise their productivity, increasing the value of the companies’ exports to places like Kenya and Uganda. As the companies’ CEOs wrote, “This benefits not only the farmers in Africa, but food producers and their workers in the United States and it promotes goodwill in a part of the world that can be a market for more American goods in the future.” USAID has also worked with Walmart to train thousands of women farmers in sub-Saharan Africa, and with Starbucks, Keurig, and others to help coffee farmers in Latin America improve their crops so they can join the global market.
These and other efforts are part of America’s global economic leadership. Pulling back now would mean retreating from the world stage at a time when other countries are doubling down on their investments. It would deprive American companies of potential new markets and make them less competitive, while also harming the health and productivity of some of the poorest people in the world. It wouldn’t be robbing Peter to pay Paul; it would be robbing Peter and then robbing Paul too.
So it’s good for the American economy when other countries join the middle class. But how much credit does aid deserve for making that happen?
It’s a hard question to answer; growth has many causes. My own conclusion, based on years of looking at the evidence and discussing it with experts, is that although aid may not directly cause growth, there is a strong indirect connection between the two. Moving to the middle class requires a strong education system and good infrastructure, nutrition, and healthcare—and smart, targeted aid can promote those things pretty effectively.
Fighting AIDS, for example, saves lives, and it increases productivity because societies are stronger when they have healthy teachers, police officers, and entrepreneurs. Countries that worked with PEPFAR—America’s phenomenally successful effort to slow the AIDS epidemic—improved three times more on one measure of economic development than their non-PEPFAR counterparts.
Their per-capita income also grew quickly. Between 2005 and 2015, for example, Tanzania’s per-person income went up more than 37 percent. Zambia’s went up 55 percent. Ethiopia’s rose 107 percent. And as these countries grew, so did their appetite for American goods. In the same time frame, U.S. exports to Tanzania rose by more than 77 percent, U.S. exports to Zambia went up 189 percent, and to Ethiopia, 241 percent.
Many other countries are making similar gains. The point is not that aid directly makes poor people richer. It’s that aid helps create a foundation for growth. Along with many other factors, it helps remove some of the barriers that keep people from making the most of their talents. And when people in one place do better, the rest of us do better too.
We can build on this progress if the United States helps maintain the momentum. Investments in aid—which account for less than 1 percent of the federal budget—are an essential part of the solution. We need to keep making them on behalf of Americans and people around the world.

Endgame
Let’s make this the last pandemic
My new book is all about how we eliminate the pandemic as a threat to humanity.

The great epidemiologist Larry Brilliant once said that “outbreaks are inevitable, but pandemics are optional.” I thought about this quote and what it reveals about the COVID-19 pandemic often while I was working on my new book.
On the one hand, it’s disheartening to imagine how much loss and suffering could’ve been avoided if we’d only made better choices. We are now more than two years into the pandemic. The world did not prioritize global health until it was too late, and the result has been catastrophic. Countries failed to prepare for pandemics, rich countries reduced funding for R&D, and most governments failed to strengthen their health systems. Although we’re finally reaching the light at the end of the tunnel, COVID still kills several thousand people every day.
On the other hand, Dr. Brilliant’s quote makes me feel hopeful. No one wants to live through this again—and we don’t have to. Outbreaks are inevitable, but pandemics are optional. The world doesn’t need to live in fear of the next pandemic. If we make key investments that benefit everyone, COVID-19 could be the last pandemic ever.
This idea is what my book, How to Prevent the Next Pandemic , is all about. I’ve been part of the effort to stop COVID since the early days of the outbreak, working together with experts from inside and out of the Gates Foundation who have been fighting infectious diseases for decades. I’m excited to share what I've learned along the way, because our experience with COVID gives us a clear pathway for how to be ready next time.
So, how do we do it? In my book, I explain the steps we need to take to get ready. Together, they add up to a plan for eliminating the pandemic as a threat to humanity. These steps—alongside the remarkable progress we’ve already made over the last two years in creating new tools and understanding infectious diseases—will reduce the chance that anyone has to live through another COVID.
Imagine a scenario like this: A concerning outbreak is rapidly identified by local public health agencies, which function effectively in even the world’s poorest countries. Anything out of the ordinary is shared with scientists for study, and the information is uploaded to a global database monitored by a dedicated team.
If a threat is detected, governments sound the alarm and initiate public recommendations for travel, social distancing, and emergency planning. They start using the blunt tools that are already on hand, such as quarantines, antivirals that protect against almost any strain, and tests that can be performed anywhere.
If this isn’t sufficient, then the world’s innovators immediately get to work developing new tests, treatments, and vaccines. Diagnostics in particular ramp up extremely fast so that large numbers of people can be tested in a short time. New drugs and vaccines are approved quickly, because we’ve agreed ahead of time on how to run trials safely and share the results. Once they’re ready to go into production, manufacturing gears up right away because factories are already in place and approved.
No one gets left behind, because we’ve already worked out how to rapidly make enough vaccines for everyone. Everything gets where it’s supposed to, when it’s supposed to, because we’ve set up systems to get products delivered all the way to the patient. Communications about the situation are clear and avoid panic.
And this all happens quickly. The goal is to contain outbreaks within the first 100 days before they ever have the chance to spread around the world. If we had stopped the COVID pandemic before 100 days, we could’ve saved over 98 percent of the lives lost.
I hope people who read the book come away with a sense that ending the threat of pandemics forever is a realistic, achievable, and essential goal. I believe this is something that everyone—whether you’re an epidemiologist, a policymaker, or just someone who’s exhausted from the last two years–should care about.
The best part is we have an opportunity to not just stop things from getting worse but to make them better. Even when we’re not facing an active outbreak, the steps we can take to prevent the next pandemic will also make people healthier, save lives, and shrink the health gap between the rich and the poor. The tools that stop an outbreak can also help us find and treat more HIV cases. They can protect more children from deadly diseases like malaria, and they can give more people around the world access to high quality care.
Shrinking the health gap was the life’s work of my friend Paul Farmer, who tragically died in his sleep in February. That’s why I’m dedicating my proceeds from this book to his organization Partners in Health, which provides amazing health care to people in some of the poorest countries in the world. I will miss Paul deeply, but I am comforted by the knowledge that his influence will be felt for decades to come.
If there’s one thing the world has learned over the last two years, it’s that we can’t keep living with the threat of another variant—or another pathogen—hanging over our heads. This is a pivotal moment. There is more momentum than ever before to stop pandemics forever. No one who lived through COVID will ever forget it. Just like a war can change the way a generation looks at the world, COVID has changed the way we see the world.
Although it may not always feel like it, we have made tremendous progress over the last two years. New tools will let us respond faster next time, and new capabilities have made us better prepared to fight deadly pathogens. The world wasn’t ready for COVID, but we can choose to be ready next time.

Everyone, everywhere
Vaccinate the world in six months
To prevent pandemics, we need to be able to do it. Here’s how.

The greatest medical breakthrough of this pandemic—and surely one of the most important in decades—is the creation of COVID-19 vaccines. One study found that in their first year, they saved more than 1 million lives and prevented 10 million hospitalizations in the U.S. alone. The number of deaths averted around the world is of course far higher. It’s horrifying to think what COVID-19 would be doing to humanity if it weren’t for vaccines.
The world has a lot to be proud of in the creation and delivery of these vaccines. Scientists have never developed one nearly as quickly as they did in 2020, and the governments of the world have never run immunization campaigns that were as fast and as far-reaching as the ones that took place in 2021.
But there are also serious problems that we need to solve before the next potential pandemic comes along. One is the huge inequity in who has been vaccinated and who has not. It is both unjust and unwise to give a third shot to a healthy 25-year-old in a rich country before a 75-year-old cancer survivor in a poor country gets her first shot.
Another concern is that the speed with which vaccines were created was only partly a matter of skill and diligence. It was also a matter of luck.
Because coronaviruses had already caused two previous outbreaks (SARS and MERS), scientists had learned quite a lot about the structure of the virus. In particular, they had identified its characteristic spike protein—the tips on the crownlike virus you’ve seen a dozen pictures of—as a potential target for vaccines. When it came time to create new vaccines, they had a sense of what part of the virus was most vulnerable to attack.
In the next outbreak, we may not be so lucky. It could be caused by a virus that scientists haven’t studied as closely, or by one they’ve never seen at all.
This is why the world needs to adopt a serious plan for developing, manufacturing, and distributing new vaccines to prevent another pandemic. The manufacturing alone is a huge challenge: To prevent the inequities we’ve seen in COVID-19, the world needs to be ready to produce enough vaccines for everyone on the planet within six months of discovering a new pathogen. That’s 8 billion doses for a single-dose vaccine, and 16 billion for a two-dose version. In a typical year, around 5 billion or 6 billion doses are produced—that’s all vaccines combined.
The plan needs to cover four steps, starting with accelerating the invention of new vaccines.
During the pandemic, the process of creating a new vaccine got a huge boost (no pun intended). Typically, the process involves a lot of trial and error: Scientists spend years identifying weak spots in the virus and trying to identify vaccine candidates that would teach the immune system to attack them.
The creation of the first mRNA vaccines during the COVID-19 pandemic was a big step forward. They work by delivering genetic code to your body that instructs it to make shapes that look like the weak part of the virus. Your immune system notices that those shapes are foreign and sets out to attack them. Once it does, it remembers what the shapes looked like and will attack them the next time they show up. That’s what makes you immune.
One reason mRNA vaccines were so revolutionary is that they’re easily adapted for different pathogens. Once the weak spot of a virus has been identified—a process made much easier by recent advances in mapping viral genomes—it’s simply a matter of changing the genetic code in the vaccine so that it tells your body to make a new shape. This can be done in a matter of days.
As a result, the development of new vaccines will be exponentially faster—as long as researchers have the same deep understanding of future pathogens as they did of coronaviruses. So it is imperative to invest in basic research on a wider array of known viruses and other pathogens, so we understand as much as possible before the next outbreak.
Once a vaccine has been invented, the second step is to test it and get it approved for use in humans. Typically, it takes years to run all the trials necessary to prove that a vaccine is safe and effective—including time spent recruiting tens of thousands of volunteers. Assuming the vaccine proves out, it can take another year to get it authorized by the WHO and the relevant government agencies.
But when an outbreak is threatening to go global, we won’t have years. So we need ways to speed up the process without sacrificing the safety and effectiveness that people have come to expect from vaccines.
The world should build on models like the RECOVERY trial in the U.K. It set up protocols for running drug trials in advance and built infrastructure that made it much easier to get started once COVID hit. In addition, the agencies that regulate vaccines need to agree ahead of time on how volunteers will be enrolled in trials and on the software tools that will enable people around the world to sign up as soon as the disease strikes. And by connecting diagnostic tests to the trial system, we can automatically suggest to doctors that their patients should join a trial if they’re eligible.
The third step, once a vaccine has been approved for use in humans, is to make enough of it fast enough to stop the outbreak. Ending a relatively small outbreak might require hundreds of thousands of doses of a new vaccine, which is not hard to make. (The world already produces more than 5 billion doses of vaccines every year.) But countries need to be prepared for the worst—another big outbreak in which everyone needs to be vaccinated—so we must be ready to produce as many as 8 billion or even 16 billion, roughly triple the amount manufactured in a typical year.
During COVID-19, the closest thing to a breakthrough in manufacturing vaccines was the proliferation of second-source deals. These are agreements in which a company that invented a vaccine agrees to let other companies use their factories to make it. (Picture Honda Accords rolling off the line of a Ford facility.)
It’s hard to overstate the impact of second-source deals during COVID-19. In less than two years, a single manufacturer, AstraZeneca, signed second-source deals involving 25 factories in 15 countries. (AZ also agreed to forgo its profits on the COVID vaccine.) Novavax also signed one with Serum Institute of India—leading to a COVID-19 vaccine now being used in many countries—and Johnson & Johnson signed one with the Indian company Biological E. Limited and the South African firm Aspen Pharmacare. All told, second-source deals led to the production of billions of additional COVID vaccine doses.
In the future, such deals could be done even faster if companies that have them now can maintain their relationships with one another so they can hit the ground running during the next outbreak.
mRNA vaccines could also help speed up manufacturing. Many of the conventional ways to make vaccines are quite complex, so it can take a lot of time to transfer the technology and know-how from one company to another. But because the basic approach to mRNA is pretty much the same—you just swap out your old mRNA for the new one and make sure the lipid is made the right way—it should be easier to transfer between companies. There are also some new modular technologies in the pipeline that, if they prove out, will make it cheaper and easier to build and run factories that can be adapted to make different vaccines.
Finally, the fourth step in the world’s plan should be to make sure that new vaccines reach everyone who needs them—including people who live in low-income countries. In 2021, only 8 percent of people in those countries received at least one dose of a COVID-19 vaccine, while more than half of the world’s population did.
So how can the world make sure that doesn’t happen in future outbreaks?
One key is to take on the problem of vaccine hesitancy. Check out this video about how, by dealing with rumors and myths, one community in India increased its COVID-19 vaccination rate by a factor of five and created a model that other communities are now taking up:
Another key is to make sure it’s possible to manufacture enough vaccines that supply is not a limiting factor, as it was during much of 2021. Another is to make sure that vaccines are affordable for every country. Organizations like COVAX have helped with that during COVID-19. It also helps to work with manufacturers in developing countries to design new vaccines that are much cheaper to produce than existing ones. This is how the price of the pentavalent vaccine, which protects against five debilitating and deadly diseases, dropped from $3.50 per dose to less than $1 a dose—which in turn allowed the number of children who get it every year to increase by more than 16 times since 2005.
There are also a lot of innovations that make it easier to deliver vaccines. For example, auto-disable syringes have a built-in safety mechanism so health workers can’t accidentally poke themselves or use them more than once. New coolers can keep vaccines at the right temperature for longer. Advanced methods for delivering vaccines, such as replacing the needle and syringe with a small patch containing micro-needles—picture something that looks superficially like the nicotine patches that people use to stop smoking—will also help.
With these advances, it will be possible to achieve something amazing beyond preventing pandemics: eradicating entire families of pathogens. The world could rid itself of all coronaviruses, for example, or even all influenza viruses. A future without pandemics—and without the flu—is worth investing in.

A plan for the world
3 things we can do right now
If we’re going to make COVID-19 the last pandemic, the world needs to get to work right away on these key areas.

When I sat down to write my new book, my goal was to create a concrete list of steps the world could take to prevent the next pandemic. There’s a lot we can and should learn from COVID-19. But I knew that I wanted to focus more on the future instead of the past.
For decades, people told the world to get ready for a pandemic, but hardly anyone made it a priority. Then COVID struck, and stopping it became the most important thing on the global agenda. Governments need to take action now to get ready for the next pathogen, while all of us still remember how awful COVID was (and still is) and feel the urgency of never allowing another one to happen.
If we’re going to make COVID-19 the last pandemic, the world needs to get to work right away on three key areas:
1.
Make and deliver better tools.
The story of Katalin Kariko and mRNA vaccines proves that ideas for new tools must often be nurtured and researched, sometimes for decades, before they produce anything of practical value. That’s why step one in any pandemic-prevention plan should be to keep investing in better vaccines, therapeutics, and diagnostics.
You can read more about how new vaccines can be developed and delivered faster here. This includes improving our ability to test and approve new products, as well as scaling up manufacturing capacity and creating better way of delivering vaccines (like microneedle patches) so we can get out lots of doses fast.
On the therapeutics front, it took nearly two years to find effective treatments for COVID. The trajectory of the pandemic would’ve looked a lot different if we had found them sooner. We need to build out the systems that will allow us to make new treatments much faster in the future.
One key step is to create a library of antiviral compounds that are designed to attack common respiratory viruses, so that we can more easily find out if an existing drug will work in the event of an outbreak. We can also take advantage of advances in artificial intelligence and other computational methods. A computer could quickly scan a 3D model of a pathogen to figure out which drugs might be effective against it. It would be able to tell you which drugs look promising, figure out how to improve them, and, if necessary, even design new ones from scratch.
We should also expand incentives for generics manufacturers to create low-cost versions of new drugs. This can be achieved through advance orders on behalf of low- and middle-income countries, which get generic drugmakers to start manufacturing a new drug through advance orders and agreements that allow one company to manufacture a drug invented by another company even while it’s still going through regulatory approvals.
Another area where we need to spark more innovation is in diagnostics. Researchers should keep working on—and funders should keep supporting—high-throughput PCR tests, which have all the benefits of a PCR but are significantly faster at returning results, much cheaper to run, and easier to adapt to a new pathogen. We also need to support work on new types of tests that make it easier to collect samples and turn around results quickly, like better versions of the rapid antigen tests that many of us now take at home for COVID or even handheld devices that health workers can use to easily test people in their community. And testing should be tied to treatment, so if you test positive, you get the medication you need right away.
2.
Improve disease monitoring.
Creating the GERM—Global Epidemic Response and Mobilization—team is one of the most important steps we can take to stop the next pandemic. GERM will play a crucial role in virtually every aspect of pandemic prevention, but improving monitoring will be the most significant part of their mandate.
GERM is only one piece of the puzzle, though. Another crucial step is to improve civil registration and vital statistics in the developing world. At a minimum, many low- and middle-income countries need stronger registries of births and deaths, so that GERM can work with local organizations to more easily spot if there’s an unusual pattern worth investigating. Then, building on that foundation, countries should expand into autopsies that use minimally invasive tissue samplings, wastewater surveillance, and other practices.
The world’s disparate disease monitoring systems also need to be integrated so that public health officials can rapidly detect pathogens. Data must be made available in real time, with test results integrated into the public health system so that officials can watch for outbreaks. And in countries like the United States, where testing can be extremely expensive, governments need to make diagnostics cheaper and more accessible to everyone.
Finally, we need to expand our capacity to sequence the genomes of pathogens in order to track new variants. We should double down on investments in projects like the Africa Pathogen Genomics Initiative, a network of labs across the continent that share genomic data with each other, and in new tools that will let us sequence more genomes in more places.
3.
Strengthen health systems.
Good health care starts with good health systems. That’s true for basic care, and it’s especially true for pandemic prevention. When a new or deadly pathogen emerges, you need somewhere for sick people to reliably seek treatment. You need health workers who can identify potential threats and the infrastructure to report anything out of the ordinary. And, once a pathogen starts to spread, you need trained professionals who can administer higher level tests, treatments, vaccines, and more.
The pandemic devastated health systems around the world, but the need in low-income countries is especially acute. The fundamental challenge is that they don’t have the funding, expert capacity, or institutions they need to offer basic health services to all their people, let alone manage a major outbreak. And during the pandemic, the problem got worse, as many rich governments cut foreign aid or took money from work on other diseases and redirected it to COVID.
We need to reverse this trend. A major part of the Gates Foundation’s work has been to help improve health systems—investments that both save lives, end preventable infectious diseases, and pave the way for economic growth. But philanthropy alone cannot close the gap between rich and poor countries. The models for wealthy countries are still Sweden and Norway, who each give at least 0.7 of their GDP in aid. If we’re going to be serious about preventing the next pandemic, we need to not just go back to pre-COVID aid levels but increase investments in strengthening health systems (which will also help shrink the overall health gap between the rich and the poor).
For their part, low- and middle-income countries should focus on health spending that achieves many things at once. For example, hiring more health workers gives you more people who can manage malaria cases, offer HIV testing and treatment, and give public officials unprecedented insight into what’s causing illness and death in their country.
But as COVID made clear, low- and middle-income countries aren’t the only ones that need to strengthen their health systems. There are steps that countries at every income level should consider, like improving primary health care and deciding in advance of a crisis who will oversee what. Governments and donors also need a global forum where they can coordinate action with poor countries.
All of these efforts—new tools, better disease surveillance, and improved health systems—won’t be cheap, but they will save lives and money in the long run. I estimate that, over the next decade, governments combined need to spend $15 to $20 billion per year to develop the tools we need. Strengthening health system will cost the world an extra $30 billion a year, on top of the money we should already be spending to improve health in low income countries.
That sounds like a lot of money until you learn that the International Monetary Fund estimates this pandemic will cost $12.5 trillion over just five years. Think of it like insurance. This is the billions we need to spend in order to save millions of lives and trillions of dollars.
And here’s the best news: Even when we’re not facing an active outbreak, these investments will make people healthier, save lives, and shrink the health gap between the rich and the poor. This is an opportunity to not just stop things from getting worse but to make them better.
We don’t need to surrender to living in perpetual fear of another global catastrophe. But we do need to remain aware of the possibility and be willing to do something about it. I hope the world seizes this moment and invests in the steps needed to make COVID-19 the last pandemic.
The outbreak squad
Meet the GERM team
Creating the GERM team is one of the most important things we can do to prevent the next pandemic.

At the beginning of the movie Outbreak, there’s a scene where three government virologists arrive by helicopter at a remote village. Most of the village has recently died from Ebola-like symptoms. Wearing protective moon suits while triumphant music plays in the background, our heroes immediately get to work trying to contain the threat before it hurts anyone else. It’s an inspiring scene.
Unfortunately, it’s pure Hollywood fiction.
A full-time team like this doesn’t exist in real life—yet. I’m hoping this changes soon, because it is one of the most important things we can do to prevent the next pandemic.
Today, there are many organizations that work hard to respond to a major epidemic, but their efforts are largely dependent on volunteers. The best known is the Global Outbreak Alert and Response Network, or GOARN, which does heroic work but doesn’t have the staffing, funding, or global mandate to tackle every threat.
We need a permanent organization of experts who are fully paid and prepared to mount a coordinated response to a dangerous outbreak at any time. In my book, I propose that we call this group the GERM—Global Epidemic Response and Mobilization—team.
The GERM team would be made up of people from all over the world who have a wide range of expertise: epidemiology, genetics, data systems, diplomacy, rapid response, logistics, computer modeling, communications, and more. When they aren’t actively working in the field, most of them would call individual countries’ public health agencies home base, though some would sit in the WHO’s regional offices and at its headquarters in Geneva. (I talked about GERM at length in my TED talk last month.)
It's important that GERM have a diverse workforce. The team is going to serve the entire world—it only makes sense that its members reflect the experiences and backgrounds of the people they’re going to work with. Ideally, GERM would have a high number of local experts from countries at a higher risk of outbreak, and outsiders would only show up when necessary and when the in-country team requests help.
Here’s how a GERM response would work: The team’s disease monitoring experts would look for potential outbreaks. Once it spots one, GERM should have the ability to declare an outbreak and work with national governments and the World Bank to raise money for the response very quickly. Product-development experts would advise governments and companies on the highest-priority drugs and vaccines. People who understand computer modeling would coordinate the work of modelers around the world. And the team would help create and coordinate responses, such as how and when to implement border closures and recommend mask use.
But GERM’s response to an active outbreak is only one part of their work.
The team’s most important job is helping to run outbreak response exercises that test whether the world is ready for the next major outbreak. Militaries regularly run war games to evaluate their readiness—we should do the same with disease threats. In most countries, these exercises can be run by local public health and military leaders, with GERM acting as an advisor and reviewer. For some low-income countries, the world should invest in building this capacity and lend resources as needed.
You can learn more about what these germ games would look like by reading chapter 7 of How to Prevent the Next Pandemic, which is available as a free download for all Gates Notes Insiders.
The GERM team would also be responsible for developing a checklist for pandemic preparedness, similar to the ones that airplane pilots follow before every takeoff and many surgeons now use during an operation. A checklist sounds like such an obvious tool, but very few places had a plan like this in place when COVID hit. A GERM-developed checklist could be used anywhere and help make sure that governments are ready with an efficient and effective response.
But GERM’s impact won’t be limited to stopping pandemics. The group will improve overall health around the world, especially in the poorest countries.
Emerging diseases will always be their top priority, but when there isn’t an active pandemic threat, the team will keep their skills sharp by helping out with deadly diseases like polio and malaria. For example, they could work alongside public health workers in Nigeria to help distribute millions of doses of the oral polio vaccine every year to keep the country polio-free. This would both save a lot of kids from needless suffering and help the GERM team build relationships with communities they will need if an outbreak strikes. Now that’s what I call getting your money’s worth!
Running GERM will cost the world around $1 billion a year to cover salaries for the force of 3,000 people we’d need, plus equipment, travel, and other expenses—money that would come from governments. The work would be coordinated by the WHO, the only group that can give it global credibility, and it needs to be accountable to the public.
When Hollywood gets something wrong, the result is usually pretty silly and unrealistic. But movies like Outbreak nailed it when they imagined a global disease-fighting team who is ready to respond to a crisis on a moment’s notice. If we’re going to make sure that COVID-19 is the last pandemic, we need the GERM team.

Live from Vancouver
Talking about the last pandemic at TED
A lot has changed since the last time I spoke on the TED stage.

Last week, I went to the TED conference in Vancouver. It was my first time back at TED since 2015, when I gave a speech about how the world wasn’t ready for the next epidemic.
A lot of people watched that talk, but almost all of the views came after the start of the COVID-19 pandemic. This time, I spoke about the same subject, but a lot had changed. No one in the audience needed to be convinced that a deadly virus could kill millions of people around the world and upend our lives.
My talk was all about how we can make COVID-19 the last pandemic. I believe we can eliminate the threat of pandemics completely if we approach infectious diseases like we approach fires. We need a well-oiled system in place, complete with full-time professional personnel and innovative tools ready to be deployed at a moment’s notice.
You can watch my full talk here:
Giving a TED talk is always a memorable (and nerve-wracking!) experience. I started thinking about what I wanted to say a couple months ago. I decided to focus on what I call the GERM—Global Epidemic Response and Mobilization—team, a new full-time, paid group whose entire job is to prepare for the next outbreak. I talk a lot about GERM in my upcoming book, but this was the first time I was going to speak about GERM publicly at length.
One of the coolest things about TED is how visual all the talks are. I had the opportunity to make sure the graphics for mine looked okay during a rehearsal. I also got to practice bringing the Roman fire brigade bucket I was using as a prop onto the stage. (It’s a lot heavier than it looks!)
Learning from Munich & Islamabad
The innovations and investments that do double duty
Health systems developed to fight longstanding infectious diseases have been critical for COVID—and vice versa.

Last week, I traveled to Germany to attend the 58th Munich Security Conference, a gathering of leading experts on global security, health, development, and international relations. After learning from and working with so many of them virtually for two years, I was eager to hear from heads of state and global health leaders—in person at last!—about the ongoing impact of COVID-19 on their countries, the infectious disease and inequity challenges they’re still contending with, and what we need to be doing now to prevent future pandemics.
Health security was already a big priority at the MSC in pre-COVID times, but this year’s conference underlined how much global health is now rightfully seen as a serious national and global security issue. It’s clearer than ever that investing in health R&D, disease surveillance, and strong health systems is critical to keeping people safe, wherever they live in the world.
In Munich, I took part in a panel discussion that included the foreign ministers of Canada and Sweden, the CEO of the Crisis Group, and remarks from Tedros Adhanom Ghebreyesus, the director-general of World Health Organization. These leaders hit on the same themes I heard from many others I talked with on this trip—themes I’ve given a lot of thought to while writing a book about how to prevent the next pandemic. For one, when it comes to COVID, we’re not out of the woods yet, because the virus is still mutating. At the same time, the pandemic is evolving, with vaccines plus the rapid spread of Omicron appearing to offer many more people some protection against severe disease. Meanwhile, COVID continues to exacerbate existing inequities—something we’ll feel the effects of for years to come.
In all countries, especially the poorest, the pandemic is still hindering the prevention and treatment of other diseases. The world’s response must continue prioritizing equity and protecting the most vulnerable. We need an integrated approach that manages COVID for the long haul alongside other infectious diseases such as HIV, TB, and malaria, which continue to kill millions. This will enable countries to take limited resources and apply them where they are needed most, whether by mitigating COVID risks, supplying insecticide-treated nets against rising malaria cases, or making up for lost ground with other life-saving vaccinations.
Another theme that came up in Munich is the need for stronger health systems and tools to prevent, detect, and respond quickly to emerging and existing infectious diseases. We discussed how this can prevent future pandemics and what role multilateral cooperation must play. For example, the effects of COVID would have been much worse without investments made to fight other infectious diseases like HIV, TB, malaria, and polio. For decades, countries like Pakistan, Kenya, and South Africa have strengthened their health systems by training community health workers, building surveillance and lab capacity, creating efficient supply chains, and accelerating innovation.
The world’s response to COVID was far from perfect, but these advances helped put some countries in a better position to pivot and defend against the virus. And they helped mitigate the pandemic’s impact on these countries’ ability to fight other diseases.
Take the Global Polio Eradication Initiative. Thanks to investments made by governments, the private sector, and philanthropy, wild polio cases are at a historic low, and the disease is endemic in just two countries: Pakistan and Afghanistan. Last week I also went to Pakistan, where I visited two of the country’s innovative command centers for fighting diseases, the National Emergency Operations Center for polio eradication and the National Command and Operation Centre for COVID. The NEOC uses state-of-the-art informational tools developed by GPEI to track polio so that no child is ever paralyzed by it again. The NCOC has applied resources and lessons learned from the polio program—including data analysis, vaccine campaign planning, and community engagement—to coordinate Pakistan’s response to COVID. Both centers blew me away.
At the NEOC, we pored over a wall of screens that displayed an up-to-the-minute summary of immunization rates and areas where children have not been reached with the vaccine. The health officials I talked to in Pakistan told me that the polio program’s infrastructure was invaluable once COVID hit. By setting its priorities based on the needs at the time, Pakistan was able to expand and redirect health infrastructure that had been supported by the global community—the national help line call center, communication systems, and networks of religious leaders and community influencers—to help protect people during the pandemic.
It’s easier to ramp up testing and deliver vaccines and protective gear during a pandemic when you already have a community health workforce, labs, surveillance capacity, and supply chains in place. Another organization that has proven invaluable over the last two years is the Global Fund, which funds more than half of all global programs working to end AIDS, tuberculosis, and malaria. The Global Fund’s partnerships with countries enabled community health workers who go door to door to detect, diagnose, and report fevers as malaria or COVID. Along the same lines, organizations like the Coalition for Epidemic Preparedness Innovations, which accelerates work on vaccines for infectious diseases, and Gavi, which has immunized nearly 1 billion children since 2000, have been key partners in developing and distributing COVID vaccines.
Unfortunately, this isn’t a simple success story. We’ve also seen increases in cases and deaths from malaria, HIV, and tuberculosis for the first time in 20 years because of COVID. But the backsliding was not nearly as bad as it could have been.
I’m optimistic about the future. We have learned so much from COVID, and the innovations have been tremendous. Talking to public health leaders in Munich and Islamabad, it’s clear that long-term funding for global health—including investments in proven initiatives like GPEI, Global Fund, and CEPI —helped save millions of lives during this pandemic. Just think: It took less than a year after the virus emerged to develop a vaccine against it. I believe we’ll do even better next time and can deliver them to everyone within six months of an outbreak if we build enough global capacity.
As the pandemic continues to evolve and the world adapts strategies and investments to match, we can apply these lessons and make choices that help prevent future pandemics. We need a full-time global team dedicated to responding to new disease outbreaks and working to end other infectious diseases. We should, above all, approach this work with a greater focus on improving inequities by understanding that investments in global health and pandemic prevention are critical security issues. And they’re mutually reinforcing.
Now is the time to build on these lessons, increase our funding for the basic building blocks of public health, and support countries in meeting their needs. If we make the right choices and investments now, we can end other devastating diseases and make COVID-19 the last pandemic.

Pathogen prevention
In Africa, detecting disease outbreaks before they become a global threat
Using genomic sequencing technologies, this hero is working to prevent the next pandemic.

While promoting my new pandemic book the last month, I’ve been telling audiences and interviewers that if we want to make COVID-19 the last pandemic, we need to combat infectious diseases the same way we fight fires.
Just like we have a robust system of fire alarms, firefighters, and fire hydrants to help detect and extinguish fires, we need to create an equally effective system to identify and respond to new disease outbreaks.
This firefighting comparison is also a useful way to understand the amazing work of Sofonias Tessema.
Officially, Sofonias is the program lead for the Africa Pathogen Genomics Initiative at the Africa Centers for Disease Control and Prevention or Africa CDC. But in firefighting terms you might think of him as a fire safety officer who is building a network of fire watchtowers and smoke detectors across Africa.
Instead of looking out for the first signs of a fire before it can spread, however, Sofonias is focused on quickly detecting deadly pathogens before they can grow into a global threat. And instead of using watchtowers and smoke detectors, he relies on powerful genomic sequencing technologies to spot disease outbreaks.
Genomic sequencing allows scientists to read the DNA and RNA of pathogens and understand what they are, how they spread from one person to another, and develop counter measures like vaccines. During COVID-19, this technology has been an invaluable tool for identifying new variants, tracking the evolution and spread of the virus, and guiding public health responses.
Advances in this technology have made it easier, faster, and cheaper to do genomic surveillance. Over the last two decades, the price of sequencing a full human genome has fallen dramatically. And one company, Oxford-Nanopore, has even developed a portable gene sequencer that can be operated with a laptop and no need for a lab, allowing health officials to conduct genetic testing in remote areas where outbreaks may occur.
As powerful as genomic sequencing technologies have become, many countries have not taken full advantage of them. Building genomic disease surveillance capacity presents challenges because it requires investments in labs, expensive equipment, and specially trained personnel. While the COVID-19 pandemic has sparked new interest in using genomic sequencing to improve disease surveillance, many parts of the world are still working to strengthen their capacity to use this critical technology.
In 2019, Sofonias joined the Africa CDC to establish a continent-wide genomic disease surveillance network. One of Sofonias’s first projects was to conduct an assessment to understand how many African nations were prepared to use this technology.
The results, Sofonias said, were shocking.
Of the African Union’s 55 member states, just seven had public health institutions with trained personnel and equipment to do genetic sequencing.
Given the scale of the job before them, Sofonias and his team had planned for a phased approach to help African nations build genomic surveillance capabilities. They had to acquire the technology, hire and train the technicians to operate them, and create the data systems so governments can analyze and share the genetic information and use it to inform public health decisions. Building this system would take time.
But the Africa CDC soon learned that time was a luxury they didn’t have. Within weeks of Sofonias joining the Africa CDC, the first cases of COVID-19 were detected in China. And two months later, the first cases were identified in African countries.
It’s hard to overstate the challenge before Sofonias and the Africa CDC. While genomic surveillance had been used during Ebola, Lassa fever, and cholera outbreaks, bringing this technology to scale posed many challenges in Africa, where many countries did not have the infrastructure or trained personnel to run these labs.
But this was just the kind of challenge Sofonias had always been eager to take on.
Born in Ethiopia, Sofonias grew up in a rural town where malaria was always a major threat. Seeing people die and suffer from the mosquito-borne disease got him interested in a career in public health. He earned a PhD in malaria genomics, an emerging field of research that uses genetic data of the malaria parasite to advance malaria eradication efforts. After graduate school, he was working as postdoctoral fellow at the University of California in San Francisco, where he was focused on how genomic data combined with mobile phone data could help researchers understand how malaria spreads from one country to another.
In 2019, when a call came from the Africa CDC asking if he would use his knowledge of genomic surveillance technologies to help Africa, he jumped at the opportunity. Sofonias saw the untapped potential of this new technology to make more informed public health decisions in Africa. And after years living abroad, he was also excited to return home to Ethiopia, where the Africa CDC is based.
Sofonias and his team scrambled to quickly build up Africa’s capacity to do genomic disease surveillance. The Africa CDC focused first on scaling up COVID-19 testing capabilities. At the beginning of the pandemic, only two African nations had the ability to perform PCR COVID tests, highly accurate tests that detect genetic material from the virus.
At the same time, his team worked to acquire next-generation sequencing technologies (NGS) for Africa. NGS technologies offer a more efficient, accurate, and cheaper way for researchers to track the slightest genetic changes in pathogens which may cause disease outbreaks. This effort received support from a group of public, private, and non-profit partners including the African Union, Illumina and Oxford Nanopore, which produce next-generation sequencing machines, the US Centers for Disease Control and our foundation.
Thanks to Sofonias and the rest of the Africa Pathogen Genomics Initiative team, 31 African nations now have the capability to do genetic sequencing for surveillance of COVID, malaria, cholera, Ebola, and other diseases.
Despite this progress, much remains to be done. Sofonias’s team faces challenges in bringing this technology to all African nations. Access to the equipment needed in the labs has been delayed because of global supply chain disruptions. Training enough lab technicians and data scientists to process and analyze the samples has been difficult. Finally, more coordination is needed between countries to share their genetic data and use it to inform collective health responses.
But every month, Sofonias’s team continues to strengthen and expand the system across the continent. The goal is to create a seamless, integrated network that includes laboratories at the community level, which can spot the first signs of an outbreak, perform genomic testing of pathogens, and analyze the results to guide a public health response.
“Our vision is bold. Our vision is optimistic. We always push forward and continue to work with the countries to show that this is actually feasible,” he said. “It really makes me hopeful that this technology can improve outbreak detection and response in Africa.”
Sofonias shared the progress and challenges of building a genomic disease surveillance network with a group of graduate students who participated in a recent Gates Notes Deep Dive on pandemic prevention.
Pioneering research
She helped change vaccines forever
Long before most of us heard of mRNA vaccines, this hero saw their potential to save lives.

For most people, the highly effective mRNA COVID vaccines made by Moderna and Pfizer-BioNTech seemed to come out of the blue. But these new vaccines, which were essential to end this pandemic and will likely play a critical role in preventing future pandemics, are the product of decades of painstaking work by researchers.
One of those researchers is Dr. Katalin Karikó, a Hungarian biochemist who long ago saw the potential of mRNA to save lives when few others did.
The daughter of a small-town butcher in Hungary, Karikó knew from a young age that she wanted to become a scientist. She was drawn to biochemistry and developed a particular fascination with messenger RNA, or mRNA, molecules that (among other things) direct the creation of proteins in your body.
Messenger RNA functions as a kind of middleman—it carries the directions for making proteins from your DNA to the factories in your cells where the proteins will be assembled. It’s a bit like the waiter in a restaurant who writes down your order and takes it to the kitchen, where the cooks will make your meal.
In the 1980s, while working on her PhD in her native Hungary, Karikó became convinced that tiny strands of mRNA could be injected into cells to send instructions to the body to make its own medicines. She was interested in developing mRNA treatments for stroke, cancer, and other diseases.
Although vaccines were not the focus of Karikó’s work, other researchers saw that it would be possible to use mRNA to make those as well—for flu, coronaviruses, and maybe even various forms of cancer.
Using mRNA to make vaccines would be a major departure from the way most vaccines work. Many conventional vaccines operate by injecting a weakened or dead form of the virus you’re trying to stop. Your immune system sees the new shapes on the virus, kicks into gear, and builds up immunity. While conventional vaccines have been very effective, it takes years of lab work and clinical studies to make sure that they are safe and will produce a good immune response.
The idea behind mRNA vaccines was quite clever. Since mRNA takes the orders for proteins from the DNA and delivers them to the cooks in your cells’ kitchen, what if we could change those orders in a very targeted way? By teaching your cells to make shapes that match shapes on the actual virus, the vaccine would trigger your immune system without having to introduce the virus itself.
If they could be made, mRNA vaccines would be a huge advance over conventional vaccines. Once you had mapped out all the proteins that make up the virus you wanted to target, you’d identify the one that you want antibodies to grab. Then you’d study the virus’s genetic code to find the instructions for making that protein, and you’d put that code into the vaccine using mRNA. If, later, you wanted to attack a different protein, you’d just change the mRNA. This design process would take at most a few weeks. You would ask the waiter for fries instead of a side salad, and your immune system would do the rest.
There was just one problem: It was only a theory. No one had ever actually made an mRNA vaccine. What’s more, most people in the field thought it was crazy to even try, not least because mRNA is inherently unstable and prone to degrading quickly. Also, cells have evolved to avoid being hijacked by foreign mRNA, and there would need to be a way of getting around this defense system.
Karikó’s interest in mRNA eventually brought her to the U.S. And in 1993, while doing research at the University of Pennsylvania, Karikó and her boss managed a feat that told them they were on to something: They got a human cell to produce a tiny amount of new proteins using a modified version of mRNA that had been altered so it could get past the cell’s defense system. This was a breakthrough, because it meant that if they could expand the production dramatically, they would be able to make a cancer treatment using mRNA.
Stories of medical discoveries often don’t travel in straight line from breakthrough to lifesaving impact. And Karikó’s story is no different. Karikó’s work lost momentum when her boss left academia for a biotech firm. She no longer had a lab or financial support for her work; although she applied for grant after grant, every application was rejected. In 1995, she had a cancer scare, she was taken off the tenure track at work, and her husband was stuck in Hungary because of a problem with his visa. But Karikó was undeterred.
Then in 1997, she began working with Drew Weissman, a new colleague who came to the University of Pennsylvania with a promising background: He had done a fellowship at NIH under the supervision of Tony Fauci, and he was interested in using Karikó’s work on mRNA to develop vaccines.
Together Karikó and Weissman kept pursuing the idea of working with mRNA that had been engineered in a lab. But they still had to get more mRNA past the cell’s defense systems, a problem that other scientists helped solve. In 1999, a cancer researcher named Pieter Cullis and his colleagues proposed that lipids—basically, tiny bits of fat—could be used to encase and protect a more delicate molecule, such as mRNA. Six years later, working with Cullis, biochemist Ian MacLachlan did it for the first time. The lipid nanoparticles he developed paved the way for the first mRNA vaccines.
As late as 2010, hardly anyone in the federal government or private industry was interested in trying to make vaccines using mRNA. Major pharmaceutical companies had tried and failed, and some scientists felt that mRNA would never trigger enough of a response in the body. But an official at DARPA, the little-known research program for the U.S. military, saw enough promise in the technology that he started funding mRNA vaccines for infectious diseases.
As pioneering as this work was, it didn’t lead immediately to new vaccines. Accomplishing that would be the task of companies dedicated to translating the breakthrough into a product that could be approved and sold; the U.S.-based Moderna and Germany-based CureVac and BioNTech were founded to do just that.
In 2014, Karikó joined BioNTech, which was working on an mRNA vaccine for cancer. Early efforts didn’t work, although a test of a rabies vaccine showed promise. Still, Karikó and her BioNTech colleagues persevered, as did scientists at Moderna. When COVID hit, they immediately set out to make a vaccine for the new virus. It was a good bet.
The notion that mapping a virus’s genome would allow you to create an mRNA vaccine in a matter of weeks proved to be exactly right. In March 2020, just six weeks after scientists sequenced the COVID virus’s genome, Moderna announced that it had identified an mRNA-based candidate and begun making it for clinical trials. On December 31, the mRNA vaccine made by BioNTech in partnership with Pfizer was approved for emergency use by the World Health Organization. When Karikó received the first dose of the vaccine she had done so much to create—a few days before it was officially approved—she wept.
For all her amazing foresight, I doubt even Dr. Karikó imagined that mRNA vaccines would one day play an essential role in ending a pandemic – and giving us a tool to prevent the next one. And to me, that’s the important lesson of her story: It’s impossible to predict exactly how breakthroughs will shape the future. That’s why it’s critical, if the science makes sense, that we should be willing to bet on crazy sounding ideas and the researchers like Dr. Kariko willing to fight tooth and nail to pursue them. They just might change the world.

Heroic acts
Meet the heroes in Africa fighting back against this pandemic—and working to prevent the next one
As Africa faces many challenges during the pandemic, these heroes are making a difference.

In Africa, the latest statistics on COVID-19 are discouraging. Just 6 percent—about 78 millionof the continent’s 1.3 billion people have been fully vaccinated. Worldwide, by comparison, 43 percent are fully vaccinated, and boosters are now widely available in many countries.
Without enough vaccines available in Africa, COVID-19 marches on infecting millions of people. Even assessing the true scale of the pandemic on the continent is difficult. A recent World Health Organization assessment estimated that only one in seven cases of COVID in Africa are being detected because of a limited amount of testing.
And while many Western and Asian countries are recovering economically from the pandemic and returning to some version of normalcy, most countries in Africa continue to struggle. Disruptions to schooling, health care, and livelihoods have sunk many families deeper into poverty, leaving them without enough food and basic services.
We should all be upset about this inequity. (I’ve written recently about this divide and the steps the world needs to take to get the virus under control.) It’s critical that more be done to get vaccines into the arms of the people at high risk for COVID, including the elderly and immunocompromised, who are living in low-income countries. And the recent detection of the Omicron variant serves as a reminder of how important increasing vaccination rates is to deter new mutations of the virus from emerging.
But even during this difficult time, I think it’s important to highlight the many Africans who are fighting back against this pandemic. They are stepping up to alleviate suffering, to combat misinformation, and to develop the tools needed to prevent future pandemics.
There are thousands of examples of heroic work being done in Africa during this pandemic. Here are three stories of organizations and individuals who are working to save lives and bring hope to their communities.
1. South Africa: The Truck
As COVID-19 swept across South Africa, one of the most pressing needs was access to public health information. People needed to know about the virus and how to stay safe. And as South Africa started rolling out COVID vaccines this year, health officials were also tasked with counteracting the spread of misinformation about the virus and vaccines. This was especially challenging in hard-to-reach communities in South Africa, where people don’t have access to television and other media. But UNICEF, in partnership with the national government, had an answer to this challenge: A truck. Not just any truck but a multi-media messenger on wheels. The truck has LED screens, which allows the truck’s organizer to broadcast videos telling local stories about COVID-19. They also organize presentations in communities to raise awareness of the virus, teach people how to prevent its spread, and promote COVID testing and vaccinations. The truck has logged more than 40,000 miles and delivered messages to hundreds of thousands of people.
2. Lesotho: Mamello Makhele
Mamello Makhele is a nurse-midwife working to improve health care for women in rural Lesotho, where there are high rates of maternal mortality. During the pandemic lockdowns many health facilities closed, leaving women living in these remote communities without access to family planning services. On foot and by donkey, Mamello travels high into the mountain to offer health care, deliver babies, and distribute contraceptives. Mamello has also worked nationwide to empower young women, encouraging them to take control of their health and prevent unwanted pregnancies. Thanks to her incredible work, many women are healthier today in Lesotho.
3. Tanzania: Afyadata
Even as the world seeks to end the current COVID-19 pandemic, we need to also be thinking about how to prevent future pandemics. That’s just what a mobile app called Afyadata is helping health officials do in Tanzania. Designed by the Southern African Center for Infectious Disease Surveillance (SACIDS), Afyadata is a digital surveillance tool that allows health workers and even ordinary people to serve as disease detectives. Users can report unusual health occurrences not only in humans, but also animals. Monitoring animals is critical because most new pathogens start in animals before they spread and sicken humans. With the app, farmers can easily report any suspicious illness among their livestock to health officials, who can then quickly follow up with further investigation, if necessary. While this app is still being piloted in several districts of Tanzania and other parts of Africa, it has already been effective in the detection and identification of several small disease outbreaks. I look forward to learning more about Afyadata’s progress.
Inspiring acts
7 unsung heroes of the pandemic
Incredible people caring for those in need during COVID-19.

When I was a kid, my image of a hero was largely inspired by my dad’s collection of early Superman comics. I read them all. A “hero” was somebody who had supernatural powers like flying, laser vision, or the strength to bend steel.
As humans, of course, we’re all pretty limited in our physical powers. We don’t fly. We can’t see through walls. But what’s unbounded in us is our ability to see injustices and to take them on—often at great risk to ourselves.
My work in global health and development has introduced me to many extraordinary heroes with this kind of superpower. And I’ve had the honor of highlighting many of them on this blog: An epidemiologist who helped eradicate smallpox. A doctor working to end sexual violence in Africa. A researcher working to end hunger with improved crops. Just to name a few.
Why do we need heroes?
Because they represent the best of who we can be. Their efforts to solve the world’s challenges demonstrate our values as a society and they serve as powerful examples of how to make a positive difference in the world. And if enough people hear about their actions, they can inspire others to do something heroic too.
If there’s ever been a time that we need heroes, it’s now. The COVID-19 pandemic has created unprecedented health and economic challenges, especially for the most vulnerable among us. The good news is that many people from all walks of life are doing their part to help them. Health care workers. Scientists. Firefighters. Grocery store workers. Aid workers. Vaccine trial participants. And ordinary citizens caring for their neighbors.
Here are portraits of a few individuals from around the world working to alleviate suffering during this pandemic. I hope their stories inspire you just as much as they have me.
To these heroes and heroes everywhere, thank you for the work you do!

Abundant air
Breathing new hope into Africa’s fight against COVID-19
In Africa’s battle against COVID-19, a Kenyan doctor is making sure every breath counts.

As the COVID-19 pandemic spreads across Africa, hospitals across the continent face shortages of essential medical supplies needed to treat the respiratory disease and keep patients alive.
Not just masks and ventilators, but oxygen.
For people living in wealthy countries, medical oxygen is often taken for granted. In many low-income countries, however, oxygen is often in short supply or not available at all. And globally, a lack of oxygen –needed to treat pneumonia, malaria, and other diseases—leads to hundreds of thousands of deaths each year.
Addressing this often overlooked challenge is the life’s work of Bernard Olayo, a Kenyan doctor who founded Hewatele, an innovative organization working to ensure all patients—even in remote areas of the country—have access to oxygen.
Now, he is playing a critical role in Kenya’s preparations to tackle COVID-19 by scaling up oxygen supplies that will be needed to keep the most critically ill patients alive.
While the number of COVID-19 cases in Africa remains low compared to other parts of the world, the continent is bracing for a surge of infections. According to the World Health Organization, up to 190,000 people could die of COVID-19 in Africa if the disease is not controlled. A widespread outbreak would flood many of Africa’s fragile health systems.
A lot of attention has been focused on the lack of ventilators in Africa. Ventilators are the mechanical devices that help patients breathe, pushing air in and out of their lungs, when they can’t on their own. And the shortage of them is a real problem. But the lack of oxygen itself is equally worrying. The coronavirus attacks the respiratory tract, inflaming the lungs and making it difficult for patients to breathe. Oxygen, delivered through a mask or nasal tube, is an essential and effective first line of treatment that’s less invasive than being on a ventilator. Oxygen is also needed to run a ventilator. If COVID-19 patients have access to oxygen as an initial treatment, however, it may prevent many of them from becoming so critically ill that they would require one of the limited number of ventilators to breathe.
What Bernard is hoping to avoid during this pandemic are the painful choices he faced as a young doctor because of a lack of oxygen. After medical school he was posted to a rural hospital, where many of the patients were children battling pneumonia who needed oxygen for treatment. But Bernard soon learned that there was never enough oxygen available. He and the other hospital staff often had to share a single cylinder of oxygen between patients. When there were too many patients and not enough oxygen, he and other doctors would be forced to decide which children would receive oxygen and live, and which would go without it and sometimes die—a choice that broke his heart, he says.
That experience inspired Bernard to investigate the source of Kenya’s oxygen supply shortages. He discovered that one of the biggest challenges is that oxygen is expensive in Africa. In Kenya, oxygen costs about 13 times more than what it does in the United States. The high cost was driven, in part, by a lack of competition. In many countries, including Kenya, there was just a single oxygen supplier for the entire country. And with many health facilities located hundreds of miles away from the oxygen plants, transportation costs drove up prices even higher. The long distances and poor roads also meant that deliveries were unreliable. Hospitals and clinics would regularly run out of oxygen supplies.
In 2014, Bernard founded a public-private partnership to try a new approach that would make access to medical oxygen more affordable and reliable. He named the organization Hewatele (Swahili for “abundant air”). Given the delivery challenges in Kenya, Bernard decided to build oxygen plants at several of the busiest hospitals in the country, where demand is highest and reliable electricity for production is available. The oxygen is then sent out for delivery using a milkman model, with oxygen cylinders regularly dropped off at remote hospitals and clinics and the empty cylinders returned to be refilled. This system ensures that there is always more than enough oxygen available at each facility. Using this new approach, Hewatele has cut the market price for oxygen in Kenya by 50 percent. Now, Bernard is working to expand the number of oxygen plants in Kenya and bring Hewatele’s business model to other parts of Africa.
While the COVID-19 pandemic has brought much needed attention to the oxygen gap in Africa, more needs to be done to ensure that everyone has access to this simple medical intervention. Thanks to Bernard’s efforts, progress is being made. His work has already helped save the lives of thousands of children and adults and will save many more in the future—one breath at a time.

High hopes
This organization is working to create a world without pandemics
The Coalition for Epidemic Preparedness is working to make sure we never again experience the hardship of a pandemic.

Here’s a fact that’s hard to believe: At this time two months ago, the world did not yet know about the omicron variant.
It’s both remarkable and horrifying how quickly omicron has become the dominant cause of COVID-19 in many countries. In just seven weeks, it has led to record-high case numbers and hospitalizations around the world. I’m still optimistic that the pandemic can come to an end sometime in 2022, but first we have to contend with a virus that’s spreading faster than any other in history. (I recently had a good discussion about this with global health Professor Devi Sridhar.)
The omicron surge has been an unfortunate reminder that the only way to eliminate the threat of COVID-19 somewhere is to eliminate it everywhere. As long as the virus continues to circulate at a high level in some parts of the world, we’ll always be at risk for another devastating variant. Game-changing innovations—including vaccines and new antivirals—will save lives but won’t truly accelerate the end of the pandemic until they’re accessible to everyone.
That’s why the Gates Foundation is renewing its investment in the Coalition for Epidemic Preparedness Innovations, or CEPI. I’m excited to announce a new $150 million commitment to its future work on COVID and beyond.
Our foundation helped create CEPI in 2017 to accelerate work on vaccines against new infectious diseases and make sure those vaccines reach people in the poorest countries. The organization has played an invaluable role in the COVID-19 pandemic as one of the leaders of COVAX, the global effort to get vaccines out to low- and middle-income countries.
As with malaria, polio, and many other diseases that our foundation works on, the key to pandemic prevention and preparedness is to keep on innovating. This pandemic’s most significant innovation is mRNA vaccines, which were available less than a year after the virus that causes COVID was identified. CEPI began funding efforts to develop mRNA vaccines for COVID just days after the virus was detected outside of mainland China. (One of the candidates CEPI backed in January 2020 was Moderna.)
But CEPI’s support for research on mRNA vaccines predates COVID-19—which is one of the reasons the approach was successful. The groundwork had been laid years before by investments from governments, pharmaceutical companies, and (more recently) CEPI. And the progress they’ve supported will continue to pay dividends long after the COVID pandemic ends. The mRNA platform is already being used to test new vaccines for TB and malaria diseases. Scientists are hard at work formulating next-generation vaccines that don’t require as many doses and don’t need to be kept frozen.
Altogether, CEPI has invested in 14 COVID vaccine candidates and it continues to work on variants of concern and develop next-generation vaccines that could protect against all coronaviruses. It is also focusing on six other diseases of epidemic potential.
But creating new vaccines isn’t enough. We also have to make sure that everyone who can benefit from vaccines has access to them, and that’s where the world has collectively failed in its response to COVID. While at least 9 billion doses were distributed in the past year, less than one percent went to people in low-income countries. It doesn’t make sense that so many people at lower risk of infection in wealthier countries got vaccinated before we reached the most vulnerable people, including the elderly, those with underlying medical conditions, and healthcare workers.
We need to do better the next time the world faces a pathogen that has the potential to spark a pandemic. (I’m currently writing a book about what the world needs to do to prevent the next pandemic, which will come out later this year.) I believe that the world can and should be ready to develop a new vaccine and make enough for everyone in the world within six months of detecting a potential pandemic—and CEPI will play a crucial role in achieving that. It is one example of how we need to be making investments now to support innovations that will prevent disasters in the future. For example, the organization is supporting efforts to increase manufacturing capacity and recently released a study that provides valuable insights into how we can improve the world’s production capabilities. This is the type of investment we need to make now to prevent disasters in the future.
And because CEPI is a global institution rather than a national one, it can focus on providing access for everyone, alongside other effective global institutions that have saved millions of lives like WHO, Gavi, and the Global Fund to Fight AIDS, TB and Malaria. These groups will help make sure that vaccines don’t just go to the highest bidders.
Imagine how different the last two years would’ve been if everyone in the world had had access to safe, effective COVID vaccines within six months. I know it’s hard to think about the next pandemic as the omicron variant surges around the world, but we have an opportunity to make sure the world never experiences this hardship again. Investing in organizations like CEPI is an important step that moves us closer to a world without pandemics.
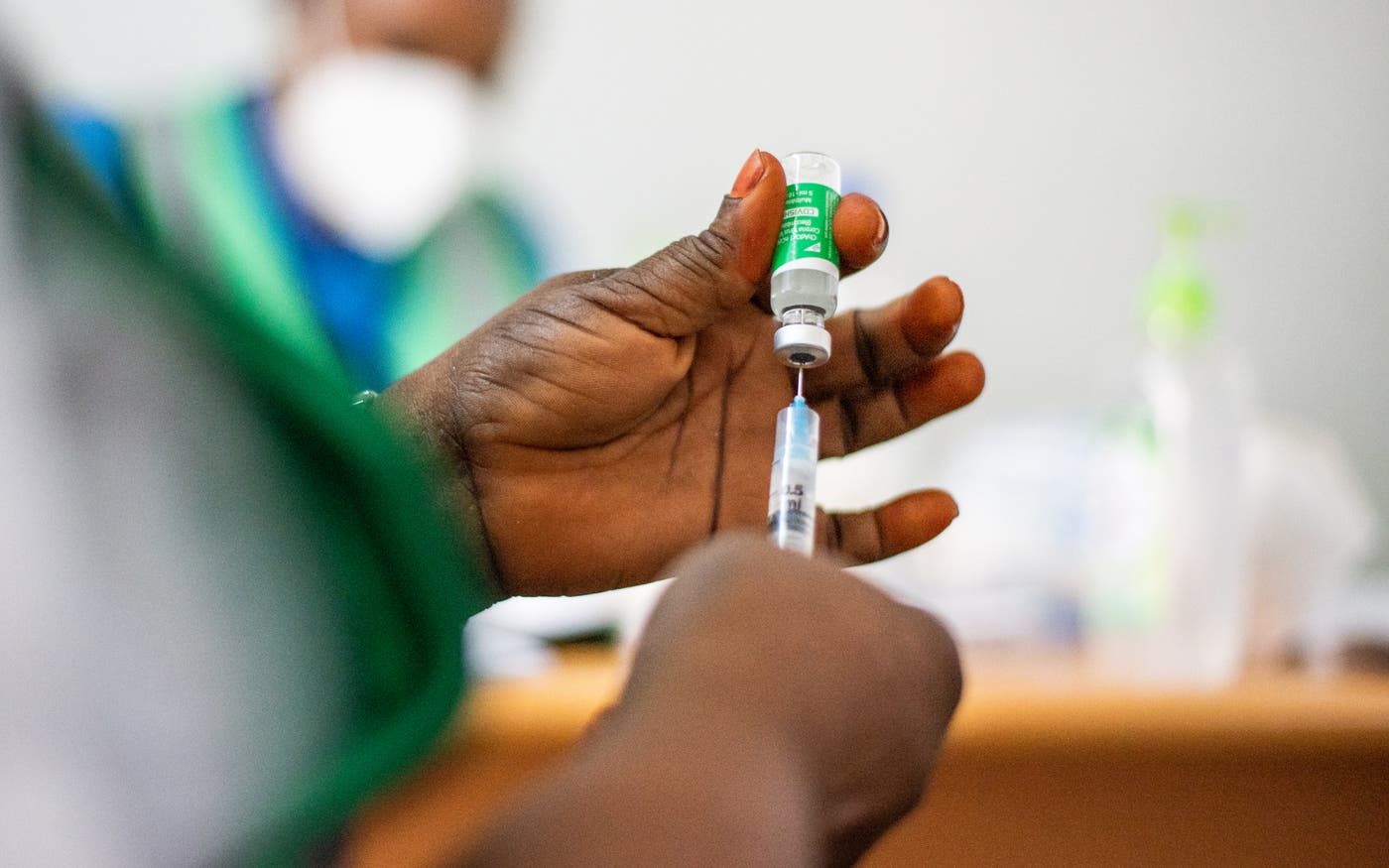
COVID coverage
Next time, we can close the vaccine gap much faster
How to use vaccines more fairly and effectively.

Today, 46 percent of the world’s population has received at least one dose of a COVID-19 vaccine. It’s hard to overstate what a remarkable achievement this is. Humanity has never made and distributed a vaccine for a disease faster than it did for COVID-19. It accomplished in 18 months something that used to take a decade or more.
But within this amazing success there is a startling disparity: Just over 2 percent of people in low-income countries have received any COVID-19 vaccines. And the gap will be harder to close as rich-world governments buy up extra doses to serve as booster shots.
People are right to be upset about the inequity here. Vaccines make COVID-19 a largely preventable disease—and a survivable one in all but the rarest cases—and it is heartbreaking to know that people are dying of a disease not because it can’t be stopped but because they live in a low-income country.
Sadly, this inequity is not new. It is not even the worst gap in global health. There were shocking disparities in health long before any of us had heard of COVID-19.
Every year, more than 5 million children die before their fifth birthday, mostly from infectious diseases, and almost entirely in low- and middle-income countries. A child in northern Nigeria is 20 times more likely to die before the age of 5 than a child in a rich country. That is simply unjust, and reducing this inequity has been the Gates Foundation’s top priority for more than 20 years.
If you step back and look at the trends, though, there is good news. Since 1960 the childhood death rate has been cut by more than 80 percent, thanks in large part to the invention and distribution of vaccines for children around the world.
The fact that routine childhood vaccines are reaching so many people is reason to believe COVID-19 vaccines can too. Providing them to everyone who needs them is one of three crucial steps in controlling this pandemic, along with containing the virus so it doesn’t come roaring back and coordinating the global response. At the same time, we can learn from the inequities that were so clear during this pandemic so we can do a better job of closing the gap during the next one. (Assuming there is a next pandemic. I think it is possible to prevent them altogether. But that’s a subject for another time.)
How could we achieve vaccine equity in a future pandemic? I see two ways.
1. Change how the world allocates doses.
What would the optimal allocation look like? It’s not simply a matter of proportional representation, where if your county has X percent of the world’s population, you get X percent of the vaccines. There are two different benefits to consider, and both are important.
One benefit is to the individual who’s immunized; they get protection from the virus. The more likely you are to get infected—and the more likely you are to become seriously ill or die if you do get infected—the more benefit you get from a vaccine. A COVID-19 patient in their seventies is 90 times more likely to die of the disease than a patient in their twenties. From a global perspective, it is neither fair nor wise to protect that young person before the old one.
Second, when an individual is vaccinated, society gets the benefit of lowering the risk that the person will spread the disease to others. This is the core of the argument in favor of vaccinating health workers and people who work in elderly care facilities, since even when a lockdown is in place, they can transmit the virus to people at high risk.
When a virus is spreading, we should maximize both benefits—saving lives and stopping transmission. This means that, when supplies are short, we should prioritize vaccinating people who both have a high risk of death and live in the places where the virus is spreading fastest.
Those will not necessarily be low-income countries. When COVID-19 vaccines first became available, many of the most severe epidemics were in rich- and middle-income countries.
The gravest inequity, even more than vaccinating rich people before poor ones, is vaccinating young people in rich countries before older people in middle-income countries with bad epidemics, such as South Africa and most of South America.
To their credit, rich countries have pledged to share more than a billion doses with poorer countries during COVID-19. But they haven’t yet delivered fully on those pledges, and even if they had, the gap would still be enormous.
Although sharing doses needs to be part of the solution, it will never be sufficient to solve the problem. For one thing, the number of doses won’t be high enough. And will future politicians always be willing to tell young voters they can’t be vaccinated because the doses are going to another country, at a time when schools are still closed and people—including a few young people—are still dying?
That’s why it’s so important to find ways to produce more doses in less time. The world should have the goal of being able to make and deliver enough vaccines for everyone on the planet within six months of detecting a potential pandemic. If we could do that, then the supply of doses would not be a limiting factor, and the way they were allocated would no longer be a matter of life and death.
2. Make more doses.
As limited as the supply of COVID-19 vaccines has been, the situation could have been even worse.
We are fortunate that mRNA vaccines work so well, since this is the first disease for which the mRNA technology has been used. If they hadn’t, we would have been far worse off.
It is also great that some vaccine companies entered into second-source deals, which allowed huge volumes of their vaccines to be manufactured by other firms. This was a crucial and remarkable step. (It’s as if Ford let Honda use its factories to build Accords.) Just one example: In less than two years, a single manufacturer, AstraZeneca, signed second source deals involving 25 factories in 15 countries.
You may have heard the argument that waiving intellectual property (or IP) restrictions would have made a difference. Unfortunately, that’s not true in this case. IP waivers and licensing are a complicated issue, so I want to take some time to untangle it.
There are cases in which IP licensing is a great way to make something cheaper and better. For example, in 2017, the Gates Foundation and a number of partners were involved in an agreement to make a new, more effective version of an HIV drug cocktail that would be more affordable for the world’s poorest countries.
In the deal, a pharmaceutical company gave the recipe for the key ingredient in this cocktail to firms that specialize in producing generic drugs. These firms were able to reduce the cost so much that today nearly 80 percent of people who get HIV treatment in low- or middle-income countries are receiving the improved cocktail.
Unfortunately, IP licensing doesn’t work as well with vaccines. Here’s why.
Many drugs are made using chemical processes that are well defined and measurable. If you mix the same ingredients in the right proportion and so on, you’ll get the same product every time, and you can check your work by looking at the chemical structure after the drug is made. Company A can give a recipe to company B, and company B will be able to make precisely the same drug consistently.
But many vaccines don’t work that way. Manufacturing them often involves living organisms—anything from bacteria to chicken eggs. Living things don’t necessarily act exactly the same way every time, which means that even if you follow the same process twice, you might not get the same product both times. Even an experienced vaccine maker might not be able to simply take another’s recipe and replicate it reliably.
This is why broadly waiving IP protections would not meaningfully increase the supply of vaccines. (In the case of COVID-19, though, a narrow waiver that applied to specific easily transferred technologies during the pandemic made sense.) Supply has been limited not because of IP rules, but because there aren’t enough factories capable of handling the more complicated process of making vaccines.
Licensing IP—or having the rights to it waived—only guarantees that company A can’t sue company B. Second-source deals are far superior because they involve sharing not only the recipe but also knowledge about how to use it, as well as personnel, data, and biological samples. It was a second-source deal with AstraZeneca—not an IP waiver—that allowed Serum Institute of India to produce 100 million doses at a very low cost and in record time.
So how can the world make more doses faster next time?
First, decision makers should get serious about expanding the world’s vaccine-making capacity. In particular, governments and industry should make sure there’s enough capacity to quickly make huge volumes of mRNA vaccines; now that we know the mRNA platform works, it will allow new vaccines to be developed faster than any other approach. And if companies that have second-source deals now maintain their relationships with each other, they won’t have to start from square one in the next outbreak.
Another step is to develop prototype vaccines against the diseases that are most likely to cause future outbreaks, and to develop universal vaccines for flu and coronaviruses, which would protect people against any form of the two pathogens. The NIH and Coalition for Epidemic Preparedness Innovations are doing excellent work on both, but even more research is needed.
One longer-term step is for more countries to build the capacity to develop, manufacture, and approve vaccines themselves.
Historically, the companies that invent new vaccines have been based in higher-income countries. Because it costs so much to develop a new product, they try to recoup their costs as quickly as possible by selling doses at the higher prices that rich countries can afford. They have no financial incentive to try to lower their costs (by optimizing the production process, for example) so that the price can be cheap enough for lower-income countries.
The pentavalent vaccine—which protects against five diseases—is a great example. It was invented in the early 2000s, but there was only one manufacturer, and at more than $3.50 per dose, it was far too expensive for low- or middle-income countries. Our foundation and other partners worked with two vaccine companies in India—Biological E Limited and Serum Institute of India—to develop a pentavalent vaccine that would be affordable everywhere. Today that vaccine costs about $1, and it is given to 80 million children a year. That’s a 16-fold increase since 2005.
We need more examples like this. Pentavalent took years to pull off. If there were more high-volume vaccine manufacturers whose primary goal was to produce low-cost vaccines, then affordable doses would be available much faster. Middle-income countries are a natural home for these companies, and some have set ambitious goals for themselves. For example, a group of African leaders has set a target of manufacturing 60 percent of the continent’s vaccines by 2040.
Helping middle-income countries build their vaccine-making capacity is something the Gates Foundation has been working on for two decades. We’ve helped bring 17 vaccines to market, and we’re supporting the African efforts to build theirs out by 2040.
What we’ve learned is that creating an entire vaccine-making ecosystem is a tough challenge. But the obstacles can be overcome.
One issue is the need for regulatory approvals. Vaccine factories are required to be approved by what’s known as a “gold-standard” regulator. India is the only developing country with a gold-standard regulator; factories in any other developing country have to be approved by their own government first, and then by the WHO. It’s time-consuming.
Regional agencies in Africa are working with the WHO and the European Union to create gold-standard regulation on the continent. Governments are also collaborating on regional standards for vaccines, so manufacturers don’t have to meet different safety and efficacy requirements in each country.
Another challenge: If vaccine manufacturers don’t have other products to make between outbreaks, they’ll go out of business. Unfortunately, making existing vaccines isn’t a viable option, at least right now, because the market is already saturated with existing vaccines, and it would be hard for new entrants to compete on price with established low-cost / high-volume companies.
But new products are coming that would be ideal products for them. As vaccines become available for diseases like malaria, tuberculosis, and HIV, they’ll create opportunities for producers in middle-income countries. In the meantime, countries can take on the fill and finish process—putting vaccines made elsewhere into vials and distributing them.
To anyone who has lost a loved one to COVID-19, or had to choose between paying the rent or buying food, it is no comfort to suggest that anything has gone well in this pandemic. But as my friend the late Hans Rosling used to say, “The world can be both bad and better.” The situation today is bad, and also better than it would have been if COVID-19 had come along ten years ago. If the world makes the right investments and decisions now, we can make things better next time. And maybe even make sure there is no next time at all.
This post originally appeared on CNN.com.

Pandemic plan
How to end the COVID crisis
Three steps to getting the virus under control.

This week global leaders are coming together at the UN General Assembly, which presents an opportunity to refocus energy and commitment on ending the crisis phase of this pandemic and to make sure we’re better prepared for the next one. In this piece I talk about how we can apply what we have learned since early 2020 and embrace a set of global actions that chart an equitable course out of the pandemic—vaccinate now, contain the disease, and coordinate the global response.
We’ve reached the 18th month of the COVID-19 pandemic, a somber milestone marked by yet another surge of cases and deaths fueled by the Delta variant. This global crisis has been a health, economic and moral disaster playing out in waves in every geography, sparing none. While the pandemic has been a shared experience, the experience has not been the same everywhere.
In the past year-and-a-half, we have witnessed scientific breakthroughs with multiple safe and effective vaccines developed in record time, incredible multilateral cooperation resulting in billions of dollars raised for the response, and heroic efforts by healthcare and frontline workers in communities worldwide. But at the same time, we have also seen widening gaps in equity that go against everything our foundation and its partners have worked for over the past 20 years. The advent of vaccines was an opportunity to bend the curve in the direction of a global recovery. It turned out that unequal distribution and a lack of funding and supply meant the recovery has been precarious and halting.
In last year’s Goalkeepers report, Melinda and I shared modeling that warned that globally deaths would be higher if doses went predominantly to high income countries. To date, less than 2% of people in low-income countries have received a dose of a COVID-19 vaccine, compared to more than 60% of people in the U.S. The pull of the inequity we’re seeing isn’t only on the here and now—the economic recovery of low-income countries that are slow to be vaccinated is stuck in the starting blocks. These countries can expect to experience between 2-4% GDP losses through 2025 (averaging 3% per year in sub-Saharan Africa).
After 18 months of surprises around every corner with variants fueling new waves of disease there’s a tendency to say one cannot predict what will happen next. To some extent that’s true—nature is wily, and the virus will continue to mutate if it can transmit unchecked. But it’s also defeatist and incorrect to suggest that the acute phase of the pandemic will spiral on from one variant to the next. Just as the virus can change, so can the world’s response to it. Whether the world can finally turn the corner, however, will be determined by what we do next and how it’s done.
Our path out of the pandemic has always required one thing—a commitment to equity. A willingness to see that what happens in lower-income countries affects high-income countries. There is no nationalistic solution to this global problem. We’ve seen countries try and fail in that pursuit as variants emerge and threaten progression from the acute phase of the pandemic. There are three things that can be done in the coming months that can bring about the end of the acute phase of the pandemic and set the world on a different timeline in preparation for the next. I hope that leaders meeting virtually this week at the COVID Summit commit to actions that meet these needs:
1. Vaccinate Now
Governments and the private sector must work together to build a more transparent system to accelerate the global supply of vaccines. While a shortage of supply was a major issue in the first half of the year, recently 41 million doses per day have been distributed globally. It’s progress, but there’s a long way to go. The WHO/Gavi-led COVAX AMC, Africa CDC-led African Vaccine Acquisition Task Team (AVATT) and other channels can move vaccines, but they need more doses, visibility to supply, and sufficient money to acquire and deliver them. This is quickly turning into a logistics and financing challenge, and we know how to solve those types of problems. A consolidated global dashboard that provides real-time vaccine production and availability data will enable countries and global institutions to collaborate on filling access gaps. While donations to COVAX were slow to arrive, current funding can support delivery to about 30% of the population in lower- and middle-income countries. It’s a good start, and funding for 70% coverage in the lowest income countries needs to be made available by mid-2022 along with enhanced delivery capacity at the country level.
2. Contain the Disease
In addition to getting vaccines out to close the global equity gap we also must contain outbreaks as they happen. This can help keep countries out of the cycle of lockdowns that has left schools and businesses in constant flux. To reduce the risk of variants jumping from border to border, the world must invest in readily available rapid testing, a system for sharing genetic sequences, and a mechanism to deliver expertise and commodities (like oxygen, PPE, and life-saving drugs) quickly where they are needed. We’ve seen this done successfully with diseases like polio and malaria—using data to inform actions that bring outbreaks under control. We need to have expert support and response materials like oxygen, PPE, and life-saving drugs ready to deploy in the event of major outbreaks. The private sector has a role to play, using its expertise in logistics to reduce lead times and fill supply gaps.
3. Coordinate the Global Response
The establishment of the Access to COVID-19 Tools Accelerator (ACT-A) in early 2020 was a milestone: governments, international organizations and the private sector came together in response to the crisis. We now need all governments to appoint a COVID-19 global lead, reporting to the head of state, and for these leads to regularly convene through 2022. With the support of independent monitoring this globally coordinated, time-limited task force can complement ACT-A and take us from aspiration to ending the pandemic through collective action and provide a model for the long-term coordination needed to prevent future pandemics.
For people involved in global health, what happened during the pandemic is disappointing, but not a surprise. The system whereby lower-income countries rely on the generosity of high-income country donors broke down when those donor countries were experiencing the same struggles. The next 18 months do not have to look like the past 18 months. But we cannot turn the page on this pandemic until we’ve addressed the fundamental inequity that stands in our way.
I’m optimistic about the potential of this moment. Health is not a zero-sum game—we can meet everyone’s needs through planning, investment, collaboration, and applying lessons learned. The cost of this pandemic has already been unacceptably high. Ending it cannot come at the cost of progress on other global health and development priorities. Reducing poverty, advancing gender equality, and finishing the job of eradicating polio are all possible through the same collective action that is needed to end this pandemic.
For those that want to go deeper, Gargee Ghosh who heads up the policy and advocacy division at the Gates Foundation has shared a white paper with more details on actions the world could take to end the COVID crisis.

Changes
5 things you should know about variants
The virus that causes COVID-19 is evolving, and it’s complicating our efforts to end the pandemic.

I’ve spent a lot of time over the last year meeting with colleagues at our foundation and around the world about ways to test for, treat, and prevent COVID-19. In recent months, the experts in those meetings are increasingly asking the same question: How will new variants impact our efforts to end the pandemic?
The world has come a long way in the fight against COVID-19, but new variants of the virus could threaten progress we’ve made over the past year. Here are five things you should know if you want to understand how variants are (and aren’t) complicating the pandemic.
1. If you’ve ever gotten a flu shot, you’ve already dealt with a virus variant.
Viruses evolve all the time. Unless you work on infectious diseases, the idea of a “variant” might seem new and scary—but there’s nothing particularly unusual about them. Influenza’s ability to mutate quickly (I’ll talk more about this in the next section) is why we get a new flu shot every year. We need to update the vaccine annually to keep up with constantly shifting flu virus strains.
To understand why the virus that causes COVID-19 is changing, you need to understand how it works (or spreads) in your body. The coronavirus—like all viruses—has only one goal: to replicate itself. Every time the virus invades your cells, it tricks the cell into following the instructions encoded in its RNA to make more copies of the virus.
When the cell is making a new virus, it has to copy those instructions. If you’ve ever had to take a typing class in school, you know how hard it is to retype something without making a mistake. The code for the virus that causes COVID-19 is around 30,000 letters long. That’s a lot of opportunities to mess up—which the coronavirus often does.
Most mistakes lead to a virus that either is functionally identical or can’t replicate. But every once in a while, there’s a change that makes it easier for the virus to infect people or evade the immune system. When that change starts to spread through a population, a new variant emerges.
2. We’re seeing the same mutations pop up again and again. That may be good news.
All viruses evolve, but not all viruses evolve at the same rate and in the same way. Some, like the flu, change rapidly. Others mutate slowly. Fortunately for us, SARS-CoV-2 is in the latter camp. It mutates about half as fast as the influenza virus.
I know it feels like new variants are popping up all the time right now. That’s because there is so much virus circulating around the world, giving it more opportunities to change. Once case numbers go down, I suspect we’ll see new variants emerge much less often.
Compared to influenza viruses—which are made up of eight genetic segments that can be rearranged in lots of different ways—the coronavirus is a much simpler virus. The most notable mutations we’ve seen so far have happened in the same spot: the spike protein that sticks out of the surface of the virus.
That spike protein is the key to COVID’s spread. Its shape is what enables the virus to grab onto human cells. If the spike protein changes just a little, it might bind with cells more effectively (which makes the virus more transmissible) or become harder for the immune system to target (which makes people more susceptible to it). But if it changes too much, the virus can no longer gain the entry that’s key to its lifecycle.
That limited capacity for change may explain why we keep seeing the same mutations appear in different places rather than lots of distinct variations. Both B.1.1.7 (which was originally detected in the UK) and B.1.351 (which was first found in South Africa) evolved independently, yet they share a number of the same mutations. There’s clearly something about these specific mutations that makes them more likely to succeed than other changes.
Some experts think we may have already seen the most concerning mutations that this virus is capable of. But COVID-19 has surprised us before, of course, and it could surprise us again.
3. The virus is changing, but the path to ending the pandemic remains the same.
For the last year, public health experts have been repeating some form of the same message: we need to contain COVID-19 as best we can until the vaccine is ready and available for everyone.
The good news is that many of the vaccines being used today appear to prevent severe disease, even from the new variants. This is a tribute to how effective the vaccines are in general. We still need a lot more data about how effective every vaccine is against the different variants, but many of the early numbers are reassuring (especially out of Israel, where many people are already vaccinated and the B.1.1.7 strain is dominant).
The big question now is whether we need to update the vaccines to target the variants. Regulators and drug companies are working on a modified vaccine that could be out in a couple months if it’s deemed necessary. Here in the United States—where the majority of people will likely be vaccinated by the end of the summer—some people may end up getting a booster shot that protects against additional strains.
For now, the key is to keep following best practices. The best way to prevent new variants from emerging is by stopping transmission of the virus altogether. If we remain vigilant about social distancing, wearing a mask, and getting vaccinated, we will bring the pandemic to an end much sooner.
4. Variants make it even more important that vaccines are made available everywhere.
COVID-19 anywhere is a threat to health everywhere. That’s true with the original virus, and it’s true when it comes to variants.
The more the virus that causes COVID-19 is out there in the world, the more opportunities it has to evolve—and to develop new ways of fighting our defenses against it. If we don’t get the vaccine out to every corner of the planet, we’ll have to live with the possibility that a much worse strain of the virus will emerge. We could even see a new variant emerge that evades existing vaccines altogether.
No one wants that to happen. The best way to make sure it doesn’t is by getting the vaccine out to everyone who needs it, no matter where they live. That’s why our foundation is working with governments, vaccine manufacturers, organizations like CEPI and Gavi, the Vaccine Alliance, and others to deliver COVID-19 vaccines to low-income countries through an initiative called COVAX.
COVAX recently announced that it’ll be able to deliver 300 million doses by mid-2021. That’s great news, but the world is going to need a lot more if we’re going to truly stamp out the threat of COVID-19. I hope rich world countries continue to support COVAX’s work, even as life starts to get back to normal in some parts of the world over the summer.
5. We can do better next time.
Virus variants are inevitable. If we ever find ourselves in a pandemic scenario again where a pathogen is spreading around the globe, we should expect to see it adapt to survive our attempts to stop it—just as we saw with COVID-19. I hope the difference next time is that we’re better prepared to spot these variants earlier.
The key will be genetic sequencing in combination with better disease surveillance. Right now, if you test positive for COVID-19, there’s a possibility that your test sample gets selected to be sequenced. This lets researchers see the exact 30,000 letter code that makes up the virus’ RNA instructions. That code gets uploaded to a database, where a computer compares the virus in your sample to all the other strains in circulation. . If you have a new strain that’s starting to pop up over and over in your area, scientists can compare the sequence data to transmission, death, and hospitalization rates to see if there’s need for concern.
Researchers need to take a systematic approach to catch variants early. Some experts think we need to sequence at least 5 percent of all test samples to get an accurate picture of how a pathogen is mutating—although sequencing a large number of samples alone isn’t enough. The UK has analyzed nearly 8 percent of its tests and linked that data with their surveillance capabilities, which helped them see that B.1.1.7 was spreading much faster and was more lethal. South Africa was able to quickly see how vaccines worked on B.1.351 by comparing results from clinical trials there to sequenced data.
The tools we’re putting in place to monitor variants in this pandemic will prove invaluable long after the worst of COVID-19 is behind us. Widespread sequencing should be part of any plan to prepare for the next pandemic. If you’re doing enough sequencing and comparing that data with other measures, you can see concerning variants when they first emerge. The earlier you identify a change, the more time you have to study it and, if needed, to tune vaccines and therapeutics to address any changes that have taken place.
There’s no doubt that variants complicate our efforts to bring an end to this pandemic. Even once the worst is behind us, we’ll need to remain vigilant. Fortunately, we know what we need to do to stop them from emerging. For now, the best thing you can do to protect yourself is to follow public health guidelines and get vaccinated as soon as you’re eligible.

Defeating dengue
This amazing breakthrough in fighting dengue is taking flight
Thanks to a tiny bacterium and mosquitoes, the world might defeat this terrible disease for good.

When it comes to killing humans, no other animal—not sharks, snakes, or crocodiles—is as deadly as the mosquito.
But in the fight against dengue fever, one kind of mosquito has been transformed into a surprisingly powerful ally to save and improve lives.
Dengue fever is a virus spread through bites by the Aedes aegypti mosquito. Nicknamed “breakbone fever” because of the severe pain it causes, dengue infects about 400 million people every year and kills more than 20,000. Warming temperatures due to climate change have expanded the geographic range of the mosquitoes, driving up the number of dengue cases in recent years.
Researchers with the World Mosquito Program, however, have been working on a breakthrough that just might defeat dengue for good.
This breakthrough relies on a tiny bacterium called Wolbachia and the Aedes aegypti mosquito.
Wolbachia is a common and harmless bacterium found in 60 percent of all insects, including fruit flies, bees, moths, and butterflies. But it’s not found in Aedes aegyptiWolbachia mosquitoes. More than a decade ago, researchers made a surprising discovery about . If Wolbachia Aedes aegyptiWolbachiais given to mosquitoes, it blocks them from transmitting the dengue virus. Researchers learned that spreads rapidly among mosquitoes when they mate, blocking the spread of dengue from one generation of mosquitoes to the next.
All this initial research was done in a lab setting. The next step was to test whether this approach would work in the real world. If Wolbachia mosquitoes were released into a community, would it lead to a reduction in dengue cases?
That’s the experiment the World Mosquito Program, a non-profit working to stop the spread of dengue and other mosquito-borne diseases, has been conducting in Yogyakarta, Indonesia. (Our foundation has been a proud funder of this research. In 2014, I visited Yogyakarta to see this work just as it was getting started. I even helped feed some of the Wolbachia-carrying mosquitoes!)
As part of a randomized controlled trial, researchers released Wolbachia mosquitoes in parts of Yogyakarta, which has some of the highest rates of dengue fever in the country.
Setting mosquitoes free in people’s neighborhoods is, of course, an unconventional solution to fight dengue. To earn public trust, researchers collaborated closely with the local community. They met with thousands of people in the city and addressed their questions and concerns about the program.
This public outreach effort took years. But it was worth it.
In June, the New England Journal of Medicine published the results of the trial, which show that the Wolbachia-carrying mosquitoes reduced the number of dengue cases by 77 percent and dengue hospitalizations by 86 percent.
Now, the World Mosquito Program is working to expand this effort in other parts of the world where dengue is a threat, including cities in Sri Lanka, Vietnam, Brazil, Colombia, Mexico, Australia, and Fiji.
This effort can be effective in preventing not only dengue, but also Zika, yellow fever, and other diseases transmitted by Aedes aegypti mosquitoes.
It’s hard to overstate the impact the World Mosquito Program may have on communities at risk of these diseases. Every dollar spent on this effort is expected to deliver $4 in economic benefits by saving billions of dollars in health care costs and preventing billions of hours of lost productivity due to illness.
I look forward to sharing more news about this incredible project in the years ahead.

Catastrophe averted
How to fight malaria during a pandemic
Despite COVID-19 disruptions, Africa’s malaria programs have kept up lifesaving malaria control and treatment efforts.

At the start of the pandemic, many people feared that not only would COVID-19 itself be a disaster, but the lockdowns and other prevention methods would have an awful ripple effect: disrupting the fight against malaria in a catastrophic way.
A modeling analysis from the World Health Organization, which I shared here last year, found that annual malaria deaths in sub-Saharan Africa could double, returning to death rates not seen in over 20 years.
A year later, I’m happy to be able to report that this worst-case scenario, at least for now, has been avoided. This is thanks to the leadership of African countries, which quickly adapted their malaria programs to meet the challenges of the pandemic. Practicing social distancing and other safety measures, malaria workers were able to carry out their duties, delivering long-lasting insecticide-treated bed nets, controlling mosquito populations with indoor spraying, and providing preventive treatment for pregnant women and children. In Nigeria, which still suffers from 60 million cases of malaria each year, health workers managed to even increase their delivery of malaria control, protecting millions of children in one of their largest campaigns to date.
At the same time, malaria resources have served double duty, tackling the mosquito-borne disease and helping to control the spread of COVID-19.
In Zambia, the scientists and equipment in the National Malaria Elimination Program’s genomic surveillance laboratory used to monitor malaria drug resistance quickly pivoted to find COVID-19 variants in the country. In Mozambique, an app created for health workers to provide real-time reporting of malaria cases and fevers has supplied critical data to the national COVID response.
Despite this progress, our work is not over. Malaria still kills more than 400,000 people each year. And pandemic lockdowns and movement restrictions have hampered some critical malaria activities, including access to diagnosis and treatment efforts in Africa.
Still, I’m optimistic that a world without malaria is within reach. And the COVID-19 pandemic reminds us why eradicating malaria is essential. Many of the building blocks we need to fight malaria and prevent the next pandemic are the same: accurate, real-time data; reliable supply chains to bring medicines and resources where they are needed most; and cross-country collaboration.
Investments in malaria programs help build stronger health systems that will not only save lives and bring an end to malaria, but also protect us from the next pandemic. And that creates a healthier, safer world for all.
Birthday Potty
Flush with innovation: 10 years of reinventing the toilet
A decade of innovation has yielded hundreds of new sanitation solutions that will prevent illness and death.

Ten years ago, our foundation challenged the world to reinvent the toilet.
To raise awareness of this challenge, I shared a stage with a jar of human feces.
Took a giant whiff of pit latrine odor.
Drank water made from fecal sludge.
And convinced Jimmy Fallon to drink it too.
All these stunts got some laughs, but my goal was to draw attention to a serious problem: poor sanitation.
About 3.6 billion people—nearly half of the world’s population—lack toilets or use unsafe sanitation.
Living without a toilet is more than an inconvenience. It’s dangerous. Unsafe sanitation means contaminated water, soil, and food. It causes illness and death.
According to the latest estimates, diarrhea and other sanitation-related diseases kill nearly 500,000 children under the age of five every year.
As the world gets more crowded, the human toll of unsafe sanitation will only increase. The United Nations estimates that between now and 2050, the world’s population will grow by two billion people. More than 90 percent of that growth will be concentrated in cities and in developing countries—places that are least likely to have good sanitation.
The COVID pandemic has also served as a powerful reminder of the urgent work households and cities must do to contain and treat deadly pathogens.
But this sanitation crisis can be solved.
In 2011, our foundation’s Reinvent the Toilet Challenge asked researchers if they could develop safe sanitation solutions that work without relying on sewage systems or running water. (Sewers and treatment plants have historically been the best way to safely process waste, but they are extremely expensive to build, maintain, and operate. They also rely on large amounts of water when many countries are suffering from water shortages.)
In the decade since we launched this challenge, the world has responded with the power of innovation. Scientists and engineers from across the globe developed hundreds of exciting ideas for how to design toilets that safely process human waste with little or no need for water or electricity. They created toilets that convert feces into valuable resources, including fertilizer, clean water, and electricity.
Other researchers invented a new system to process fecal sludge from pit latrines, septic tanks and sewers that turns human waste from entire communities into drinkable water and electricity. These machines, called omni-processors, can be used to support a fecal sludge treatment plant or complement a waste-water treatment plant. And they require a fraction of the energy, space and cost that a traditional sewer and wastewater treatment plant require.
In the next phase of the Reinvent the Toilet work, a team of researchers led by Dr. Shannon Yee at Georgia Institute of Technology is taking the best of these ideas to develop a low-cost reinvented toilet. It’s called the Generation 2 Reinvented Toilet. You can read more about the progress Shannon and his team have made here.
To be sure, there are still challenges ahead to bring these innovations to market so that they can transform the lives of the billions of people who need them.
But I’m optimistic about what can be accomplished in the next 10 years and beyond.
75 million toilets
India is winning its war on human waste
In India toilets are saving lives and boosting the economy.

Nearly three years ago, Indian Prime Minister Narendra Modi made one of the boldest comments on public health that I have ever heard from an elected official. It's still having a big impact today.
He made the comment during his first speech to the nation commemorating India's Independence Day. Modi said: “We are living in the 21st century. Has it ever pained us that our mothers and sisters have to defecate in the open?... The poor womenfolk of the village wait for the night; until darkness descends, they can`t go out to defecate. What bodily torture they must be feeling, how many diseases that act might engender. Can`t we make arrangements for toilets for the dignity of our mothers and sisters?”
I can’t think of another time when a national leader has broached such a sensitive topic so frankly and so publicly. Even better, Modi backed up his words with actions. Two months after that speech, he launched a campaign called Clean India (“Swachh Bharat” in Hindi), which now includes ending open defecation nationwide by 2019, installing 75 million toilets throughout the country—75 million!—and making sure that no untreated waste is dumped into the environment.
On my most recent visit to India, I made a video about this amazing undertaking:
If you’re wondering why the Prime Minister would put a spotlight on a subject that most of us would rather not even think about, take a look at the statistics. Of the 1.7 million people worldwide who die from unsafe water, sanitation, and hygiene each year, more than 600,000 are in India. A quarter of young girls there drop out of school because there’s no decent toilet available. When you factor in the deaths, sickness, and lost opportunity, poor sanitation costs India more than $106 billion a year.
In other words, solving this problem will save hundreds of thousands of lives every year, help girls stay in school, and boost the country’s economy. Improving sanitation is a big focus for our foundation, and we’re working closely with the Indian government in support of its goals.
There are two keys to achieving the targets of Clean India. One involves giving everyone access to a well-managed toilet, which means all the waste is treated (either on-site or in a treatment facility) to remove the pathogens that make people sick. It’s crucial to get the entire process right, from containing the waste in a toilet to collecting it, transporting it if necessary, and treating it. If one link in the chain fails, people still get sick.
Unfortunately, in many places, it’s not feasible to lay down sewer pipes or build treatment facilities. That’s why Indian researchers are testing a variety of new tools, including redesigned toilets that don’t require sewer systems and advanced ways to treat human waste.
So far, the progress is impressive. In 2014, when Clean India began, just 42 percent of Indians had access to proper sanitation. Today 63 percent do. And the government has a detailed plan to finish the job by October 2, 2019, the 150th anniversary of Mahatma Gandhi’s birth. Officials know which states are on track and which are lagging behind, thanks to a robust reporting system that includes photographing and geotagging each newly installed toilet.
But giving people access to toilets isn’t enough. You also have to persuade them to use the toilets. That’s the second key to Clean India, and in some ways it is even harder than the first. People can be reluctant to change old habits.
Clean India has ingenious ways of tackling that problem. In some communities, groups of children band together to call out people who are defecating in the open and encourage them to use public toilets instead. In a pilot project that will be expanded next year, the government worked with Google so users in 11 cities could search online for the nearest public toilets, get directions, and read reviews by other users. On streets throughout the country, billboards remind passers-by of the mission. Stars from Bollywood films and cricket teams speak out on TV and radio. Even India’s currency features the Swachh Bharat logo.
The hard work is paying off. Today more than 30 percent of Indian villages have been declared free of open defecation, up from 8 percent in 2015. (You can track the progress on this handy dashboard.)
What I love most about Clean India is that it identified a big problem, got everyone working on it, and is using measurement to show where things need to be done differently. As the old saying goes, What gets measured gets done. If you don’t set ambitious targets and chart your progress, you end up settling for business as usual—and in this case, business as usual would mean poor sanitation keeps killing more than half a million Indians every year.
By aiming high, the people of India are demanding change, and they are taking action to make it happen. It is a great example for other countries and an inspiration for all of us who believe everyone deserves a chance at a healthy, productive life.
A number one priority
Why the world deserves a better toilet
The toilet hasn’t really changed in over a century. It’s time for a redesign.

I just traveled halfway around the world to look at a toilet.
If you’re a long-time reader of TGN, this shouldn’t come as a surprise. There are few things I love talking about more. Sanitation is one of the most important issues we work on. I even drank water made from human feces a couple years ago.
That’s why I’m so excited to visit Beijing, China this week for the Reinvented Toilet Expo, where some of the most high-tech toilets in the world will be on display.
The toilets at the expo aren’t just fascinating gadgets—they have the potential to save millions of lives. More than half of the world’s population uses unsafe sanitation facilities. Even in places where people have access to toilets or pit latrines, their waste isn’t disposed of safely. The pathogens from the waste find their way into the local water supply and makes people sick.
The diseases caused by contaminated water kill more than 500,000 children under five every year. Those who survive are often too sick to go to school. It’s no exaggeration to say that poor sanitation holds back whole communities and entire nations.
If you live in a level 3 or 4 country, you can thank your sewer system for keeping you safe. Sewers have historically been the best way to make sure waste isn’t releasing harmful pathogens into the environment.
But what if you didn’t need a sewer to keep people safe? What if your toilet could dispose of waste all on its own?

Here in China, I get to see this and several other amazing new inventions that could deliver on the promise of sewer-less toilets.
Our foundation has invested a lot of money to develop a pipeline of next-generation sanitation solutions. In 2011, we launched the Reinvent the Toilet challenge. Many of the solutions created for that challenge are now ready to license. A remarkable cohort of engineers, scientists, companies, and universities around the world has done the hard work of getting a safe, off-grid sanitation market ready for take-off. My hope is that this week’s showcase moves their hard work one step closer to being used by real people around the world.
Each of these toilets seeks to solve the same problem, but they’ve all taken a different approach to get there. (The video above explains what specifically makes each toilet special.) Several run on solar power, so they can operate off-grid.

Others generate their own power, like the Cranfield nanomembrane toilet. Opening or closing its lid moves a screw that separates liquids from solids. A gasifier converts the solids into ash and heat that is used to operate the toilet.
A big theme for next-gen toilets is the ability to turn waste into something useful. The Ecosan extracts clean water, which is safe to use for hand-washing. The water created by Duke University’s neighborhood treatment system can be used to flush toilets or supplement fertilizer. The University of South Florida’s New Generator even collects methane gas for cooking or heating.
Another common feature involves burning waste to get rid of it (I apologize if you’re eating right now, but there’s no delicate way to describe this). The Janicki Firelight dries out urine and feces, turning them into sterile ash and water.
As you might have guessed, these toilets are a lot more complicated than your average toilet. Just look at the maintenance panel used to operate a public restroom:

The user experience for each is more or less the same as any other toilet, though. Most of the magic happens behind the scenes.
I know most people wouldn’t describe what toilets do as magical, but I think it’s true in this case. Think about it: the toilet hasn’t really changed in more than a century. If you could go back in time to the mid-1800s, you’d find flush toilets that work basically the same as the toilet in your home. And if you live somewhere with pit latrines, toilet design has stayed the same for even longer.
The toilets on display here in Beijing might one day replace a piece of technology that’s been with us for ages—and they could save millions of lives in the process.
Smells of Success
A perfume that smells like poop?
I took a whiff of the future of sanitation and it smells pretty good.

I recently traveled to Switzerland to take a giant whiff of pit latrine odor. What I inhaled was a strong kick to the nostrils, a potent combination of sewage stink, barnyard sweat, and bitter ammonia topped off with vomit (or was it parmesan cheese?). The stench was foul and made me wince.
Fortunately, I also got to smell something much fresher and more pleasing during my trip. I took the first sniffs of a future of odor-free toilets and better sanitation for all.
These olfactory revelations occurred during my tour of Firmenich, a family-owned fragrance and flavor company based in Geneva. The 120-year-old firm is known for crafting some of the world’s best-known fragrances and enhancing the flavors of beverages and foods. But it is also one of our foundation’s newest partners in the effort to improve sanitation in the world’s poorest countries.
I’ve written before about the world’s sanitation challenge. The numbers are staggering. One billion people have no access to toilets so they defecate out in the open. Three billion more have toilets, but their waste is dumped untreated, seeping into water and food supplies. About 800,000 children under age 5 die each year from diarrhea, pneumonia, and other common infections caused by unsafe water and sanitation. Beyond the tremendous human suffering, it’s a problem that slows economic development. In India alone, poor sanitation costs nearly $55 billion each year—more than 6 percent of GDP.
So how could a perfume company help?
Because smell matters.
Millions of new toilets are being built around the world to help end open defecation, including in India where a massive new toilet construction program is currently underway. This is great news. Unfortunately, many of these new toilets, especially the pit latrines, don’t get used because they smell bad and people continue to relieve themselves in the open where the air is fresher. This is a worrying trend that threatens to undermine the progress that’s been achieved in global sanitation.
A few years ago our foundation organized a “smell summit” to discuss ways to address this problem. Representatives from Firmenich were among the attendees and they thought they might be able to help.
With more than a century of experience creating perfumes and flavors, Firmenich has developed sophisticated approaches to analyzing odors and breaking them down to their chemical components. They started their work with the foundation’s sanitation team by asking a basic question: why do toilets smell so bad?
The answer may seem obvious. But toilet odors are actually quite complex. They consist of more than 200 different chemical compounds arising from feces and urine that change over time and vary depending on the health and diet. Firmenich researchers wanted to know which ones were responsible for the terrible smell.
They isolated four chemical culprits: indole, p-cresol, dimethyl trisulfide, and butyric acid. Then, they asked their scientists to try to recreate the odor using synthetic compounds. In other words, they made a fragrance that smelled like fecal matter and stale urine. A poop perfume!
To make sure they got the offensive odor just right, Firmenich asked people in Switzerland, India, and Africa which fragrances most closely mimicked a stinky toilet. The result of their efforts? The fragrance I breathed in during my visit. I put my nose up to a glass sniffing tube in Firmenich’s research facility and I was hit by a blast of foul-smelling odors. As I described (perhaps too vividly) above, it smelled as bad as the worst toilets I’ve ever visited.
With the poop perfume in hand, Firmenich’s researchers could use it to experiment with various other fragrances, exploring how to effectively mask the offensive odors.
In the long history of battling disagreeable odors, from sweaty armpits to wet dogs, the world has largely relied on one solution to the problem. We use pleasant fragrances to cover over the malodors we want to hide—the olfactory equivalent of sweeping dirt under a rug.
Firmenich wanted to try a different, more innovative approach to this age-old challenge. They wanted to attack the problem on a molecular level at the connection between our noses and our brains.
Our noses have 350 olfactory receptors, each one awakening us to new sensations from the smell of a rose to stinky feet. Just a handful of them allow us to smell repulsive odors. Firmenich researchers used this knowledge to develop fragrances that block certain receptors in our noses, making us unable to register certain malodors.
The approach is similar to noise-canceling headphones which many people use to block out jet engine noise on flights. Electronics in the headsets create a sound wave that is 180 degrees out of phase with the ambient noise that needs to be blocked. This wave cancels unpleasant sounds and allows you to enjoy peace and quiet. Likewise, the ingredients in the fragrances developed by Firmenich inhibit the activation of the olfactory receptors sensitive to malodors. By blocking the receptors, our brains do not perceive the bad smells.
I had an opportunity to experience the odor-blocking fragrances in action. I was invited to push my nose into a glass sniffing tube and breathe in a mixture of the poop perfume I had just experienced and one of the new odor-blocking fragrances. It smelled pretty good. There was no evidence of repulsive odor I had experienced earlier. Instead of stinky sewage, sweat, and ripe cheese, I sniffed a pleasant floral scent.
The question now is whether this technology is good enough to make a difference in communities with poor sanitation. That’s why Firmenich is launching pilot projects in communities across India and Africa to understand whether the fragrances will make toilets and pit latrines more inviting for users. They also need to determine if it’s better to distribute the fragrance as a spray, a powder, or something else. The ultimate goal is to make the product affordable and easy-to-use.
I continue to be amazed by the innovation that’s underway in the field of sanitation. Until recently, sanitation was a taboo subject. It didn’t attract many resources or interest from researchers. Now, dozens of researchers, technologists, and decision-makers from both the private and public sectors are partners in the effort. Together, we are working to identify and develop solutions that people value and that will improve the health and dignity of urban slums and other densely populated communities where the need for better sanitation is greatest.
I was excited to see Firmenich contributing its expertise and creativity to solving this challenge and look forward to updates on the progress they’re making.
It had been a busy day in Geneva for my nose and my 350 olfactory receptors. But one scent continues to linger. It’s the smell of success—the kind that happens when people put their talents together to make the world a better place.
War on Pathogens
Update: what ever happened to the machine that turns feces into water?
An update on the machine that turns feces into water.

Earlier this year, I shared a video where I drank water made from feces. (My review: It was delicious.) Today the machine that produced the water, the Janicki Omni Processor—or JOP—is in Dakar, Senegal, as part of a pilot project that could ultimately save lives and reduce disease in poor countries. Here’s an update on where things stand:
You may recall that the JOP takes human waste and turns it into drinking water, electricity, and ash. (It is actually one of several Omni Processors being developed that treat human waste and produce something of value.) It’s tempting to focus on the drinking water, for obvious reasons. But the goal is not to provide water. The goal is to dramatically improve sanitation for all the cities in poor countries.
Today at least 2 billion people use latrines that aren’t properly drained, and diseases caused by poor sanitation kill some 700,000 children every year. Unfortunately, rich-world solutions aren’t feasible in poor countries—they require too much expensive infrastructure. (We put together this slideshow so you can see how the system works in Dakar today and how the JOP fits in.) The idea behind every Omni Processor design is to solve this problem by making sanitation affordable for the poor.
We think we have solved the big engineering challenges, thanks to ingenious design work by our partners Janicki Bioenergy. The technology just keeps getting better: The next version of the machine will burn most types of garbage in addition to human waste, and it will be easier to maintain. We also think we have a good business plan. Janicki is discussing the sale of the first JOP to a Senegalese company, and they’re talking to potential buyers in wealthier countries too.
But business plans and brilliant engineering are not enough. The machine has to be tested—and unlike a computer program, sanitation machines can’t be tested from a desk in Seattle. The real world introduces lots of variables. For example, you have to find the right personnel to run the machine. You have to work with local and national governments and gauge the public’s reaction.
So it is great that we are now on the learning curve with a unit in the field. So far, the results on all fronts have been promising. The JOP is working as predicted. The partners in Dakar, especially the national sanitation utility, have been fantastic—you can see in the video how energetic and optimistic they are. At every step, we’re learning and will incorporate what we find in future designs and operating plans. For example, the team is still looking at ways to make the JOP cheaper and smaller.
Much of the technology involved in the JOP has been around for years. So why hasn’t anyone built one before now? Because the people who understood the technology weren’t getting sick or dying from contaminated water, and they didn’t know anyone who was. Nor was it clear how they could make a profit by working on the problem. It was a classic market failure.
Now we have a business plan, an impassioned team of engineers, great in-country partners, and a pilot project in motion. I think we have a real shot at solving the sanitation problem. This is a great example of what can happen when we get bright people focused on the world’s biggest problems.
Why is better sanitation so important
Sanitizing in Senegal
Photos that show why better sanitation is so important.

The next time you flush a toilet, consider this: 1 billion people defecate in the open. Another 4 billion use rudimentary toilets and their waste is never treated.
I have visited communities where this is a sobering fact of life. The smell can be overwhelming, but even worse, the sewage seeps into the water supply, spreading disease. Poor sanitation is linked to the deaths of some 700,000 children every year.
Our foundation is funding the Omni Processor, a machine that we hope will make sanitation affordable.
Dr. Mbaye Mbeguere is one of the Senegalese officials leading this pilot project. You can see the Janicki OP behind him. Dr. Mbeguere and his colleagues hope Omni Processors will change the face of sanitation in cities around the world. I am optimistic that they are right.
From Poop to Potable
This ingenious machine turns feces into drinking water
This machine turns feces into water and electricity—and may save lives.

I watched the piles of feces go up the conveyer belt and drop into a large bin. They made their way through the machine, getting boiled and treated. A few minutes later I took a long taste of the end result: a glass of delicious drinking water.
The occasion was a tour of a facility that burns human waste and produces water and electricity (plus a little ash). I have visited lots of similar sites, like power plants and paper mills, so when I heard about this one—it’s part of the Gates Foundation’s effort to improve sanitation in poor countries—I was eager to check it out.
The water tasted as good as any I’ve had out of a bottle. And having studied the engineering behind it, I would happily drink it every day. It’s that safe.
Here’s a short video from my visit in November, which explains how it all works:
Why would anyone want to turn waste into drinking water and electricity?
Because a shocking number of people, at least 2 billion, use latrines that aren’t properly drained. Others simply defecate out in the open. The waste contaminates drinking water for millions of people, with horrific consequences: Diseases caused by poor sanitation kill some 700,000 children every year, and they prevent many more from fully developing mentally and physically.
If we can develop safe, affordable ways to get rid of human waste, we can prevent many of those deaths and help more children grow up healthy.
Western toilets aren’t the answer, because they require a massive infrastructure of sewer lines and treatment plants that just isn’t feasible in many poor countries. So a few years ago our foundation put out a call for new solution.
One idea is to reinvent the toilet, which I’ve written about before.
Another idea—and the goal of the project I toured—is to reinvent the sewage treatment plant. The project is called the Omniprocessor, and it was designed and built by Janicki Bioenergy, an engineering firm based north of Seattle. I recently went to Janicki’s headquarters to check out an Omniprocessor before the start of a pilot project in Senegal.
The Omniprocessor is a safe repository for human waste. Today, in many places without modern sewage systems, truckers take the waste from latrines and dump it into the nearest river or the ocean—or at a treatment facility that doesn’t actually treat the sewage. Either way, it often ends up in the water supply. If they took it to the Omniprocessor instead, it would be burned safely. The machine runs at such a high temperature (1000 degrees Celsius) that there’s no nasty smell; in fact it meets all the emissions standards set by the U.S. government.
Before we even started the tour, I had a question: Don’t modern sewage plants already incinerate waste? I learned that some just turn the waste into solids that are stored in the desert. Others burn it using diesel or some other fuel that they buy. That means they use a lot of energy, which makes them impractical in most poor countries.
The Omniprocessor solves that problem. Through the ingenious use of a steam engine, it produces more than enough energy to burn the next batch of waste. In other words, it powers itself, with electricity to spare. The next-generation processor, more advanced than the one I saw, will handle waste from 100,000 people, producing up to 86,000 liters of potable water a day and a net 250 kw of electricity.
If we get it right, it will be a good example of how philanthropy can provide seed money that draws bright people to work on big problems, eventually creating a self-supporting industry. Our foundation is funding Janicki to do the development. It’s really amazing to see how they’ve embraced the work; founder Peter Janicki and his family have traveled to Africa and India multiple times so they can see the scope of the problem. Our goal is to make the processors cheap enough that entrepreneurs in low- and middle-income countries will want to invest in them and then start profitable waste-treatment businesses.
We still have a lot to learn before we get to that point. The next step is the pilot project; later this year, Janicki will set up an Omniprocessor in Dakar, Senegal, where they’ll study everything from how you connect with the local community (the team is already working with leaders there) to how you pick the most convenient location. They will also test one of the coolest things I saw on my tour: a system of sensors and webcams that will let Janicki’s engineers control the processor remotely and communicate with the team in Dakar so they can diagnose any problems that come up.
The history of philanthropy is littered with well-intentioned inventions that never deliver on their promise. Hopefully, these early steps will help us make sure the Omniprocessor doesn’t join the list. If things go well in Senegal, we’ll start looking for partners in the developing world. For example I think it could be a great fit in India, where there are lots of entrepreneurs who could own and operate the processors, as well as companies with the skill to manufacture many of the parts.
It might be many years before the processor is being used widely. But I was really impressed with Janicki’s engineering. And I’m excited about the business model. The processor wouldn’t just keep human waste out of the drinking water; it would turn waste into a commodity with real value in the marketplace. It’s the ultimate example of that old expression: one man’s trash is another man’s treasure.
Polio
Iron will
I can’t think of a more important moment than right now in the fight against polio.

Most people today probably don’t know what this is.
And that’s a good thing because it shows how much progress the world has made against polio, a terrible and now largely forgotten disease.
This metal tank is an iron lung, a mechanical respirator that saved the lives of thousands of polio victims.
Polio attacks the body’s nervous system, crippling patients. In the worst cases, the disease paralyzes their respiratory muscles and makes it difficult for them to breathe, sometimes resulting in death.
Using changes in air pressure, the iron lung pulls air in and out of a patient’s lungs, allowing them to breathe and stay alive.
During the height of the polio epidemic in the U.S. in the 1940s and 1950s, rows of iron lungs filled hospital wards to treat thousands of polio patients, most of them children.
Polio
Meeting the Musahar
A trip to a remote corner of India taught me a powerful lesson about what it will take to wipe out polio.

Whenever someone asks me why I believe it’s possible to eradicate polio, I tell them about my 2010 trip to India to visit one of the country’s lowest castes—the Musahar.
Today, India is polio free. But less than a decade ago, more than half the world’s cases of polio could be found in India. At the time, many health experts said that India would be the last place on Earth to stop polio because its high birth rate, poor sanitation, and population density allowed the disease to flourish.
So how did they wipe out the disease?
The answer can be found in the remote marshlands of the Kosi River in the Indian state of Bihar. The region is home to one of the poorest, most underserved castes in India, the Musahar. In 2010, vaccinating the Musahar and other people living in remote, high-risk areas was one of the biggest obstacles India faced in its long campaign to end the paralyzing disease. Thousands of children were being missed during the national immunization drives, allowing the disease to continue to spread.
In response, the Indian government launched an all-out effort to reach every child, employing a new communication campaign to mobilize support for polio immunization and better maps to ensure that no family was missed. They deployed more than 2 million vaccinators who covered every speck of the country, including the Musahar village I visited, which was often inaccessible because of flooding from the Kosi River. (One of the most inspiring photographs of that time was an image of polio workers wading waste deep in water to reach remote villages with the polio vaccine.)
By 2014, India achieved its goal of being polio free, proving that the paralyzing disease could be defeated in the most complicated circumstances. With new ties to even the remotest communities, health workers are providing children with much more than the polio vaccine. They continue to work with local communities to improve the delivery of other critical health services, including maternal and newborn care, as well as vaccinations for measles and other preventable diseases.
India’s experience continues to be an inspiration for the world’s final push to wipe out polio in the three countries where it endures: Afghanistan, Pakistan, and Nigeria. Based on the latest figures, in 2017, there were just 21 identified cases of wild poliovirus in the world—the lowest number ever—down from 350,000 cases per year when the global polio eradication effort launched in 1988.
That’s an incredible achievement. But now is no time for complacency. If polio is a threat anywhere in the world, it is a threat to us all. That’s why it’s more important than ever for the world to continue to support the millions of vaccinators who are working tirelessly to finish the job. Their dream, as is mine, is to see the day that polio is defeated.

Inspired by a farmer
These married scientists are leading the way on HIV
The Abdool Karims revolutionized the fight against AIDS. Now they’re helping the world tackle COVID-19 too.

Quarraisha and Salim Abdool Karim are two of the most respected HIV/AIDS researchers in the world. This year, the wife-and-husband team has also helped shape the world’s response to COVID-19. But it was a more humble setting that sparked their careers in epidemiology more than 30 years ago.
They had met in medical school in their native South Africa before moving to New York City for graduate school. In 1988, shortly after they were married, they took a trip to Mexico, where they met up in a tiny village in the Sierra Madre mountains with a friend, a physician who had written a seminal textbook on health care in remote rural settings.
Outside the village’s health clinic, they saw a man pedaling a bicycle that was mounted on a stand and connected to a power cable. It turned out that a local farmer also doubled as the village’s dentist—a pretty good one, apparently—and volunteers would pedal the bike to power his drill.
“We watched how this community took their destiny in their own hands,” says Salim, “and they had the most amazing dental care from this bicycle powering a drill. It imprinted on us how people can really change their own world.”
It was a powerful lesson about the need for scientists to understand and collaborate with the people they’re trying to help. The experience in that village would shape the rest of their careers, especially when they created a research center in South Africa designed to address two of the biggest problems in HIV/AIDS in Africa.
By the 1990s, the disease was devastating the Abdool Karims’ home country—and still is today. One out of every five people in the world with HIV lives in South Africa. The couple saw two issues that were rarely on the agenda of other HIV experts. One was that young women were bearing a disproportionate burden in the epidemic, and that there was no way to control the epidemic if their needs weren’t addressed. The other was that people living with HIV are at a high risk of contracting and dying from tuberculosis—a link that’s now known as HIV-TB coinfection.
“These were very much our problems in Africa that few others were working on,” says Quarraisha, “and if we waited for solutions from elsewhere, it wasn’t going to come. We had to take the lead.”
In 2001, they brought together a group of researchers they felt could make a bigger impact on HIV and named the group CAPRISA (for the Center for the AIDS Program of Research in South Africa). Today CAPRISA runs three clinics where they provide antiretrovirals to people living with HIV and study new approaches to treating and preventing the disease. It is regarded as one of the world’s most influential AIDS research programs.
CAPRISA is probably best known for a landmark study published in 2010 proving for the first time that a microbicide—a gel that a woman could use before and after sex—can offer some protection from the virus. Scientists had been trying to make effective microbicides for nearly two decades, but the Abdool Karims’ formulation—one that used tenofovir, a drug normally given to people who already had HIV—was the first to offer any protection. Although the field has now moved on from microbicides and is focused on a more effective daily pill instead, the concept is still based on CAPRISA’s microbicide findings.
CAPRISA is as admired for the way it works as for its results. Inspired by the farmer-dentist they met in Mexico, Salim and Quarraisha make it a priority to empower the people they’re trying to help. They work closely with community leaders to make sure their research efforts are informed by realities on the ground and embraced by their neighbors. Here’s the story of one remarkable CAPRISA staff member, Gethwana Mahlase, and the way she represents the program in her community of Vulindlela.
Over the next few years, Quarraisha and Salim hope to build on their study of tenofovir as an HIV preventative. Right now, the best option is a pill you have to take every day, a regimen that can be hard to keep up. So CAPRISA is working on a form of the drug that could protect a woman for as long as a year at a time.
They’re also working on a fascinating approach called “broadly neutralizing antibodies,” which dates back several years. In 2012, they discovered that an HIV-positive woman in one of CAPRISA’s studies had a trait that was, as far as they knew, unique. The antibodies made by her immune system could attack not only the strain of HIV that she had, but also—this was the impressive part—80 percent of the other known strains of HIV from around the world. If they could isolate the cells that made these antibodies, reproduce them, and use them to create antibodies for other people, it would be a game changer.
After years of painstaking work with a number of partners, they were able to create the broadly neutralizing antibodies in a lab and test them in monkeys, with very positive results. Now the antibodies are being studied in humans for safety and, eventually, efficacy. If this approach works, you would need to get an injection just twice a year in order to get protection—a dosage that is far more practical than a daily pill. Success would also point the way toward the ultimate goal of an HIV vaccine.
Unfortunately, much of the Abdool Karims’ attention has been elsewhere this year. Drawing on their experiences from HIV and TB, they are helping guide the COVID-19 response in South Africa and around the world. It is a shame that they haven’t been able to focus on HIV/AIDS, but on the other hand, it is a reminder of how fighting old diseases like HIV helps the world prepare for new ones like COVID-19. Investing long-term in programs like CAPRISA—or work on polio or malaria—not only prevents deaths and disability from specific diseases, it also strengthens the overall field of global health. So when a pandemic comes along, we have a network of experts like Quarraisha and Salim ready to pitch in.
What strikes me about this couple is how upbeat they are, even in the face of devastating diseases like the coronavirus and HIV. Their motto at CAPRISA is, “Each day that you come to work, you should be looking for how today is going to be better than yesterday.” That is a lesson we can all take to heart.
Heroes
Strength in numbers
The story of this amazing woman living with HIV in Mozambique fuels my optimism about our world.

Last year, at an event in New York, I learned about an impressive woman whose story I want to share with you. Her name is Cacilda Fumo, she lives in Mozambique, and every year she helps save hundreds of lives—by reminding them they are not alone.
Mozambique has one of the highest HIV infection rates in the world. More than 1.6 million people—10 percent of the adult population—are living with HIV.
Cacilda was diagnosed with HIV in 2002. “When I first learned about it, I thought I would die,” she recalls. “I used to wake up early morning and check if I am alive or not.”
But then she started meeting other people living with HIV, and as their numbers grew so did her strength and her belief she would live. Cacilda was one of the first in Maputo to be open about her status. She started wearing a t-shirt emblazoned with a logo that reads: “HIV POSITIVE.”
At times, people rejected her because of her status. Many more in her community, however, admired her for her courage, helping her create an even larger circle of friends and supporters. They met every week, praying together, cooking together, and sharing their stories. Eventually, the group had about one hundred people, many of them receiving life-saving anti-retroviral treatment. Cacilda emerged as their leader.
About the same time, Mozambique’s Ministry of Health was struggling to improve the delivery of anti-retroviral treatment. While the program was successful in putting thousands of patients on treatment for the first time, medical staff were overburdened with caseloads. People on HIV treatment often walked miles to reach their clinic and waited in long lines to get care. Every year, about 30 percent of HIV patients dropped off their life-saving treatment.
Working with Doctors Without Borders, the government of Mozambique decided to try a new approach to simplify care to help keep more people on treatment. They started organizing small peer support groups for people on HIV treatment. The idea was simple. Make treatment easier by putting more control into the hands of the patients. A representative from each patient group could pick up all the drugs for the group each month, saving the rest of the group the hassle of going to the clinic. Members of the groups, known as Community antiretroviral therapy (ART) Groups or CAGs, would also support one another to ensure they were all staying on their treatment.
When the program reached Maputo, Cacilda was ready to join. She helped organize dozens of support groups from her network. Then she went one step further. She kept track of the groups, checking whether members were attending their meetings and taking their treatment. If someone fell off treatment, she took upon herself to locate them and find out what was wrong.
“We help people feel strong knowing they are not alone,” she says.
Some patients who stop treatment are addicted to alcohol and forget to take their treatment, she says. Some don’t understand how the treatment works and the stop taking their medication as soon as they feel better. Others get busy with their jobs and drift away.
Whatever the reason, Cacilda warns them of the dangers of stopping treatment and encourages them to restart. Her efforts to bring back residents of Maputo to treatment has become nearly full-time work. Most days residents of Maputo see Cacilda traveling on foot—which is remarkable because due to a childhood injury she uses crutches—through the dirty alleyways and crowded markets in search of people who have stopped treatment. She doesn’t give up until she finds them.
Cacilda’s persistence pays off—in lives saved. Cacilda estimates that she tracks down about 500 people every year and encourages them to resume their treatment.
That’s a remarkable achievement—one that proves how much difference one life can make in the world.
World AIDS Day
The fight against AIDS is filled with heroes. Learn how you can be one too.
Thanks to many heroes, the world has made amazing progress against HIV/AIDS.

On December 1st, the global community will observe World AIDS Day. This year I would like to mark it by highlighting the work of two heroes who are making a difference in the fight against this deadly disease.
Chief Jonathan Eshiloni Mumena is chief of the Kaonde people, who live along Zambia’s border with the Democratic Republic of Congo. Risking his position as his people’s leader, Chief Mumena challenged long-held traditions to encourage Kaonde men to embrace voluntary medical male circumcision as a strategy to prevent HIV transmission. (Male circumcision can reduce a man’s risk of acquiring or transmitting HIV by up to 60 percent.) I had the privilege of meeting Chief Mumena in 2012. His story is an inspiring tale of courageous leadership and deep compassion for his people.
Guided by her belief that health care is a basic human right, Dr. Krisana Kraisintu, a pharmacist from Thailand, has worked tirelessly to make medicines affordable to even the poorest in the world. Her development of generic versions of the lifesaving HIV drugs dramatically reduced treatment costs, saving and improving countless lives. She has also dedicated her pharmaceutical skills to reduce treatment costs for malaria and other diseases.
Of course, Chief Mumena and Dr. Kraisintu are just two of the countless individuals—doctors, policymakers, researchers, activists, and political leaders—whose contributions have helped turn the tide against the disease. Today, 19.5 million people receive lifesaving antiretroviral therapy, giving them the opportunity to live full, productive lives. Improved access to treatment has also meant that millions of babies are now born HIV-free.
Much of this progress has been made possible by the world’s enormous investments in efforts to defeat the epidemic, including the Global Fund to Fight AIDS, Tuberculosis and Malaria, and the U.S. HIV/AIDS program known as PEPFAR, President’s Emergency Plan for AIDS Relief.
Still, many challenges lie ahead in the fight against the AIDS epidemic.
Funding for HIV control has been flat and there’s talk about cuts as the world turns to other priorities. Cuts in funding for HIV/AIDS would lead to sharp increases in deaths and new infections, reversing the gains that have been made the last decade. That’s why it’s more important than ever for the world to reaffirm its commitment to this fight. We need more AIDS heroes—from health care workers and advocates to global leaders. Together, we can bring an end to this public health threat.
If you want to be a hero this World AIDS Day, support the (RED) Shopathon. Our foundation is matching every dollar raised—up to $15 million—to fight HIV/AIDS in Africa.

Exemplars
We’re finally learning why countries excel at saving lives
A new program is spreading the word about the most successful approaches to health.

Ever since I was a teenager, I’ve tackled every big new problem the same way: by starting off with two questions. I used this technique at Microsoft, and I still use it today. I ask these questions literally every week about COVID-19.
Here they are: Who has dealt with this problem well? And what can we learn from them?
They seem like obvious questions, but sometimes it's surprisingly hard to find the answers—especially when it comes to global health. There are low- and middle-income countries that have made huge leaps in, for example, delivering vaccines or ending malnutrition. But anyone who wants to identify those countries, find out how they did it, and apply the lessons in their own country would have their work cut out for them.
In sports, every coach is able to study the most successful teams and figure out what they’re doing well. There’s no reason that things should be any different when the goal is preventing childhood deaths instead of scoring touchdowns.
That’s why I was eager to be part of a global effort to fill the gap. Over the past three years, health experts and organizations from countries at every income level (including the Gates Foundation) have come together to find out who has made the most progress on certain health problems, identify what made them so successful, and help others put these lessons into action.
The result of all this effort—the Exemplars in Global Health program—launched earlier this year. If you want to know which countries have made the most progress with limited resources, Exemplars is a great place to start.
For now, Exemplars focuses on five areas: under-five mortality; vaccine delivery; the role of community health workers; epidemic preparedness and response; and childhood stunting (the reduction in physical and mental development caused by poor nutrition). The team will be adding other areas, including newborn and maternal mortality, family planning, maternal anemia, and primary health care systems.
The Exemplars team has scoured the world for the best performers and worked with experts in those countries to find out what worked so well. For example, they identified seven countries that have excelled at reducing the number of children who die before their fifth birthday: Bangladesh, Cambodia, Ethiopia, Nepal, Peru, Rwanda, and Senegal. The Exemplars website has a profile of each country, detailing insights from its work that other countries could learn from.
Bangladesh—whose childhood mortality rate dropped 56 percent between 2000 and 2015—used data, research, and testing especially well, and empowered women to make decisions about their children’s health. Peru, which achieved roughly the same decline as Bangladesh, conducted local studies to identify interventions that might suit specific communities. All seven countries built up strong community health systems and made specific efforts to close the equity gap by reaching the poorest people.
Of course, not all lessons can be applied in the same way everywhere. What works in one country may not work exactly the same way in another. And it is not always obvious how to implement big changes in national health systems, which are very complex and require a lot of coordination among the government, the private sector, and non-profits.
Recognizing these challenges, the Exemplars program is much more than a website. There is also a community of global and in-country experts ready to help countries make the case for investing in the most effective programs and figure out how to adapt the lessons to their particular needs. We’re not interested in simply getting the information out there—we want to help drive change.
Our hope is to connect with decisionmakers: people who work in the governments of low- and middle-income countries, at development agencies like America’s USAID and the World Bank, and at organizations that implement health programs. Exemplars is all about figuring out how to improve health care based on evidence of what works. It will help governments use time and money more efficiently—and with the COVID-19 pandemic, there has never been a greater need to get the most impact out of every dollar spent.
I’m grateful to all the people in governments, academia, and non-profits who made the Exemplars program possible. We all started out with one goal in mind: to accelerate the progress in improving health, so that the poorest countries don't have 20 times the childhood death rate of the richest ones. I think Exemplars is a great resource that will spread success stories so even countries with very little money can benefit. And that will, ultimately, save lives.

Ripple effect
As COVID-19 spreads, don’t lose track of malaria
The pandemic is a reminder of why we need to eradicate this mosquito-borne disease.

Mosquitoes don’t practice social distancing. They don’t wear masks, either.
As COVID-19 spreads across the globe, it’s important to remember that the world’s deadliest animal hasn’t taken a break during this pandemic.
Mosquitoes are out biting every night, infecting millions of people with malaria—a disease that kills a child every other minute of every day.
Most of these deaths occur in the poorest countries with the weakest health systems. Now, they face the added burden of halting the coronavirus. And in many of these countries, COVID-19 cases are likely to peak at the worst possible time: the height of their malaria transmission seasons.
During the 2014 Ebola outbreak in West Africa, endemic diseases like malaria, tuberculosis and HIV/AIDS contributed to many more deaths than Ebola because the epidemic disrupted local health care systems. Health officials fear the same could happen with COVID-19.
Lockdowns and social distancing regulations have already made it difficult for health workers to provide malaria prevention and treatment in many parts of Africa. There have also been interruptions to supplies of essential malaria tools—like bed nets, anti-malaria medicines, and rapid diagnostic tests—that have been instrumental in cutting malaria deaths by more than half since 2000.
Now that incredible progress may be in jeopardy. A recent modeling analysis from the World Health Organization found that if essential malaria prevention and treatment services are severely disrupted by the pandemic, malaria deaths in sub-Saharan Africa would reach mortality levels not seen since 2000. That year, an estimated 764,000 people died from malaria in Africa, most of them children.
There is not a choice between saving lives from COVID-19 versus saving lives from malaria. The world must enable these countries to do both. Health officials urgently need to step up to the challenge of controlling the pandemic while also making sure that malaria, as well as other diseases like HIV and tuberculosis, are not neglected.
For malaria, that means continuing with campaigns to deliver long-lasting insecticide-treated bed nets, control mosquito populations with indoor spraying, and provide preventive treatment for pregnant women and children in high-risk communities. At the same time, health workers must deliver these services while not putting their communities at risk of the coronavirus.
The good news is that many countries are finding ways to maintain key malaria programs even in the face of the pandemic. In Benin, a country in West Africa with one of the highest burdens of malaria in the world, the government teamed up with Catholic Relief Services and our foundation this year to develop a new, innovative way to distribute bed nets across the country. Using smartphones, real time data collection, and satellite mapping, Benin has helped ensure that all families, no matter where they live, will be protected by a bed net at night. And scientists haven’t paused research efforts to find new ways to prevent malaria and control mosquito populations, like those underway at “Mosquito City” in Tanzania.
What’s exciting to see is how some existing malaria programs are also helping to control COVID-19. For example, emergency operations centers that track outbreaks of malaria in Africa are now being used to monitor the spread of COVID-19. By tracking the shape and movement of the pandemic across countries and regions, health officials are also able to deepen their understanding of health conditions in communities that will, in turn, help improve their responses to malaria in those areas.
The progress the world has made against malaria is one of the greatest global health success stories. The COVID-19 pandemic only reinforces why eradicating malaria is so essential. So long as malaria exists, it will continue to flare up and burden the most vulnerable communities. Ridding the world of preventable, treatable diseases like malaria will save millions of lives and lead to healthier, more prosperous communities. And that will make them better prepared to confront any new health challenges like COVID-19 in the future.

Amazing results
This partnership helped prevent 13 million deaths
Childhood deaths have been cut in half since 1990. Vaccines are a big reason why.

Vaccines have been saving lives for centuries. But from the time Edward Jenner created the first vaccine in the late 1700s, not everyone has had equal access to them. As a result, children in some parts of the world continued to die from diseases that were preventable in other parts.
When Melinda and I learned about this inequity over twenty years ago, we thought it was infuriating—and deeply unfair. So, in 2000, our foundation teamed up with countries whose children were impacted the most, the World Health Organization, the World Bank, UNICEF, vaccine manufactures, and donors to do something about it. Together, we created an organization called Gavi, the Vaccine Alliance.
Gavi works with governments to make sure that every child has access to the lifesaving vaccines they need. The organization makes this happen by negotiating vaccines at prices that are affordable for the poorest countries. Since Gavi guarantees high volumes, manufacturers are able to lower the cost of vaccines quite dramatically. Gavi also helps low-income countries strengthen systems to deliver vaccines to all communities.
Over the last two decades, Gavi has helped vaccinate more than 760 million children and prevented more than 13 million deaths. That’s a truly amazing result.
Governments and partners from around the world are meeting virtually today to raise funds for Gavi’s next five years of work. This investment is more important than ever before, because Gavi is going to play a key role in making sure that, when we have COVID-19 vaccines, they reach the most vulnerable people. Their expertise and experience in distributing vaccines will be invaluable as we work to end this outbreak once and for all.

The vaccine race, explained
What you need to know about the COVID-19 vaccine
Humankind has never had a more urgent task than creating broad immunity for coronavirus.

One of the questions I get asked the most these days is when the world will be able to go back to the way things were in December before the coronavirus pandemic. My answer is always the same: when we have an almost perfect drug to treat COVID-19, or when almost every person on the planet has been vaccinated against coronavirus.
The former is unlikely to happen anytime soon. We’d need a miracle treatment that was at least 95 percent effective to stop the outbreak. Most of the drug candidates right now are nowhere near that powerful. They could save a lot of lives, but they aren’t enough to get us back to normal.
Which leaves us with a vaccine.
Humankind has never had a more urgent task than creating broad immunity for coronavirus. Realistically, if we’re going to return to normal, we need to develop a safe, effective vaccine. We need to make billions of doses, we need to get them out to every part of the world, and we need all of this to happen as quickly as possible.
That sounds daunting, because it is. Our foundation is the biggest funder of vaccines in the world, and this effort dwarfs anything we’ve ever worked on before. It’s going to require a global cooperative effort like the world has never seen. But I know it’ll get done. There’s simply no alternative.
Here’s what you need to know about the race to create a COVID-19 vaccine.
The world is creating this vaccine on a historically fast timeline.
Dr. Anthony Fauci has said he thinks it’ll take around eighteen months to develop a coronavirus vaccine. I agree with him, though it could be as little as 9 months or as long as two years.
Although eighteen months might sound like a long time, this would be the fastest scientists have created a new vaccine. Development usually takes around five years. Once you pick a disease to target, you have to create the vaccine and test it on animals. Then you begin testing for safety and efficacy in humans.
Safety and efficacy are the two most important goals for every vaccine. Safety is exactly what it sounds like: is the vaccine safe to give to people? Some minor side effects (like a mild fever or injection site pain) can be acceptable, but you don’t want to inoculate people with something that makes them sick.
Efficacy measures how well the vaccine protects you from getting sick. Although you’d ideally want a vaccine to have 100 percent efficacy, many don’t. For example, this year’s flu vaccine is around 45 percent effective.
To test for safety and efficacy, every vaccine goes through three phases of trials:
- Phase one is the safety trial. A small group of healthy volunteers gets the vaccine candidate. You try out different dosages to create the strongest immune response at the lowest effective dose without serious side effects.
- Once you’ve settled on a formula, you move onto phase two, which tells you how well the vaccine works in the people who are intended to get it. This time, hundreds of people get the vaccine. This cohort should include people of different ages and health statuses.
- Then, in phase three, you give it to thousands of people. This is usually the longest phase, because it occurs in what’s called “natural disease conditions.” You introduce it to a large group of people who are likely already at the risk of infection by the target pathogen, and then wait and see if the vaccine reduces how many people get sick.
After the vaccine passes all three trial phases, you start building the factories to manufacture it, and it gets submitted to the WHO and various government agencies for approval.
This process works well for most vaccines, but the normal development timeline isn’t good enough right now. Every day we can cut from this process will make a huge difference to the world in terms of saving lives and reducing trillions of dollars in economic damage.
So, to speed up the process, vaccine developers are compressing the timeline. This graphic shows how:
In the traditional process, the steps are sequential to address key questions and unknowns. This can help mitigate financial risk, since creating a new vaccine is expensive. Many candidates fail, which is why companies wait to invest in the next step until they know the previous step was successful.
For COVID-19, financing development is not an issue. Governments and other organizations (including our foundation and an amazing alliance called the Coalition for Epidemic Preparedness Innovations) have made it clear they will support whatever it takes to find a vaccine. So, scientists are able to save time by doing several of the development steps at once. For example, the private sector, governments, and our foundation are going to start identifying facilities to manufacture different potential vaccines. If some of those facilities end up going unused, that’s okay. It’s a small price to pay for getting ahead on production.
Fortunately, compressing the trial timeline isn’t the only way to take a process that usually takes five years and get it done in 18 months. Another way we’re going to do that is by testing lots of different approaches at the same time.
There are dozens of candidates in the pipeline.
As of April 9, there are 115 different COVID-19 vaccine candidates in the development pipeline. I think that eight to ten of those look particularly promising. (Our foundation is going to keep an eye on all the others to see if we missed any that have some positive characteristics, though.)
The most promising candidates take a variety of approaches to protecting the body against COVID-19. To understand what exactly that means, it’s helpful to remember how the human immune system works.
When a disease pathogen gets into your system, your immune system responds by producing antibodies. These antibodies attach themselves to substances called antigens on the surface of the microbe, which sends a signal to your body to attack. Your immune system keeps a record of every microbe it has ever defeated, so that it can quickly recognize and destroy invaders before they make you ill.
Vaccines circumvent this whole process by teaching your body how to defeat a pathogen without ever getting sick. The two most common types—and the ones you’re probably most familiar with—are inactivated and livevaccines. Inactivated vaccines contain pathogens that have been killed. Live vaccines, on the other hand, are made of living pathogens that have been weakened (or “attenuated”). They’re highly effective but more prone to side effects than their inactivated counterparts.
Inactivated and live vaccines are what we consider “traditional” approaches. There are a number of COVID-19 vaccine candidates of both types, and for good reason: they’re well-established. We know how to test and manufacture them.
The downside is that they’re time-consuming to make. There’s a ton of material in each dose of a vaccine. Most of that material is biological, which means you have to grow it. That takes time, unfortunately.
That’s why I’m particularly excited by two new approaches that some of the candidates are taking: RNA and DNA vaccines. If one of these new approaches pans out, we’ll likely be able to get vaccines out to the whole world much faster. (For the sake of simplicity, I’m only going to explain RNA vaccines. DNA vaccines are similar, just with a different type of genetic material and method of administration.)
Our foundation—both through our own funding and through CEPI—has been supporting the development of an RNA vaccine platform for nearly a decade. We were planning to use it to make vaccines for diseases that affect the poor like malaria, but now it’s looking like one of the most promising options for COVID. The first candidate to start human trials was an RNA vaccine created by a company called Moderna.
Here’s how an RNA vaccine works: rather than injecting a pathogen’s antigen into your body, you instead give the body the genetic code needed to produce that antigen itself. When the antigens appear on the outside of your cells, your immune system attacks them—and learns how to defeat future intruders in the process. You essentially turn your body into its own vaccine manufacturing unit.
Because RNA vaccines let your body do most of the work, they don’t require much material. That makes them much faster to manufacture. There’s a catch, though: we don’t know for sure yet if RNA is a viable platform for vaccines. Since COVID would be the first RNA vaccine out of the gate, we have to prove both that the platform itself works and that it creates immunity. It’s a bit like building your computer system and your first piece of software at the same time.
Even if an RNA vaccine continues to show promise, we still must continue pursuing the other options. We don’t know yet what the COVID-19 vaccine will look like. Until we do, we have to go full steam ahead on as many approaches as possible.
It might not be a perfect vaccine yet—and that’s okay.
The smallpox vaccine is the only vaccine that’s wiped an entire disease off the face of the earth, but it’s also pretty brutal to receive. It left a scar on the arm of anyone who got it. One out of every three people had side effects bad enough to keep them home from school or work. A small—but not insignificant—number developed more serious reactions.
The smallpox vaccine was far from perfect, but it got the job done. The COVID-19 vaccine might be similar.
If we were designing the perfect vaccine, we’d want it to be completely safe and 100 percent effective. It should be a single dose that gives you lifelong protection, and it should be easy to store and transport. I hope the COVID-19 vaccine has all of those qualities, but given the timeline we’re on, it may not.
The two priorities, as I mentioned earlier, are safety and efficacy. Since we might not have time to do multi-year studies, we will have to conduct robust phase 1 safety trials and make sure we have good real-world evidence that the vaccine is completely safe to use.
We have a bit more wiggle room with efficacy. I suspect a vaccine that is at least 70 percent effective will be enough to stop the outbreak. A 60 percent effective vaccine is useable, but we might still see some localized outbreaks. Anything under 60 percent is unlikely to create enough herd immunity to stop the virus.
The big challenge will be making sure the vaccine works well in older people. The older you are, the less effective vaccines are. Your immune system—like the rest of your body—ages and is slower to recognize and attack invaders. That’s a big issue for a COVID-19 vaccine, since older people are the most vulnerable. We need to make sure they’re protected.
The shingles vaccine—which is also targeted to older people—combats this by amping up the strength of the vaccine. It’s possible we do something similar for COVID, although it might come with more side effects. Health authorities could also ask people over a certain age to get an additional dose.
Beyond safety and efficacy, there are a couple other factors to consider:
- How many doses will it be? A vaccine you only get once is easier and quicker to deliver. But we may need a multi-dose vaccine to get enough efficacy.
- How long does it last? Ideally, the vaccine will give you long-lasting protection. But we might end up with one that only stops you from getting sick for a couple months (like the seasonal flu vaccine, which protects you for about six months). If that happens, the short-term vaccine might be used while we work on a more durable one.
- How do you store it? Many common vaccines are kept at 4 degrees C. That’s around the temperature of your average refrigerator, so storage and transportation is easy. But RNA vaccines need to be stored at much colder temperature—as low as -80 degrees C—which will make reaching certain parts of the world more difficult.
My hope is that the vaccine we have 18 months from now is as close to “perfect” as possible. Even if it isn’t, we will continue working to improve it. After that happens, I suspect the COVID-19 vaccine will become part of the routine newborn immunization schedule.
Once we have a vaccine, though, we still have huge problems to solve. That’s because…
We need to manufacture and distribute at least 7 billion doses of the vaccine.
In order to stop the pandemic, we need to make the vaccine available to almost every person on the planet. We’ve never delivered something to every corner of the world before. And, as I mentioned earlier, vaccines are particularly difficult to make and store.
There’s a lot we can’t figure out about manufacturing and distributing the vaccine until we know what exactly we’re working with. For example, will we be able to use existing vaccine factories to make the COVID-19 vaccine?
What we can do now is build different kinds of vaccine factories to prepare. Each vaccine type requires a different kind of factory. We need to be ready with facilities that can make each type, so that we can start manufacturing the final vaccine (or vaccines) as soon as we can. This will cost billions of dollars. Governments need to quickly find a mechanism for making the funding for this available. Our foundation is currently working with CEPI, the WHO, and governments to figure out the financing.
Part of those discussions center on who will get the vaccine when. The reality is that not everyone will be able to get the vaccine at the same time. It’ll take months—or even years—to create 7 billion doses (or possibly 14 billion, if it’s a multi-dose vaccine), and we should start distributing them as soon as the first batch is ready to go.
Most people agree that health workers should get the vaccine first. But who gets it next? Older people? Teachers? Workers in essential jobs?
I think that low-income countries should be some of the first to receive it, because people will be at a much higher risk of dying in those places. COVID-19 will spread much quicker in poor countries because measures like physical distancing are harder to enact. More people have poor underlying health that makes them more vulnerable to complications, and weak health systems will make it harder for them to receive the care they need. Getting the vaccine out in low-income countries could save millions of lives. The good news is we already have an organization with expertise about how to do this in Gavi, the Vaccine Alliance.
With most vaccines, manufacturers sign a deal with the country where their factories are located, so that country gets first crack at the vaccines. It’s unclear if that’s what will happen here. I hope we find a way to get it out on an equitable basis to the whole world. The WHO and national health authorities will need to develop a distribution plan once we have a better understanding of what we’re working with.
Eventually, though, we’re going to scale this thing up so that the vaccine is available to everyone. And then, we’ll be able to get back to normal—and to hopefully make decisions that prevent us from being in this situation ever again.
It might be a bit hard to see right now, but there is a light at the end of the tunnel. We’re doing the right things to get a vaccine as quickly as possible. In the meantime, I urge you to continue following the guidelines set by your local authorities. Our ability to get through this outbreak will depend on everyone doing their part to keep each other safe.

Innovation vs. the coronavirus
The first modern pandemic (short read)
The scientific advances we need to defeat COVID-19.

This post originally appeared as an opinion piece in the Washington Post. It’s adapted from a longer article, which you can read here.
It’s entirely understandable that the national conversation has turned to a single question: “When can we get back to normal?” The shutdown has caused immeasurable pain in jobs lost, people isolated, and worsening inequity. People are ready to get going again.
Unfortunately, although we have the will, we don’t have the way—not yet. Before the United States and other countries can return to business and life as usual, we will need some innovative new tools that help us detect, treat, and prevent COVID-19.
It begins with testing. We can’t defeat an enemy if we don’t know where it is. To reopen the economy, we need to be testing enough people that we can quickly detect emerging hotspots and intervene early. We don’t want to wait until the hospitals start to fill up and more people die.
Innovation can help us get the numbers up. The current coronavirus tests require that health-care workers perform nasal swabs, which means they have to change their protective gear before every test. But our foundation supported research showing that having patients do the swab themselves produces results that are just as accurate. This self-swab approach is faster and safer, since regulators should be able to approve swabbing at home or in other locations rather than having people risk additional contact.
Another diagnostic test under development would work much like an at-home pregnancy test. You would swab your nose, but instead of sending it into a processing center, you’d put it in a liquid and then pour that liquid onto a strip of paper, which would change color if the virus was present. This test may be available in a few months.
We need one other advance in testing, but it’s social, not technical: consistent standards about who can get tested. If the country doesn’t test the right people—essential workers, people who are symptomatic, and those who have been in contact with someone who tested positive—then we’re wasting a precious resource and potentially missing big reserves of the virus. Asymptomatic people who aren’t in one of those three groups should not be tested until there are enough tests for everyone else.
The second area where we need innovation is contact tracing. Once someone tests positive, public-health officials need to know who else that person might have infected.
For now, the United States can follow Germany’s example: interview everyone who tests positive and use a database to make sure someone follows up with all their contacts. This approach is far from perfect, because it relies on the infected person to report their contacts accurately and requires a lot of staff to follow up with everyone in person. But it would be an improvement over the sporadic way that contact tracing is being done across the United States now.
An even better solution would be the broad, voluntary adoption of digital tools. For example, there are apps that will help you remember where you have been; if you ever test positive, you can review the history or choose to share it with whoever comes to interview you about your contacts. And some people have proposed allowing phones to detect other phones that are near them by using Bluetooth and emitting sounds that humans can’t hear. If someone tested positive, their phone would send a message to the other phones, and their owners could get tested. If most people chose to install this kind of application, it would probably help some.
Naturally, anyone who tests positive will immediately want to know about treatment options. Yet, right now, there is no treatment for COVID-19. Hydroxychloroquine, which works by changing the way the human body reacts to a virus, has received a lot of attention. Our foundation is funding a clinical trial that will give an indication whether it works on COVID-19 by the end of May, and it appears the benefits will be modest at best.
But several more-promising candidates are on the horizon. One involves drawing blood from patients who have recovered from COVID-19, making sure it is free of the coronavirus and other infections, and giving the plasma (and the antibodies it contains) to sick people. Several major companies are working together to see whether this succeeds.
Another type of drug candidate involves identifying the antibodies that are most effective against the novel coronavirus, and then manufacturing them in a lab. If this works, it is not yet clear how many doses could be produced; it depends on how much antibody material is needed per dose. In 2021, manufacturers may be able to make as few as 100,000 treatments or many millions.
If, a year from now, people are going to big public events—such as games or concerts in a stadium—it will be because researchers have discovered an extremely effective treatment that makes everyone feel safe to go out again. Unfortunately, based on the evidence I’ve seen, they’ll likely find a good treatment, but not one that virtually guarantees you’ll recover.
That’s why we need to invest in a fourth area of innovation: making a vaccine. Every additional month that it takes to produce a vaccine is a month in which the economy cannot completely return to normal.
The new approach I’m most excited about is known as an RNA vaccine. (The first COVID-19 vaccine to start human trials is an RNA vaccine.) Unlike a flu shot, which contains fragments of the influenza virus so your immune system can learn to attack them, an RNA vaccine gives your body the genetic code needed to produce viral fragments on its own. When the immune system sees these fragments, it learns how to attack them. An RNA vaccine essentially turns your body into its own vaccine manufacturing unit.
There are at least five other efforts that look promising. But because no one knows which approach will work, a number of them need to be funded so they can all advance at full speed simultaneously.
Even before there’s a safe, effective vaccine, governments need to work out how to distribute it. The countries that provide the funding, the countries where the trials are run, and the ones that are hardest-hit will all have a good case that they should receive priority. Ideally, there would be global agreement about who should get the vaccine first, but given how many competing interests there are, this is unlikely to happen. Whoever solves this problem equitably will have made a major breakthrough.
World War II was the defining moment of my parents’ generation. Similarly, the coronavirus pandemic—the first in a century—will define this era. But there is one big difference between a world war and a pandemic: All of humanity can work together to learn about the disease and develop the capacity to fight it. With the right tools in hand, and smart implementation, we will eventually be able to declare an end to this pandemic—and turn our attention to how to prevent and contain the next one.

3 steps
What our leaders can do now
These decisions will affect the course of COVID-19.

There’s no question the United States missed the opportunity to get ahead of the novel coronavirus. But the window for making important decisions hasn’t closed. The choices we and our leaders make now will have an enormous impact on how soon case numbers start to go down, how long the economy remains shut down and how many Americans will have to bury a loved one because of COVID-19.
Our foundation has been working to slow the outbreak for several months. To date, we’ve invested $105 million in efforts to create new therapeutics, expand access to testing, and limit the virus’s impact here in Seattle.
As a result of this work, I’ve spoken with experts and leaders in Washington and across the country. It’s become clear to me that we must take three steps.
First, we need a consistent nationwide approach to shutting down. Despite urging from public health experts, some states and counties haven’t shut down completely. In some states, beaches are still open; in others, restaurants still serve sit-down meals.
This is a recipe for disaster. Because people can travel freely across state lines, so can the virus. The country’s leaders need to be clear: Shutdown anywhere means shutdown everywhere. Until the case numbers start to go down across America—which could take 10 weeks or more—no one can continue business as usual or relax the shutdown. Any confusion about this point will only extend the economic pain, raise the odds that the virus will return, and cause more deaths.
Second, the federal government needs to step up on testing. Far more tests should be made available. We should also aggregate the results so we can quickly identify potential volunteers for clinical trials and know with confidence when it’s time to return to normal. There are good examples to follow: New York state recently expanded its capacity to more than 25,000 tests per day.
There’s also been some progress on more efficient testing methods, such as the self-swab developed by the Seattle Coronavirus Assessment Network, which allows patients to take a sample themselves without possibly exposing a health worker. I hope this and other innovations in testing are scaled up across the country soon.
Even so, demand for tests will probably exceed the supply for some time, and right now, there’s little rhyme or reason to who gets the few that are available. As a result, we don’t have a good handle on how many cases there are or where the virus is likely headed next, and it will be hard to know if it rebounds later. And because of the backlog of samples, it can take seven days for results to arrive when we need them within 24 hours.
This is why the country needs clear priorities for who is tested. First on the list should be people in essential roles such as health-care workers and first responders followed by highly symptomatic people who are most at risk of becoming seriously ill and those who are likely to have been exposed.
The same goes for masks and ventilators. Forcing 50 governors to compete for lifesaving equipment—and hospitals to pay exorbitant prices for it—only makes matters worse.
Finally, we need a data-based approach to developing treatments and a vaccine. Scientists are working full speed on both; in the meantime, leaders can help by not stoking rumors or panic buying. Long before the drug hydroxychloroquine was approved as an emergency treatment for COVID-19, people started hoarding it, making it hard to find for lupus patients who needed it to survive.
We should stick with the process that works: Run rapid trials involving various candidates and inform the public when the results are in. Once we have a safe and effective treatment, we’ll need to ensure that the first doses go to the people who need them most.
To bring the disease to an end, we’ll need a safe and effective vaccine. If we do everything right, we could have one in less than 18 months—the fastest a vaccine has ever been developed. But creating a vaccine is only half the battle. To protect Americans and people around the world, we’ll need to manufacture billions of doses.
Without a vaccine, developing countries are at even greater risk than wealthy ones, because it’s even harder for them to do physical distancing and shutdowns. The further down the income ladder people live, the more important it is that they go to work every day just to feed their family.
If they live in the poorest parts of sub-Saharan Africa or India, staying home simply isn’t an option. Even if they do stay home, they can’t just wall themselves off from their neighbors; in slums, the houses are packed together so closely that there’s no way to keep your distance. All the work that rich countries are doing now to develop vaccines will save lives in those places, too.
We can get a head start on manufacturing all of the doses we’ll need now by building the facilities where these vaccines will be made. Because many of the top candidates are made using unique equipment, we’ll have to build facilities for each of them, knowing that some won’t get used. Private companies can’t take that kind of risk, but the federal government can. It’s a great sign that the administration made deals this week with at least two companies to prepare for vaccine manufacturing. I hope more deals will follow.
In 2015, I urged world leaders in a TED talk to prepare for a pandemic the same way they prepare for war—by running simulations to find the cracks in the system. As we’ve seen this year, we have a long way to go. But I still believe that if we make the right decisions now, informed by science, data, and experience of medical professionals, we can save lives and get the country back to work.
A version of this post originally appeared on the website of the Washington Post.

Handling coronavirus
How to respond to COVID-19
And prepare for the next epidemic, too.

In any crisis, leaders have two equally important responsibilities: solve the immediate problem and keep it from happening again. The COVID-19 pandemic is an excellent case in point. The world needs to save lives now while also improving the way we respond to outbreaks in general. The first point is more pressing, but the second has crucial long-term consequences.
The long-term challenge—improving our ability to respond to outbreaks—isn’t new. Global health experts have been saying for years that another pandemic rivalling the speed and severity of the 1918 influenza epidemic wasn’t a matter of if but when. The Bill & Melinda Gates Foundation has committed significant resources in recent years to helping the world prepare for such a scenario.
Now, in addition to the perennial challenge, we face an immediate crisis. In the past week, COVID-19 has started to behave a lot like the once-in-a-century pathogen we’ve been worried about. I hope it’s not that bad, but we should assume that it will be until we know otherwise.
There are two reasons that COVID-19 is such a threat. First, it can kill healthy adults in addition to elderly people with existing health problems. The data so far suggests that the virus has a case fatality risk around 1%; this rate would make it several times more severe than typical seasonal influenza and would put it somewhere between the 1957 influenza pandemic (0.6%) and the 1918 influenza pandemic (2%).
Second, COVID-19 is transmitted quite efficiently. The average infected person spreads the disease to two or three others. That’s an exponential rate of increase. There is also strong evidence that it can be transmitted by people who are just mildly ill or not even showing symptoms yet. This means COVID-19 will be much harder to contain than Middle East Respiratory Syndrome or Severe Acute Respiratory Syndrome (SARS), which were only spread by those showing symptoms and were much less efficiently transmitted. In fact, COVID-19 has already caused 10 times as many cases as SARS in just a quarter of the time.
The good news is that national, state, and local governments and public health agencies can take steps over the next few weeks to slow the spread of COVID-19.
For example, in addition to helping their own citizens respond, donor governments should help low- and middle-income countries prepare for this pandemic. The health systems in many of these countries are already stretched thin, and a pathogen like coronavirus can quickly overwhelm them. And poorer countries have little political or economic leverage, given wealthier countries’ natural desire to put their own people first.
By helping countries in Africa and South Asia get ready now, we can save lives and also slow the global circulation of the virus. (A significant portion of the commitment Melinda and I recently made to help kickstart the global response to COVID-19—which could total up to $100 million—is focused particularly on developing countries.)
The world also needs to accelerate work on treatments and vaccines for COVID-19. Scientists were able to sequence the genome of the virus and develop several promising vaccine candidates in a matter of days, and the Coalition for Epidemic Preparedness Innovations is already preparing up to eight promising vaccine candidates for clinical trials. If one or more of these vaccines proves safe and effective in animal models, they could be ready for larger-scale trials as early as June. Drug discovery can also be accelerated by drawing on libraries of compounds that have already been tested for safety and by applying new screening techniques, including machine learning, to identify antivirals that could be ready for large-scale clinical trials within weeks.
All these steps would help address the current crisis. But we also need to make larger systemic changes so we can respond more efficiently and effectively when the next epidemic arrives.
It’s essential to help low- and middle-income countries strengthen their primary health care systems. When you build a health clinic, you’re also creating part of the infrastructure for fighting epidemics. Trained health care workers not only deliver vaccines; they can also monitor disease patterns, serving as part of the early warning systems that will alert the world to potential outbreaks.
The world also needs to invest in disease surveillance, including a case database that is instantly accessible to the relevant organizations and rules that require countries to share their information. Governments should have access to lists of trained personnel, from local leaders to global experts, who are prepared to deal with an epidemic immediately, as well as lists of supplies to be stockpiled or redirected in an emergency.
In addition, we need to build a system that can develop safe and effective vaccines and antivirals, get them approved, and deliver billions of doses within a few months of the discovery of a fast-moving pathogen. That’s a tough challenge that presents technical, diplomatic, and budgetary obstacles, as well as demanding partnership between the public and private sectors. But all these obstacles can be overcome.
One of the main technical challenges for vaccines is to improve on the old ways of manufacturing proteins, which are just too slow for responding to an epidemic. We need to develop platforms that are predictably safe, so regulatory reviews can happen quickly, and that make it easy for manufacturers to produce doses at a low cost and a massive scale. For antivirals, there will need to be an organized system to screen existing treatments and candidate molecules in a swift and standardized manner.
Another technical challenge involves constructs based on nucleic acids. These constructs can be produced within hours after a virus’s genome has been sequenced; now we need to find ways to produce them at scale.
In addition to these technical solutions, we’ll need diplomatic efforts to drive international collaboration and data sharing. Developing antivirals and vaccines involves massive clinical trials and licensing agreements that would cross national borders. We should make the most of global forums that can help achieve consensus on research priorities and trial protocols so that promising vaccine and antiviral candidates can move quickly through this process. These platforms include the World Health Organization R&D Blueprint, the International Severe Acute Respiratory and Emerging Infection Consortium trial network, and the Global Research Collaboration for Infectious Disease Preparedness. The goal of this work should be to get conclusive clinical trial results and regulatory approval in three months or less, without compromising patients’ safety.
Then there is the question of funding. Budgets for these efforts need to be expanded several times over. Billions more dollars are needed to complete Phase III trials and secure regulatory approval for coronavirus vaccines, and still more funding will be needed to improve disease surveillance and response.
Why does this require government funding—can’t the private sector solve this on its own? Pandemic products are extraordinarily high-risk investments, and pharmaceutical companies will need public funding to de-risk their work and get them to jump in with both feet. In addition, governments and other donors will need to fund—as a global public good—manufacturing facilities that can generate a vaccine supply in a matter of weeks. These facilities can make vaccines for routine immunization programs in normal times and be quickly refitted for production during a pandemic. Finally, governments will need to finance the procurement and distribution of vaccines to the populations that need them.
Obviously, billions of dollars for anti-pandemic efforts is a lot of money. But that’s the scale of investment required to solve the problem. And given the economic pain that an epidemic can impose—just look at the way COVID-19 is disrupting supply chains and stock markets, not to mention people’s lives—it will be a bargain.
Finally, governments and industry will need to come to an agreement: During a pandemic, vaccines and antivirals won’t simply be sold to the highest bidder. They’ll be available and affordable for people who are at the heart of the outbreak and in greatest need. Not only is this the right thing to do, it’s also the right strategy for short-circuiting transmission and preventing future pandemics.
These are the actions that leaders should be taking now. There is no time to waste.
This post originally appeared on the website of the New England Journal of Medicine. I wrote there about the need for a global pandemic response system in 2015, and about the threat posed by a novel respiratory virus in 2018.

Genetics and AI
My message to America’s top scientists
How two technologies can benefit the world’s poorest.

People often ask me which technologies have the most potential to change our lives in the decades ahead.
AI is always near the top of the list. It can help us make sense of complex biological systems—like the microbiome in the human gut—and give us new insight into tough problems in global health, such as premature birth.
Gene-based tools are another technology that I always mention. For example, advances in that field are giving researchers powerful new tools to investigate potential cures for AIDS, sickle-cell disease, and other conditions.
These tools can also give us key insights into new diseases, such as the novel coronavirus that recently emerged, so that we can develop diagnostic tests, treatments, and vaccines faster.
Thanks to these and other breakthroughs, science is giving us the opportunity to improve lives more rapidly than ever. But we’ll only make the most of that potential if we ensure that these tools reach everyone who needs them, including the poorest people in the world.
That’s the focus of much of our work at the Gates Foundation. Today I’m honored to be giving a speech on this subject at the annual meeting of the American Association for the Advancement of Science. Here’s what I plan to say:
Remarks as prepared
Seattle, WA
February 14, 2020
American Association for the Advancement of Science
Thank you. It’s great to be here today.
The Coronavirus
I want to take a few minutes to talk about the novel coronavirus, which I know is on everyone’s mind.
Our foundation has committed up to $100 million to address this new coronavirus because we believe it poses a serious threat to global health. This money will support efforts to detect, isolate, and treat confirmed cases, help countries in sub-Saharan Africa and South Asia take steps to prepare for the epidemic and protect their most vulnerable citizens, and accelerate the development of vaccines, treatments, and diagnostics.
We believe that multilateral organizations and national governments must make every effort to stop this outbreak, but we also want to help the world be better prepared if it becomes a global pandemic. Above all, we believe that the world will need to be guided by science, not fear, in the weeks ahead.
The Diseases of Poverty
A few blocks from here is the foundation that Melinda and I started in 2000. When we decided to focus on philanthropy, we knew that the core of our work would be eliminating the gross inequities in health that we had seen a few years earlier on our first trip to Africa.
One area where we believed we could make a difference was investing in R&D to address diseases of poverty. Today, I want to talk about several exciting and important tools of modern science that have the potential to help us solve some of the biggest health problems—not only in low- and middle-income countries, but everywhere.
To be sure, health in lower-income countries has improved. Over the last 25 years, we’ve nearly eradicated polio. Child mortality has been cut in half. And we’ve significantly reduced deaths from HIV, TB, and malaria.
But there is still room for a lot more improvement.
This year, more than 5 million children under the age of five will die. HIV, TB, malaria, and other diseases still kill millions of people every year. And nearly a quarter of a billion children are malnourished. Almost all of this disease burden is carried by people in the poorest countries on the planet.
Innovation with Equity in Mind
To make further inroads against the diseases of poverty, we need every sector to engage. Governments need to continue funding of basic research; partners like our foundation need to nurture the best ideas through discovery and translation; and the private sector needs to develop solutions that are commercially viable, affordable, and scalable in countries with limited resources and fragile health care systems.
The private sector has much to gain from pursuing breakthroughs that benefit people in lower-income countries. Over the next few decades, developing economies will continue to expand. By 2050, the population of sub-Saharan Africa will more than double to almost 2.5 billion. That’s more than twice the forecasted population of the Europe and North America combined.
Yet, today, the overwhelming percentage of investments in health R&D reflect market opportunities in rich countries. If we stick to this model, market forces will continue to prioritize development of costly products designed to meet the needs of the few and unaffordable to most. Imagine if we turned this traditional market model on its head and committed to designing new vaccines, therapeutics, and diagnostics with equity in mind.
Today, we have an opportunity with the evolution of tools like AI and gene-based technologies to develop a new generation of health solutions that can benefit everyone, everywhere. This is what really excites me about the future.
The Potential of AI and Gene Therapy
As a 7th grader at the Lakeside School here in Seattle, I became fascinated not only with computers, but also with Shakey, the Mobile Robot. Life Magazine called Shakey the “first electronic person.” That might have been overstating it a bit, but Shakey was an early example of how artificial intelligence could be applied. It had a limited ability to perceive objects in its environment and adapt its movement. It could plan simple travel routes, and it had the ability to rearrange simple objects. For its time, Shakey was really cool.
Since Alan Turing laid the groundwork for artificial intelligence in 1950, AI has gone through a kind of boom-and-bust cycle—enthusiasm would grow and then expectations weren’t met.
But we are finally beginning to realize the potential of AI. The computational power available for AI applications is doubling every three and half months—far surpassing the historical metric of Moore’s Law. This processing capability is being coupled with troves of new data, and we are learning to annotate this data in smarter ways. That’s enabling us to realize some of the promises of AI: the ability to synthesize, analyze, see patterns, gain insights, and make predictions across many, many more dimensions than a human can comprehend.
This data revolution will apply to virtually all of the disciplines represented here today. What I’m most excited about is how it can help us make sense of complex biological systems and accelerate the discovery of therapeutics to improve health in the poorest countries.
And, with recent breakthroughs in gene-editing technologies like CRISPR, we are on the verge of a new era of precision diagnostics, therapeutics, and vaccines that has the potential to improve health—not only for rare genetic disorders, but also for diseases that predominately afflict people in poor countries.
It’s amazing to think how far we’ve come since Crick, Watson, and Franklin laid the foundation for modern genetics. It was only 15 years ago that the Human Genome Project gave us the ability to read our DNA and identify specific sequences that cause or contribute to disease. It was only 8 years ago that CRISPR gave us the ability to edit DNA precisely.
Now, with the latest CRISPR gene-editing approaches, it’s believed that up to 89% of genetic variants known to be associated with human disease can be corrected.
Last year, researchers began using the molecular scissors of CRISPR in clinical trials to remove, edit, and inject people’s cells back into their bodies.
In short, artificial intelligence and CRISPR have emerged as powerful tools with the potential to revolutionize healthcare and many other fields.
The Product Pipeline for Global Health
I’d like to share a few examples of innovations in the pipeline that make me optimistic about the future.
Our foundation is working with the National Institutes of Health to develop affordable, gene-based cures for sickle cell disease and HIV. The goal is to move these solutions into clinical trials in the next 7-10 years. This would be a huge breakthrough.
Of the 38 million people worldwide living with HIV, 95 percent live in lower-income countries and one-third aren’t receiving treatment. Imagine if we could cure every one of them.
Sickle Cell Disease is also a major health burden in lower-income countries. Fifteen million babies will be born with sickle cell disease in the next 30 years, the vast majority in Africa. Although exact numbers are hard to come by, at least half and maybe as many as 90% of these children will die before their fifth birthday.
In recent years, we’ve seen gene-based therapies introduced for some rare genetic diseases as well as for sickle cell disease. Ongoing trials are promising, with early results showing clinical benefit to more than a dozen people with sickle cell disease. But the treatments are prohibitively expensive—likely to cost $1 million or more per person.
And they require highly trained doctors and state-of-the-art hospitals to administer the cures—which involve in vitro editing of bone marrow stem cells for reinfusion, and toxic bone marrow conditioning regimens.
The focus of our work with the NIH on sickle cell disease is to develop effective, durable, safe, and affordable gene-based cures that don’t require costly hospital stays.
We hope to create in vivo gene editing techniques that can be delivered with a single injection using vectors that target and edit blood-forming cells in the bone marrow—with high efficiency. This approach could reach millions of patients in primary care facilities at a fraction of the cost.
Similarly, with HIV, the purpose of our collaboration with the NIH is to investigate the use of in vivo gene editing and other technologies that could drive a functional cure for those infected with HIV in an affordable, scalable way. A high bar, for sure, but it’s the kind of bold approach to designing therapeutic innovation with equity in mind that excites me.
Gene editing shows great promise for our work in malaria, too. The world has made huge progress against malaria in the past two decades. Since 2000, deaths have dropped from about 1 million per year to 400,000 per year. But further progress requires new tools and strategies.
Researchers are exploring the use of CRISPR to create “gene drives” that suppress the handful of mosquito species most responsible for malaria transmission. They are also working on introducing genes that could eliminate the parasites as they pass through a mosquito’s gut on their way to its salivary glands.
Newborn Health
One area where I see great potential for progress is newborn health. As you’ll see on this chart, nearly half of the 5.3 million children under age 5 who die this year will die in the first 28 days of life.
Deaths from complications associated with premature births account for the single largest percentage of neonatal mortality. The reason the number of deaths is so high is that there is still so much we don’t know about the root causes of prematurity and neonatal mortality. We are funding several studies to help solve this mystery.
First, by applying artificial intelligence to a range of complex data sets, we are learning about the biological pathways leading to prematurity and low birth weight.
Second, we’re combining clinical data with information from low-cost devices like a hand-held ultrasound and wearable sensors—and using AI to identify indicators that a pregnant woman may be at risk of giving birth before full term. We can do something similar to look for signs that newborns may be in trouble.
Third, researchers are exploring the associations between maternal undernutrition, the maternal microbiome, and premature birth. By distinguishing abnormal changes in the microbiome during pregnancy, we may be able to give pregnant women microbial therapeutics—as well as nutritional interventions—to improve fetal growth and reduce the risk of pre-term birth.
The Microbiome
It is increasingly clear that the gut microbiome and nutrition—and the interplay between the two—are also big factors in child health and development.
An estimated 225 million children worldwide are severely malnourished—and malnutrition is an underlying cause of more than 40 percent of under-five child mortality. Children who are malnourished often have underdeveloped microbiomes that make them more vulnerable to disease and to cognitive impairments that last a lifetime.
There is also evidence that children in wealthy countries who grow up in super-hygienic environments – with an abundance of processed foods and antibiotics—have poor gut health that may make them more susceptible to obesity, diabetes, allergies, and maybe even auto-immune disease.
But there’s still a lot we don’t know about the microbiome—including which bacterial species are most critical for health and whether augmenting these species can reduce malnutrition. Deciphering the human microbiome is not an easy task. It contains more than 100 trillion organisms and 200 times more genetic material than the human genome.
Using artificial intelligence, scientists hope to analyze the composition of the trillions of microbes in our body and identify the patterns, interactions, and changes we can't see that indicate a higher risk of disease—or, conversely—a protective shield against disease.
One tool that’s helping us understand how to optimize the gut microbiome is technology called “organs-on-a-chip.” In simple terms, this technology allows in vitro modeling of human organs in ways that mimic how organs perform normally . . . and when they are diseased.
Linking different organ chips together—for example, intestine, liver, and kidney chips—can enable researchers to model human drug kinetics.
Culturing a human intestinal microbiome-on-a-chip can enable researchers to probe the complex interactions between microbiome, host, nutrients, and pathogens in a systematic way.
Researchers are using this technology to study the vaginal microbiome and therapeutics that could reduce the incidence of pre-term birth and risk of HIV infection. We’re also supporting other “organ-on-a-chip” studies, including one that’s using lymphoid organoids to understand vaccine responses.
This technology has the potential to shave years off the time it takes to evaluate the safety and efficacy of new drugs, vaccines, and other therapeutics—and save hundreds of millions of dollars associated with research and clinical trials.
Climate Change and Agricultural Adaptation
I’ve been talking about the innovation we need to build on recent progress in global health. Many people are surprised when I say that progress in global health also depends on the fight against climate change.
There are two parts to addressing climate change. Mitigation and adaptation. Mitigation is about what we need to do to get to zero on greenhouse gases that are warming the climate.
Adaptation is about helping people cope with the changing climate. It’s unfortunate, but true, that the people who are most affected by climate change today account for a tiny amount of the world’s greenhouse gasses. Specifically, the 2 billion smallholder farmers and their families who rely on the food they grow to survive.
Increasingly, climate change is putting their livelihoods—and their lives—at risk. More extreme weather conditions mean more floods, more droughts, and more plant pests and diseases that can wipe out a crop.
When smallholder farmers lose their harvest, their kids may not have enough to eat and that makes them susceptible to the effects of malnutrition.
To adapt, farming families need seeds and livestock that have been bred to thrive in the more extreme conditions caused by climate change.
The world’s largest agriculture research group, CGIAR, has developed dozens of new varieties of maize and rice that can withstand drought—including one called “scuba” rice that can survive for two weeks under floodwaters.
A team of scientists led from the University of Cambridge is using evolutionary genomics to help maize and other cereals partner more effectively with microorganisms in the soil to capture nutrients and water.
For farmers with poor soils and no access to fertilizer, this process could supply the nitrogen needed to increase production. That’s good for food security, farmers’ livelihoods, and the environment.
Conclusion
Earlier this week, Melinda and I released our 2020 annual letter. It’s something we’ve done every year for the last 10 years. This year, we reflected on the progress in global health since we started our foundation 20 years ago and the challenges that remain. And we talk about where things stand with the primary focus of our work in the US—improving K-12 and postsecondary education.
These issues share one very important feature in common. They are both key to a healthier, better, and more equal world. Disease is both a symptom and a cause of inequality, while public education is a driver of equality.
When we first started our foundation, we were optimistic about the power of innovation to drive progress. Looking at progress in global health over the last two decades and the amazing advances I talked about today, I’m more optimistic than ever that we are closer to the goal of giving every person the opportunity to live a healthy, productive life. Thank you.

Inequality in the next decade
What I’m thinking about this New Year’s Eve
As the year comes to an end, I reflect on how we can make our tax system more fair.

Where will you be when the ball drops at midnight on New Year’s Eve?
I expect to spend midnight this year in the exact same place I spent midnight last year: asleep in bed. That doesn’t mean I’ll let the holiday go by without recognition, though. Melinda and I love to use this time of year to reflect. How did the last twelve months go? And what do we hope to accomplish in the years ahead?
I was fortunate to travel the world this year. I got to meet some amazing people and see incredible innovations that I’m hopeful will make life better for millions. As December comes to a close, I feel more optimistic than ever about the progress we are making. At the same time, I’m also aware that gross inequities continue to separate the lucky from the unlucky all over the world—and that I have immense privileges as a result of this inequality.
Instead of updating you on what I’m working on—as I did in last year’s end-of-year post—I want to use this year’s post to write about inequality. Specifically, I want to focus on one particular issue that came to the forefront in 2019 and will be top of mind for many in 2020: America’s tax system. This isn’t exactly the most festive topic to cover during the holidays, but it’s one of the most important debates happening in our country right now.
Although I mostly spend my time talking about the issues I’m really focused on—global health, education, and climate change—I get asked about taxes a lot. I understand why it comes up so often; I’m a natural focal point for this debate.
The truth is, I’ve been pushing for a fairer tax system for years. It was nearly two decades ago that my dad and I started calling for an increase in the federal estate tax and for an estate tax in our home state of Washington, which has the most regressive tax system in the country. In 2010, he and I also backed a voter initiative that—had it passed—would’ve created a state income tax. (My dad even wrote a book about why we need to tax accumulated fortunes.)
It isn’t always popular to stand up for higher taxes, so it’s great that many Americans are having this conversation. I want to be as clear as possible about my views.
I start with the understanding that the U.S. government simply does not bring in enough money to meet its obligations. This isn’t a value judgment; it’s just a fact. The government collects about 20 percent of GDP in taxes while spending about 24 percent. And the cost of commitments is going up.
Meanwhile, the wealth gap is growing. The distance between top and bottom incomes in the United States is much greater than it was 50 years ago. A few people end up with a great deal—I’ve been disproportionately rewarded for the work I’ve done—while many others who work just as hard struggle to get by.
That’s why I’m for a tax system in which, if you have more money, you pay a higher percentage in taxes. And I think the rich should pay more than they currently do, and that includes Melinda and me.
Although I’m not an expert on the tax code, here are some steps I think America should take to make its tax system more fair.
We should shift more of the tax burden onto capital, including by raising the capital gains tax, probably to the same level as taxes on labor.
Today the U.S. government depends overwhelmingly on taxing labor—about three quarters of its revenue comes from taxes on wages and salaries. Most people get almost all of their income from salary and hourly work, which is taxed at a maximum of 37 percent. But the wealthiest generally get only a tiny percentage of their income from a salary; most of it comes from profits on investments, such as stock or real estate, taxed at 20 percent if they’re held for more than a year.
That’s the clearest evidence I’ve seen that the system isn’t fair. I don’t see any reason to favor wealth over work the way we do today.
I’m also in favor of raising the estate tax and closing the loopholes in it that many wealthy people take advantage of. A dynastic system where you can pass vast wealth along to your children is not good for anyone; the next generation doesn’t end up with the same incentive to work hard and contribute to the economy. It’s one of the many reasons that Melinda and I are giving almost all of our wealth back to society through our foundation, rather than passing all of it along to our children.
Other steps toward a fairer tax system include removing the cap on how much income is subject to Medicare taxes, closing the carried-interest loophole that allows investment-fund managers to pay the lower capital gains rate on their income, and taxing large fortunes that have been held for a long time (say, ten years or more). Very wealthy people often have large investments they’ve held for long periods, and if those investments aren’t sold or traded, the money is never taxed. That doesn’t make sense.
And fixing taxation at the federal level is only a part of the solution. We also need to make state and local taxes fairer, since they represent a large portion of Americans’ tax bills. For example, I still think we should adopt a state income tax in Washington.
When I say the government needs to raise more money, some people ask why Melinda and I don’t voluntarily pay more in taxes than the law requires. The answer is that simply leaving it up to people to give more than the government asks for is not a scalable solution. People pay taxes as an obligation of law and citizenship, not out of charity. Additional voluntary giving will never raise enough money for everything the government needs to do. If Melinda and I signed over our foundation’s entire endowment to the state of California, it wouldn’t be enough to fund their public schools for even one year. A vibrant economic system depends on setting expectations for who pays how much.
But in addition to fair taxes, Melinda and I think there’s value to society in allowing the wealthy to put some money into private foundations, because foundations play an irreplaceable role that’s distinct from what governments do well. In particular, philanthropy is good at managing high-risk projects that governments can’t take on and corporations won’t—for example, trying out new approaches to eradicating malaria, which is something our foundation is working on. If a government tries an idea for improving global health that fails, someone wasn’t doing their job. Whereas if we don’t try some ideas that fail, we’re not doing our jobs.
The country does need to be thoughtful about how high taxes should be raised. One of the reasons that innovators flock to the United States is that this country makes it easy to start a business, invest capital, and earn a profit. We shouldn’t destroy those incentives, but we’re a long way from that point now. Americans in the top 1 percent can afford to pay a lot more before they stop going to work or creating jobs. In the 1970s, when Paul Allen and I were starting Microsoft, marginal tax rates were almost twice the top rate today. It didn’t hurt our incentive to build a great company.
It’s great that Americans are debating who should pay more in taxes and how. I’ll continue to focus on the issues our foundation works on as well as climate change, so I will not take a position on the proposals that are being debated during this campaign season. But I believe we can make our system fairer without sacrificing the incentive to innovate. We’ve updated our tax system before to keep up with changing times, and we need to do it again, starting with raising taxes on people like me.
At the beginning of this post, I mentioned two questions Melinda and I like to reflect on this time of year: How did the last twelve months go? And what do we hope to accomplish in the years ahead? As we end this decade and look forward to what the 2020s will bring, I hope to see progress not only in how taxes are collected but how they’re spent to build a healthier, more equitable world for all.
Melinda and I believe that driving progress is wealth’s highest purpose. Even before we were married, we decided that we would use the resources from Microsoft to make people’s lives better. Our wealth comes with an obligation to give back to society, and in 2020, we’re committed to continue living up to that obligation: through our taxes, through our foundation, and through our personal giving.
Melinda and I are currently writing a lot more about that commitment in our Annual Letter, which will come out at the beginning of February.
I wish you and your loved ones a wonderful year ahead.
It’s a small world
What if everyone in the world lived on the same street?
I could spend hours exploring the website Dollar Street.

I’m obsessed with a website called Dollar Street. Created by Factfulness co-author Anna Rosling Rönnlund, Dollar Street imagines a world where everyone lives on the same street and the houses are ordered by income. The poorest live on one end, and the richest live on the other end.
Income can often tell you more about how people live than location can. Whenever I visit a new place, I look for clues about which income level local families live on. Are there power lines? What kind of roofs do the houses have? Are people riding bikes or walking from place to place?
The answers to these questions tell me a lot about the people there. If I see power lines, I know homes probably have electricity in this area—which means that kids have enough light to do their homework after the sun sets. If I see patchwork roofs, families likely sleep less during the rainy season because they’re wet and cold. If I see bikes, that tells me people don’t have to spend hours walking to get water every day.
The significance of income level is brilliantly illustrated by Dollar Street. Anna sent photographers to profile hundreds of homes from countries all over the world. You can sort these homes by income, location, or even household object (so for example you can have it show you just beds, or dish soap, or cooking utensils). Each house is meticulously tagged and includes a biography of the family that lives there. You can explore 135 objects belonging to each family, from their front door to the shoes they wear. The user interference is simple and intuitive to use.
Dollar Street really comes alive when you start comparing objects. I found the photos of toothbrushes to be particularly interesting. The families at the poorest end of the street use their fingers or sticks to clean their teeth. But once you reach a certain income level, everyone starts using a plastic toothbrush with bristles.
The more time you spend on Dollar Street, the clearer it becomes that all of us have the same basic wants and needs. People tend to spend money on the same things once they increase their income whether they live in China or Cameroon. At the end of the day, we all want a solid roof over our head, a more efficient way to get around, and better tools to take care of ourselves. It’s a beautiful reminder that we have more in common with people on the other side of the world than we think.
Anna and her team at Gapminder have managed to capture the most complete picture of humanity I’ve seen yet. I could spend hours exploring Dollar Street, and I hope you check it out.
Good code, big problems
Here’s one great way to use your tech skills
This technologist changed his career to help the poor.

These days I spend a lot of my time thinking about how technology can help the poorest people in the world improve their lives. It’s been a big focus for me since before Melinda and I launched our foundation. But looking back, I think I could have started down this path even sooner than I did.
People with a STEM background have a lot to offer the world of global health and development. That’s one of the reasons why I write about innovation so often here on TGN: I want to encourage software developers, inventors, and scientists to consider how they can use their skills to fight inequity. It’s deeply rewarding. You get the chance to learn from super-capable people—health care workers, farmers, political leaders—and work with them on tools that will empower them.
Last year I heard a talk from a young technologist who came to this realization sooner than I did. His name is William Wu, and he gave a fascinating demonstration at our foundation’s annual Goalkeepers meeting in New York City. Here are some highlights from his presentation:
After hearing William’s talk, I learned more about his story. He grew up in the Bay Area in the ’80s and ’90s. His parents helped him get excited about math and science from an early age. William studied engineering and computer science in college and grad school, ending up with a Ph.D. in electrical engineering from Stanford. While in grad school he met his future wife, Jiehua Chen (she goes by “JC”), who was getting a Ph.D. in statistics with a focus on global development.
After a short time writing code at various startups, William landed a job at NASA’s Jet Propulsion Laboratory, designing a telecommunications system for satellites including the International Space Station. It was fulfilling work—he had been obsessed with space since he was a kid—but eventually he realized he didn’t have to look to the stars for interesting problems to solve.
A turning point came when JC was working on soil analysis in Africa. The field team she was working with needed to convert thousands of data points on a spreadsheet into GPS coordinates, but they couldn’t figure out how to do it quickly. When JC mentioned the problem to William, he knew it could be solved with just a few lines of code. In minutes he had written a small program that did the job.
JC helped William see that someone with skills and interests like his could make a big difference in global development. In 2012, they founded their company, Quantitative Engineering Design, which develops software and hardware to improve farming and health care in developing countries. QED now employs about 20 engineers and scientists and works with national governments around the world as well as organizations like the Centers for Disease Control and Prevention.
The soil project that William describes in the video above is just one example of what QED is doing. They also built the data processing software used in Kenya by the CHAMPS project, an initiative that our foundation is funding to learn why so many young kids still die in some regions.
Another QED project involves digitizing medical forms. Throughout sub-Saharan Africa, health clinics use paper-based, handwritten medical registries. These registries contain a lot of (anonymous) data about how many patients come in and out of the clinic, the staff’s workload, the prevalence of different diseases, and so on. But because this is all done on paper, it’s hard to analyze the data for larger trends. QED is pilot-testing an app that would allow organizations to keep using paper-based books but quickly digitize the results. A health worker would use her mobile phone’s camera to scan the handwritten information, get it transcribed using optical character recognition, store it in the cloud, and export it for analysis, all in 60 seconds.
It’s too early to predict the impact of any of these projects. The point is that people with tech skills can find fascinating problems to work on and terrific partners to work with. It’s great if you decide to make a career of it, but you don’t necessarily have to. Sometimes all it takes to make a difference is the willingness to learn about a problem and use your talents to help solve it.
Our foundation maintains a list of sites that can point you to volunteer opportunities. It’s worth a look.

Talking dirt
Why I ♥ fertilizer
I visited a warehouse in Tanzania that was filled with a magical innovation that can lift millions out of poverty.

I’ve never been shy about my passion for fertilizer. It’s a magical innovation that’s responsible for saving millions of lives from hunger and lifting millions more out of poverty by boosting agricultural productivity.
So, you can imagine my delight when I recently stepped into a warehouse in Tanzania and got a glimpse of thousands of tons of fertilizer piled as high as snow drifts. The warehouse in Dar es Salaam is part of a new fertilizer distribution center, the largest of its kind in East Africa. Watching workers fill bags with the tiny white pellets containing nitrogen, phosphorous, and other plant nutrients was a powerful reminder of how every ounce of fertilizer has the potential to transform lives in Africa.
But that potential is only realized when it reaches the hands of the world’s poorest farmers—a challenge that’s proven difficult in Africa, where fertilizer use is very low, and, as a result, agricultural productivity is too. (Farmers’ yields in many parts of Africa are just a fifth of those of U.S. farmers.)
The warehouse I visited is one critical piece of the solution for improving both the supply and demand for fertilizer in Africa.
There are many reasons fertilizer use has not caught on in Africa. Cost is one of the biggest problems. Poor roads and other weak infrastructure make transporting fertilizer expensive, driving up its price for many African farmers by about 25 percent compared to their counterparts in other parts of the world. Then, there’s the issue of supply, which is not always dependable because of weak distribution systems in many parts of the continent. Limited access to credit prevents farmers from purchasing fertilizer even if it is available. And a lack of agricultural training means that farmers may not see the value of investing in it or understand how to use it properly.
So how can a warehouse solve these challenges? Let’s start with the warehouse itself. With room for 350,000 metric tons of fertilizer—in 2016, Tanzania used a total of 277,000 metric tons—the warehouse built by Yara, a Norwegian agricultural company, can hold an ample supply to prevent shortages.
At the same time, Yara is working with the government of Tanzania and dozens of other businesses and nonprofit organizations to stimulate demand for fertilizer by providing training to smallholder farmers on how to use it to boost crop yields.
Around 80 percent of Tanzania’s workforce is engaged in farming and related industries. Growing more food through greater fertilizer use would have a huge impact on the country’s prosperity.
What I saw at work in Tanzania is part of a broader effort underway in Africa to use agricultural as an engine to power economic growth across the continent. New innovations in farming—from better fertilizer and crops that are more productive, nutritious and drought and disease resistant—will make it possible for African farmers to increase their yields in the years ahead. With greater productivity, farming families will be able to sell their surpluses to supplement their family's diet with vegetables, eggs, milk, and meat.
We’ve seen the impact of helping farmers grow more food before with the “Green Revolution,” a historic transformation of agriculture in Latin America and South and Southeast Asia during the 1960s, which doubled food production and staved off widespread famine. The increase in agriculture production was made possible by improved seeds and fertilizer use.
As Africa experiences its own agricultural revolution, however, the world must be sure to learn from the past. One of the consequences of the Green Revolution was excessive fertilizer use, leading to water pollution and other environmental impacts. That’s why our foundation continues to work with partners to help train farmers how to apply fertilizer in the proper amounts that will increase yields while also promoting environmental sustainability. We’re also working on digital soil mapping and soil testing to provide farmers with valuable insights into how to improve the health of their soil so they can remain productive for generations to come.
My visit to the warehouse was a highlight of my trip to Tanzania. Just before wrapping up my tour, I paused briefly to watch workers stack bags of fertilizer onto flatbed trucks for their long journey to farms hundreds of miles away. It was exciting to think about the farmers who would use them and the positive impact the fertilizer would have on their next harvests and their country’s future.

Light meals
Tuning up photosynthesis to feed the world
Fixing flaws in photosynthesis could help boost productivity of our most important crops.

At some point in school, you probably learned about photosynthesis—how plants use energy from sunlight to convert carbon dioxide and water into food. This remarkable process is responsible for virtually all life on Earth, providing us with the energy we need and the oxygen we breathe.
But you might not have heard that photosynthesis has some flaws.
It turns out that plants are quite inefficient when it comes to using the sun’s energy. Just a fraction of the sunlight shining on a plant ends up fueling its growth, which means our crops are producing far less food than they could be.
An international group of researchers is aiming to fix that by giving photosynthesis a tune up. If successful, their research is expected to double the productivity of some of our most important crops—like rice, maize, cowpea, soybeans, and cassava.
That would be a much-needed breakthrough because the world is facing a crisis at the dinner table. With a growing population and changes in diets—like a greater demand for more meat as people earn higher incomes—we’ll need to produce 60 to 70 percent more food by 2050. At the same time, climate change is putting additional stresses on our food supply because of erratic rainfall, severe droughts, and the spread of pests and crop diseases.
Those who are at greatest risk of hunger in the years ahead are the world’s poorest people. They live in regions with high population growth and often rely on farming both to feed their families and to earn an income.
No single solution will solve this global food crisis. We’ll need to develop innovations in all areas of agriculture to increase productivity. Improved seed varieties for crops that are resistant to drought, flood, pests, and disease. Better data to help farmers manage their crops and livestock more efficiently. And some game-changing discoveries that will lead to bigger harvests.
That’s why our foundation along with the U.S. Foundation for Food and Agriculture Research and the U.K. Government's Department for International Development is investing in the global effort to make photosynthesis more efficient. This research program, known as Realizing Increased Photosynthetic Efficiency or RIPE, is being led by the University of Illinois.
RIPE scientists began their research by modeling the entire 170-step chemical process of turning sunlight into energy. Using computer simulations, they explored which changes might lead to the biggest increases in productivity—in the same way an efficiency expert might make improvements to a car production line to maximize output.
One promising area of research involves making plants absorb sunlight more effectively. While light is essential for a plant’s survival, too much high-intensity light can cause damage to the plant. To protect themselves, plants have developed mechanisms to siphon off some of the sun’s energy as heat when they are in direct sunlight. But this creates a problem when the sun goes behind a cloud and the plant is in the shade. The plant’s protective mechanism doesn’t adjust quickly to the reduced light, inhibiting the process of photosynthesis for minutes or sometimes hours. RIPE researchers discovered a way to speed up this transition, allowing the plant to continue with photosynthesis even with light fluctuations.

Another critical area of research involves an enzyme known as Rubisco, which captures carbon dioxide and turns it into sugars for the plant. Some researchers are working to speed up Rubisco activity in the plant, which would result in higher crop productivity.
Other researchers are trying to fix an inefficiency created by Rubisco: It has a hard time distinguishing carbon dioxide from oxygen. So, about 20 percent of the time Rubisco accidently grabs an oxygen molecule instead of a carbon dioxide molecule. This results in the creation of a compound that must be recycled by the plant through a process known as photorespiration. Photorespiration is long and complicated, costing a plant energy and resources that it could use for growth. To solve this, researchers have engineered an alternative pathway to drastically shorten the photorespiration process and save energy. When tested in the lab, this fix boosted plant growth by up to 40 percent.
Much of the field testing of these improvements to photosynthesis has been done using tobacco plants. While tobacco plants are not food crops, they are a convenient proof-of-concept crop because they are easy to transform genetically and they produce a large amount of seed, shortening testing cycles. In the next phase of research, scientists are working to transfer these new genetic traits to food crops, including cowpea, cassava, and soybeans.
Still, these high yielding crops are years away from being grown on farms around the world. And they would need to pass safety tests to gain consumer acceptance. I’m excited about the progress made by the RIPE team and I look forward to hearing more about their discoveries in the future.

A fruitful partnership
How I cemented my friendship with Aliko Dangote
My friend Aliko Dangote and I are working together to fight malnutrition.

Have you ever met someone new and immediately felt like you could talk to them for hours?
That happened the first time I met Aliko Dangote. A couple years ago, he and I ended up going to the same event in New York. A mutual friend suggested that I meet him because he knew we were both super interested in global health. So we made sure to sit next to each other at dinner.
As soon as we shook hands, it was clear we had a ton in common. We both started successful businesses in the late 1970s. For our second act in life, we both chose to start foundations aimed at improving health and education. (Today, the Dangote Foundation is the largest such organization in sub-Saharan Africa.)
More importantly, we both love to geek out over things that make some people’s eyes glaze over, like cement, fertilizer, and iodized salt. Check out this video of Aliko’s recent visit to our foundation’s office in Seattle for proof:
That first meeting sparked the beginning of a fruitful friendship. In 2016, our foundations announced a joint, five-year $100 million commitment to reducing malnutrition in Nigeria.
Malnutrition is the greatest health inequity in the world. It’s responsible for nearly half of all under 5 deaths in Nigeria (and around the world). Even if you survive to adulthood, your chances of dying are much higher, and your quality of life is greatly reduced.
One of the ways our foundations are working together to fight malnutrition is through food fortification. Kids often become malnourished when they don’t get enough micronutrients—vitamins and minerals—to digest their food properly. One way to correct this is by adding micronutrients to the food that families—especially those from low-income households—are purchasing every day.
When you go to a grocery store in the U.S., a lot of food already has this fortification. Think iodized salt, or milk that comes with extra vitamin D and calcium. By introducing additional micronutrients to the food people are already eating, you can improve health without changing any habits. Our foundations are now working together to find other staple foods and condiments that could be used to deliver more micronutrients to more people in Nigeria, like fortified bouillon cubes.
Improving health in Nigeria is critical to making progress in sub-Saharan Africa. The country is home to nearly a quarter of all people living in sub-Saharan Africa, and that population is only going to grow in the future. By solving problems in Nigeria, you can have a huge impact on all of Africa.
Aliko Dangote understands this, and that’s why he’s committed to making progress in his home country. Melinda and I are lucky to have him as a partner (and friend!) in improving health.

Tipping point
Finding my voice in the fight against malaria
Meet a young Nigerian who has battled malaria as a patient, a doctor, and now as a Goalkeeper.

Dr. Elvis Eze, 28, grew up in Nigeria battling malaria both as a patient and as a physician working in a Lagos hospital. He now serves as a Youth Ambassador for Malaria No More UK, helping to mobilize funding and support to bring an end to malaria in his lifetime. Eliminating malaria is one of the Global Goals that will be discussed at this year’s Goalkeepers event. I had the privilege of meeting Dr. Eze at last year’s Malaria Summit in London. I invited Dr. Eze to share his inspiring story as one example of the many dedicated people in the world who are helping the world achieve the Global Goals. – Bill Gates
I remember growing up in Nigeria with fond nostalgia. I lived with my parents and four siblings in a middle-class Lagos neighborhood. Our days were filled with street football, video games, and card games.
What was there not to love?
Looking back, there was one thing that frightened all of us: malaria.
The mosquito-borne disease was always striking someone close to me, or sometimes even me. The fatigue, muscle aches, burning fever, and the lost play days and school days were my biggest worry as a child.
I still wonder about my childhood friend, Lukman, who was ill with malaria one day and never came back to our school. Were his parents forced to pull him from our school because of his mounting medical bills? Or, was he one of the tens of thousands of young children who lose their lives to malaria in Nigeria every year?
My experience with malaria is hardly unique. Worldwide, there are about 200 million cases recorded every year. The World Health Organization estimates that a child dies from malaria every two minutes. Nigeria alone accounts for 25 percent of the world’s malaria cases. In fact, the disease is such a regular occurrence in my country that people speak about it the same way the weather is talked about in London or the flu in the winter months. It is just an accepted part of life—and for many, an accepted cause of death.
It wasn’t until years later, when I became a doctor, that I realized that none of us needed to accept malaria as a matter of fate. We could do much more to fight it.
In 2014, I was working as a junior doctor in the emergency room in Lagos, where we regularly treated children suffering from malaria. One night, the hospital was overcrowded mostly with malaria cases. I can still remember seeing the children going through bouts of seizures, losing consciousness, and, at times, dying. I also recall the helplessness on the faces of their parents as they lived out their worst nightmare.
This was my tipping point. At the end of this one painfully long night shift, my mind was clouded with anger, sorrow, and loss. And yet, at that moment, I was thinking clearly about one thing: I needed to take action against malaria.
There was no reason for children to be experiencing the suffering I was witnessing in the emergency room. Malaria is a preventable and treatable disease. I had experienced firsthand how it was possible to administer life-saving treatments to children and give them their childhood back. Still, malaria is killing 435,000 people worldwide every year, most of them children. As a doctor, I knew I could continue to treat malaria patients in my care and advise families how to use bed nets and other prevention techniques. But I also wanted to use my voice to raise awareness of the disease and mobilize more resources in the global fight against it.
That opportunity came in 2015, when I was invited to the United Kingdom to work as a health officer for the Commonwealth Secretariat. I helped establish the Commonwealth Youth Health Network, a platform for young people to advocate and engage on health-related global issues, including the Global Goals. As a member of the network, I learned how Sri Lanka, which was one of the most malaria-infested countries in the world, had been able to eliminate the disease in 2016. Sri Lanka’s achievement was a powerful reminder that progress against malaria is possible.
In 2018, I participated in the Malaria Summit in London, where I shared my story and joined the call for heads of government to end malaria. All 53 countries of the Commonwealth made the bold commitment to halve malaria in their countries by 2023, which would prevent 350 million malaria cases and save 650,000 lives.
One lesson I’ve learned from my experience is how my voice could be a powerful tool to influence change in the fight against malaria. And your voice can be, too. I’d like to invite you to speak up as part of the Malaria Must Die campaign and record your voice for the world’s first voice petition to end malaria. Our goal is to help the Global Fund to Fight AIDS, Tuberculosis and Malaria, which finances over half of all malaria efforts worldwide, get fully funded for its vital work.
When I became a doctor, I took the Hippocratic oath, like all doctors before me. It’s an oath I think about often as I seek to provide all my patients with the highest quality of life possible. I’ll be reminded of this oath again this week when I attend this year’s Goalkeepers event, which will focus on efforts to accelerate progress on the Global Goals. Much like my oath as a doctor, the Global Goals are a promise by the world to save and improve the lives of our fellow citizens of the world. With your help, I know it will be a promise the world can keep.
Phones and Farms
Why the future is bright for the world’s poorest farmers
Technology is transforming agriculture and the fight against poverty.

I have probably learned more about farming in Africa from Sam Dryden than from any other person. Sam has spent decades working in agriculture, including a stint at the Gates Foundation, and he is passionate about improving the lives of the poorest. So when he asked me to contribute to a series of articles in Foreign Affairs on the future of farming and its role in fighting poverty, I was happy to do it. My essay is below.
One thing I’ve learned in my work with Microsoft is that the process of innovation tends to take longer than many people expect, but it also tends to be more revolutionary than they imagine. We are seeing this dynamic play out right now in the way digital technology is fundamentally reorganizing life for the poorest people in the world.
Twenty years ago, when the Internet was brand new, a lot of people thought computers would quickly become part of daily life in developing countries. And when I say “a lot of people,” I include myself. But those people weren’t thinking about all the facts.
In 1997, I traveled to South Africa for the first time. I spent most of my time in big office buildings in downtown Johannesburg. One day, though, I took a side trip to Soweto, where Microsoft was donating computers and software to a community center—the same kind of thing we did in the United States.
But it became clear to me very quickly that Soweto was not like the United States. I had seen statistics on poverty, and I had seen a lot of poor communities, but this was the first time I had ever really seen true poverty. I was struck by what I didn’t see. No electricity. No running water. No toilets. No roads.
The community center had no consistent source of power, so they had rigged up an extension cord that ran about 200 feet from the center to a diesel generator outside. Looking at the setup, I knew right away that the minute I left, the generator would get moved to a more urgent task, and the people who used the community center would go back to worrying about challenges that couldn't be solved by a PC.
When I gave my prepared remarks to the press, I said: “Soweto is a milestone. There are major decisions ahead about whether technology will leave the developing world behind. This is to close the gap.”
But as I was reading those words, I knew there was much more to the story. What I didn't say was: “By the way, we're not focused on the fact that three quarters of the people in this region are eking out a living on tiny farms that don’t produce enough food. But we're sure going to bring you computers.”
In the past 20 years, however, digital technology has gradually insinuated itself into poor people’s lives in ways I never could have predicted. For example, about two-thirds of Africans now have mobile phones, and pretty soon cellular coverage will be more or less universal. The power of a phone in every pocket is turning out to be extremely disruptive in exciting ways—and the poor finally have a chance to use technology in ways that solve the real problems they face in their lives.
CELL PHONES AND THE FINANCIAL SERVICES REVOLUTION
Mobile phones have recreated the economics of providing financial services to the poor. In an analog era when banking required buildings, piles of paperwork, security guards, and tellers, the cost per transaction was high enough that no company could even conceive of profiting by serving poor people who transacted in tiny amounts. As a result, the poor led their financial lives informally, paying exorbitant amounts in fees and interest to borrow, save, and send money.
But phones get rid of all that expensive infrastructure. Transaction costs are so low that companies can make money by serving the poor. And in the process of competing for poor people’s business, these companies will develop new financial products that meet poor people’s unique needs. One example is a new company called M-KOPA, which lets 250,000 customers in three African countries pay for solar electricity (instead of kerosene) in small daily installments through their cell phones. In short, digital financial services can create one thriving formal economy that includes everyone.
In fact, since developing countries aren’t stuck with a legacy analog banking system, I believe that for the foreseeable future the boldest ideas in financial services will be coming from upstart companies in poor places instead of the big companies we’ve all heard of.
DIGITAL AGRICULTURE
If there is another example of a market that simply does not work for the poor, it’s agriculture. But digital technology can change that, too.
Right now, hundreds of millions of Africans rely on farming for a living, but they don’t grow as much—and they don’t sell as much of their surplus—as they could. As a result, Africa had to import $40 billion worth of food last year. Something is not functioning properly when half of the continent’s labor produces food, and the continent still buys its food from somewhere else!
So what is going wrong? Why aren’t African smallholders tapping into that $40 billion market?
The main problem stems from the fact that agricultural markets, like banks, exist on a formal plane, whereas smallholders exist on an informal one. So farmers and markets cannot communicate effectively. Smallholders don’t know what the market will pay. They can’t grow crops according to the market’s specifications because they don’t know the specifications. They have no way to learn the farm-management practices that would let them double or even triple their yields. Instead, they grow mostly what they can eat or trade locally, the way they’ve always grown it.
As long as this information disconnect exists, there will be a related physical disconnect. The rails and roads that would take crops from the farm gate to the market don’t exist, because the market doesn’t want the crops the farmers are growing in the ways and volumes they’re growing them. So farmers are isolated, stuck with no money and no voice that the marketplace can hear.
But digital technology can act almost like a secret decoder ring that links the formal and informal sectors. Smallholders are already using mobile phones to communicate within their networks, to talk to family and friends. The institutions that make up the formal marketplace communicate in much the same way. So it is now possible to generate a two-way conversation between Africa’s producers and Africa’s consumers—and this is an entirely new conversation. Each party will be able to express its needs to the other for the first time ever.
Imagine a smallholder farmer who can discover, easily, that yams are expected to fetch a high price this year. She can also contact a local cooperative to combine her yams with those of her neighbor, satisfying the buyers’ volume requirements. Because she is assured of sale at harvest, she can afford to take out a loan, using her phone, to buy fertilizer or better storage or whatever else she needs to maximize her yield. In the meantime, instead of waiting for a visit from an extension worker who may or may not know about yams and the soil in this particular region, she can get advice tailored by crop and soil type via digital video or text.
When information can flow easily, when data is democratized, the cost of doing business in agriculture goes way down, just as transaction costs go way down when financial transactions are digital. The excessive time and money farmers, agribusinesses, and cooperatives spend managing the risk of doing business with unknown partners is a drag on efficiency. When these partners can know each other easily—can function as nodes in a single marketplace—agriculture will thrive.
It’s not as easy as the above paragraphs may make it seem. Building a digital agriculture system that actually accomplishes these goals will take innovation and investment. But the point is that before it wasn’t possible, and now it is. The added variable of digital technology has changed the agricultural development equation.
OTHER DIGITAL APPLICATIONS FOR AGRICULTURE
While mobile phone technology—and the way it can collapse the formal and the informal—is perhaps the most revolutionary of the digital opportunities in agriculture, there are many others.
Take seeds. Advances in genomics are fundamentally changing the way breeders do their work. It took researchers 13 years to sequence the human genome. Now they can do it in 27 hours. The cost of sequencing a genome has been reduced more than 10-fold in the past five years.
Cassava is a powerful example of what breeding—powered by the revolution in genomics—can do. It’s hard to breed cassava, and every breeding cycle takes five years, which means it usually takes a full decade to release a new variety.
But scientists can now use computer algorithms to link sequence data from the cassava genome to the performance of cassava plants in the field. This technique was first developed to predict levels of milk production in cows.
Breeders in developing countries will be able to predict how a tiny cassava seedling will perform. Consequently, the breeding cycle can be shortened from five years to two years. And it’s not just a shorter cycle. It’s also higher-quality, because breeders can focus on the most desirable traits early in the process. This will also allow for more participatory breeding, a process in which farmers themselves have input into the development of the new varieties they’ll be growing.
The digital revolution also provides opportunities to collect better data. In an age when a satellite can determine instantly how much wheat is in a field, it is a shame that we ask countries to use limited resources to send enumerators around with pen, paper, and tape measure. What we get is a lot of wasted time and inaccurate or incomplete data. The digital revolution can improve the quality of critical data while freeing up people to do other high-impact work.
CONCLUSION
I still can’t predict precisely how—or when—these changes will take hold. The beauty of innovation is that once the technology and tools are widely available, people with every possible insight and point of view start working on solutions to problems others can’t even see. Ultimately, it’s the way human beings, with our vast stores of ingenuity, deploy the power of the technology and tools that makes the biggest difference.

Meet the X-shredder
Test-tube mosquitoes might help us beat malaria
Genetic editing might help us wipe out the disease.

It’s Mosquito Week again on the Gates Notes. This year I’m exploring some of the science behind malaria and other mosquito-borne diseases. You can read below about how gene editing could play a key role in eradicating malaria. I’ve also written about amazing advances in tracking the disease and how the parasite is a deadly shapeshifter.
Humans have spent thousands of years inventing new ways to kill mosquitoes. The Romans did it by draining swamps. Today you might have a bug zapper in your back yard. In low- and middle-income countries, it’s common to see people spraying insecticides or setting up sticky traps baited with sugar.
But evolution is smart. It is one-upping us by creating mosquitoes that are harder to kill. In sub-Saharan Africa and parts of South America and southeast Asia, we are seeing an alarming number of mosquitoes that can withstand insecticides.
This is especially problematic for the fight against mosquito-borne diseases like malaria. To eradicate these diseases, we need new tools to complement the ones we already have.
Our foundation is backing a lot of different advances. One that I’m especially excited about is a set of techniques for genetically modifying mosquitoes that could dramatically reduce the number of disease-carrying insects in certain areas.
What is cool about these genetic techniques is how precise they can be. Precision matters because out of more than 3,000 species of mosquitoes, only five are responsible for causing most cases of malaria. Of those, only females spread the disease, because they’re the only ones that bite humans. (They do it when they need extra protein for reproduction. Experts call it “taking a blood meal.”) The males just drink nectar.
The promise of gene editing is that, instead of killing a bunch of mosquitoes indiscriminately, we could eliminate only the dangerous ones in a particular area. That would buy us time to cure all the people there of malaria. Then we could let the mosquito population return without the parasite.
One exciting gene-editing technique is called gene drive. The term covers several different approaches, but the basic idea is to use the CRISPR method to rewrite the usual rules of inheritance. Normally, for any given gene, there’s a 50 percent chance that a parent with that gene will pass it on to a child. (It is competing with one from the other parent, and only one of the two can win.) With gene drive, the odds go up to 100 percent. You give a few mosquitoes an edited gene that inserts—or drives—itself into all their offspring. When those mosquitoes mate with wild mosquitoes, all their children will have the edited gene, and over time it will make its way through the entire population.
Imagine if blue-eyed mosquitoes had only blue-eyed children, no matter what color their partners’ eyes were. Eventually, every mosquito in that population would have blue eyes.
This chart shows you how gene drive eventually spreads a gene throughout an entire population:
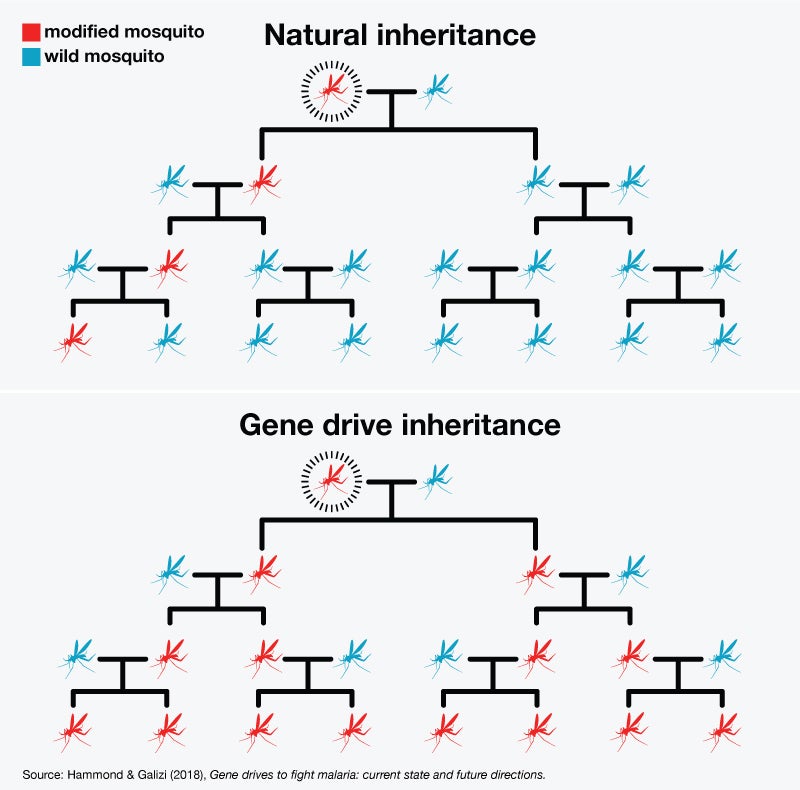
There’s no reason to think gene drive is even feasible in humans, let alone advisable. There are also serious questions surrounding the use of this technology on insects, which I will get to in a moment. But first I want to give you two examples of how it works.
One is the colorfully named X-shredder. As you might remember from biology class, the sex of a mosquito is determined partly by the sex chromosomes it inherits from its parents. Females got one X chromosome from each parent; males got an X from their mother and a Y from their father.
In 2014, scientists at Imperial College London and the Fred Hutchinson center here in Seattle were able to edit a protein in male mosquitoes so that it shreds the X chromosomes in their sperm. As a result, the males pass along mostly Y chromosomes, so most of their offspring will be males. Thanks to gene drive, those offspring will also have the edited protein, so most of their children will be males.
Within a few generations, the male/female ratio gets out of whack, and eventually the species dies off in that area.
Another example involves the doublesex gene, which in mosquitoes works along with the sex chromosome to determine whether an insect turns out male or female. Last year, researchers at Imperial College London found that females with edited doublesex genes develop a mix of male and female organs, including male genitalia and a proboscis that is too flimsy to break human skin. They can’t reproduce, so the population shrinks; and they can’t take a blood meal, so they won’t spread the parasite.
The doublesex edit doesn’t affect males, although thanks to gene drive, they will pass it to their offspring, which is how it keeps spreading through the population.
We know gene-drive technology works in the lab. When the Imperial College researchers put 150 males carrying a copy of the doublesex edit in a small cage with 450 wild-type mosquitoes, the population died off within a few months (about 10 generations). The sex bias edit produced similar results.
The next step is to run tests in larger cages and, eventually, get permission from governments to do them outdoors. We need to understand things like: What’s the impact on the food chain if a certain species of mosquito starts dying off? How many altered insects would we need to introduce? How long do we need the mosquitoes to be gone? Last year, the government of Burkina-Faso agreed to allow the release of sterile, non-gene-drive mosquitoes in the wild so researchers could begin to study some of these questions.
As I mentioned, social and regulatory issues also come into play. For example, because mosquitoes don’t exactly respect national boundaries, neighboring countries will probably need to agree on the rules surrounding the use of gene-editing technology. Policymakers and scientists have been debating these questions in forums like the World Health Organization and the African Union’s development agency, and they are moving toward a consensus.
I think we can have the regulatory approvals in place by 2024 and the first gene-drive mosquitoes ready for use by 2026. Although this technique will never replace the other tools we have for fighting malaria, I’m optimistic that it could become one more important weapon in eradicating the disease.
Captain Kirk vs. malaria
The world’s deadliest shapeshifter
The malaria parasite is good at fooling your immune system. Now scientists are fighting back.

It’s Mosquito Week again on the Gates Notes. In this post I write about how the malaria parasite changes shape to foil your immune system. I’ve also written about ingenious new genetic techniques for fighting mosquitoes and maps that could help us defeat malaria.
I remember an old episode of the original Star Trek where the bad guy is a shapeshifter who turns himself into a second Captain Kirk. There’s a great scene at the end where Spock has to figure out which one is the impostor.
Shapeshifters are not just the stuff of science fiction, though. We have them right here on earth. Some are innocuous, like a caterpillar turning into a butterfly. But there’s another shapeshifter that’s responsible for more than 400,000 deaths every year. I’m talking about the group of microscopic parasites that cause malaria.
Malaria is one of the most fascinating and frustrating diseases our foundation works on, and its ability to change shape is one of the main reasons why. These parasites have figured out ingenious ways to fool your immune system. They have also (mostly) evaded our best efforts to make a malaria vaccine.
To understand how, it helps to know a bit about how your immune system works.
Your system is very good at detecting unusual objects in your body. It looks at the proteins on the surface of an invader and says, “I’ve never seen the funny shape on the outside of this thing. I’m going to attack it.” After the invader is defeated, your body remembers what it looked like and will go after it if it ever shows up again. Vaccines work by taking advantage of this process. When you get a measles shot, it contains a little bit of the virus; it won’t make you sick, but your body learns how to defend itself against future infections.
Unfortunately, malaria is a lot more complex than viruses or bacteria. For one thing, it is caused by parasites. Parasites don’t look as weird to your body as viruses or bacteria do. In fact, they more closely resemble your own cells, so your immune system has a harder time fighting them off.
Another problem is that the malaria parasite goes through three different stages in your body. It looks radically different in each stage, and as the infection goes on, you have all three going on at once.
Stage 1 begins when an infected mosquito bites you and injects a little saliva under your skin. This dose of saliva might contain only 100 parasites (called sporozoites in this stage). They are small and don’t cause any inflammation in your body, so your immune system doesn’t bother to look for them. You’re not feeling any symptoms yet.
Within an hour or two, the sporozoites make their way to your liver for stage 2. Coming out of your liver, they take a new form (called merozoites) and start invading your red blood cells. This invasion causes the symptoms—fever, chills, and so on—that make malaria such a miserable and deadly disease.
Now your body knows it’s sick and your immune system kicks in. But this is where the parasite’s shapeshifting comes into play.
Remember how the measles vaccine helps your immune system learn to identify the virus by looking for certain proteins on its surface? That works because those proteins look the same on each clone of the measles virus in your body. With malaria, each one can present up to 60 different proteins—and thanks to a mechanism that tells the parasite to alter its surface periodically, they shuffle these proteins around in different combinations every few days.
As a result, by the time your immune system has figured out how to attack one shape, the parasite has transformed, and your body’s defenses are useless. Your immune system adjusts, but not before the parasite has shifted again. It’s as if there’s a door on the surface of the parasite, but it keeps changing the locks so your body never has the right key.
Finally, in stage 3, a few of the merozoites develop into male and female cells. These hang out in your bloodstream, waiting for the next mosquito to come bite you. Once they’re in the mosquito’s stomach, they form new sporozoites, which make their way to the bug’s saliva glands and get injected into the next human, where the cycle starts all over again.
So that is the life cycle of malaria. What does all this mean for the effort to control and eventually eradicate this disease?
You might think we could create a vaccine that simply recognizes all the different shapes of the parasite. Unfortunately, that’s not practical. The only vaccine we have ever done that with is for a type of pneumonia. It is very expensive to manufacture and covers only a dozen shapes or so, versus the 60 shapes in one malaria infection and the many hundreds across all malaria parasites worldwide.
The malaria community (including our foundation) has been working for years on a vaccine to protect you in stage 1, before the infection takes hold. This vaccine, called RTS,S, teaches your immune system to hunt for a bit of protein that is always on the surface of the parasite. Unfortunately, the protection provided by RTS,S is not strong enough for long enough to help us make real headway toward eradication. And there are other forms of protection (such as bednets and insecticides) that are more cost-effective for saving lives.
People often ask me if it’s frustrating to fund work that takes so long to come to fruition. My answer is: not at all. Of course, I’m disappointed that we don’t have a long-lasting vaccine yet. But this is hard work. Parasites are such complex organisms that there are no effective vaccines for any of the human diseases that they cause. Besides, the research on RTS,S has given scientists a lot of insight into how malaria works and new clues about how to stop it. In fact, much of what we know about how your body responds (or fails to respond) to this type of parasite came from research on RTS,S.
The malaria community is now building on this knowledge. For example, scientists are working on new approaches that we hope will trigger the immune system to create long-lived, antibody-generating cells. Another promising idea is to create synthetic antibodies rather than trying to get your immune system to make natural ones. These monoclonal antibodies have revolutionized the treatment of cancer and inflammatory disease, and they could do the same for infectious diseases like malaria.
Knowing how complex malaria is helps me appreciate how much progress the world has made in fighting it. Deaths from malaria have dropped 42 percent since 2000, thanks to investments in bednets that prevent it and medicines that cure it. When I see how far we have come and how much we have learned, I am as optimistic as ever that we can beat this clever shapeshifter.

Disease atlas
These maps could point the way to stopping malaria
We’re using them to maximize scarce resources.

It’s Mosquito Week again on the Gates Notes. This year I’m exploring some of the science behind malaria and other mosquito-borne diseases. You can read below about how maps are revolutionizing the fight against malaria. I’ve also written about how the malaria parasite is a clever shapeshifter and how genetically editing mosquitoes could help us defeat the disease.
Imagine calling the fire department and telling them: “There’s a house burning somewhere in the city!” They ask you for the address or at least some nearby streets, but you’re not sure. Without more specifics, it’s just about impossible for them to help.
For decades, the malaria community has faced a similar problem, but on a national scale. In many of the countries with a lot of malaria, we have had a national estimate of how prevalent it is, but very little reliable information about the breakdown within the country. That means health officials have to distribute bednets across an entire region, hoping to get everyone who might be at risk while also covering people who aren’t.
This problem is especially urgent now. After more than 15 years of steady progress against the disease, the improvement is slowing down. Funding for malaria has also flatlined. If we simply stick with the same tools and the same strategies, progress will stall, and the disease might make a comeback. We need to do more with what we have.
I am happy to report that things are changing, thanks to better data. A combination of new technology and improved systems is helping us target lifesaving interventions in the places where there’s the greatest risk of malaria—making sure that each dollar spent has the biggest possible impact.
I admit that data isn’t as sexy as shapeshifters or the X-shredder. Yet the topic is super-important. It is a big focus for our foundation’s malaria strategy, one of the key things we bring to the table given our interest in technology and innovation. This post will get more in-the-weeds than I usually do on TGN, but if you are as obsessed with malaria as I am, I hope you’ll find it interesting.
Health experts estimate the burden of disease in two ways. One is to use anonymous information collected by health workers. But this information has a lot of gaps and gets aggregated as it moves up the chain from the clinic to the district to the province. This would be roughly equivalent to adding up the cases in every hospital in a U.S. state and only reporting the total. It obscures a ton of local variation, and by the time all the data is processed, the report may be a year out of date.
The other source is surveys. Health workers go out to a community and test a few volunteers for malaria, then repeat this at sites across the country. But this process is expensive and time-consuming, which limits the number of samples a country can take and how often it can take them.
The malaria community is tackling the problem in two ways. A nonprofit called the Malaria Atlas Project (funded by our foundation) started by gathering all the data they could find from every endemic country. They discovered something surprising: Although there were big gaps on the map where we had very little information, overall there was a lot more data than anyone expected.
Using the information they had, along with data on local conditions that affect the spread of malaria (such as the temperature, humidity, and the location of health clinics), MAP started building computer models that give us a much clearer picture of what’s going on.
The results are remarkable. We now have data-rich maps with pixels that are just 5 km square. Instead of blanketing entire regions with bednets and other anti-malaria measures, health officials can target efforts where they will do the most good.
Now comes the next step: getting even better data so we make maps with an even higher resolution. To accomplish this, our foundation and other partners are helping countries strengthen their systems for monitoring disease. In the poorest places, this might mean disaggregating their data and making sure it is accurate and timely. For others, it means equipping health workers with mobile phones or tablets so they can enter the information digitally. More than 60 countries already use the same software to report health data, vastly simplifying the process of collecting and analyzing information.
Below you can see a dramatic example of what the future of mapping looks like. Both are maps of Haiti. The one on the left uses the 5x5 km resolution, built with aggregated data. (Remember, this was already a huge leap forward from national estimates.) The one on the right uses data from individual health facilities to create pixels that are just 1x1 km square. See how much more detailed it is? When you need to maximize scarce resources, this kind of information is invaluable.
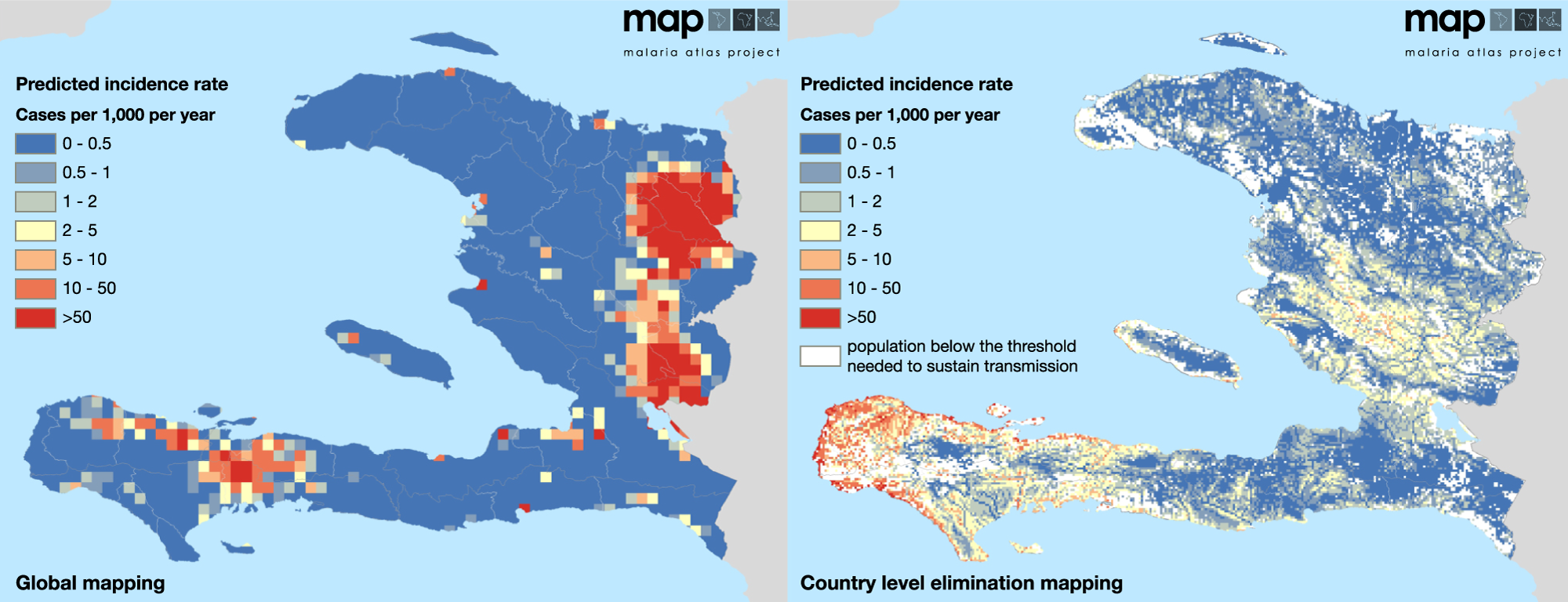
There is more to come. One promising approach uses genetic analysis of the malaria parasite to make the maps even more robust, for example revealing how the disease is transmitted from place to place.
Genetic data is also helping us identify insecticide-resistant mosquitoes and drug-resistant forms of the disease. In Vietnam, health officials recently noticed an alarming spike of cases in one region of the country. Then genetic analysis of the parasite in that region revealed that they were fighting a drug-resistant strain of malaria. They quickly switched to a more effective drug and expect to see the number of cases drop soon.
This kind of work is best done at the local level. So we’re funding programs that help scientists in developing countries do more of this analysis themselves, rather than sending samples off to a lab in the U.S. or Europe. Increasingly, scientists in Senegal, Thailand, and other countries are doing their own analysis, which both speeds up the process and puts local experts in the leading role where they belong.
There is a lot of innovation in the malaria field right now, including work on vaccines and other parasite-killers and a way to fight the disease using test-tube mosquitoes. Better data and malaria maps will help us put all these breakthroughs to their best use, and bring us closer to the day when this disease is gone forever.

Quality of life
What the plow and lab-grown meat tell us about innovation
I was honored to guest curate MIT Technology Review’s 2019 breakthrough technology issue.

I’m a big fan of the MIT Technology Review’s annual list of ten breakthrough technologies—so when they asked me to choose this year’s list, I jumped at the chance. It’s been a lot of fun working on the issue and picking which innovations to include. I think all ten entries will have a significant impact in the years to come, and I’m excited for you to learn more about them.
Here’s the opening essay I wrote for the issue. You can see the full list of breakthrough technologies here.
I was honored when MIT Technology Review invited me to be the first guest curator of its 10 Breakthrough Technologies. Narrowing down the list was difficult. I wanted to choose things that will not only create headlines in 2019 but captured this moment in technological history—which got me thinking how innovation has evolved over time.
My mind went to—of all things—the plow. The plow is an excellent embodiment of the history of innovation. Humans have been using them since 4000 BCE when Mesopotamian farmers used sharpened sticks to aerate soil. We’ve been slowly tinkering with and improving them ever since, and today’s plows are technological marvels.
But what exactly is the purpose of a plow? It’s a tool that creates more: more seeds planted, more crops harvested, more food to go around. In places where nutrition is hard to come by, it’s no exaggeration to say that a plow gives more years of life to people. The plow—like many technologies, both ancient and modern—is about creating more of something and doing it more efficiently, so that more people can benefit.
Contrast that with lab-grown meat, one of the innovations I picked for this year’s TR10 list. Growing animal protein in a lab isn’t about feeding more people. There’s enough livestock to feed the world already, even as demand for meat goes up. Next-generation protein isn’t about creating more—it’s about making meat better. It lets us provide for a growing and wealthier world without contributing to deforestation or emitting methane. It also allows us to enjoy hamburgers without killing any animals.
Put another way, the plow improves our quantity of life, and lab-grown meat improves our quality of life. For most of human history, we’ve put most of our innovative capacity into the former. And our efforts have paid off: worldwide life expectancy jumped from 34 years in 1913, to 60 in 1973, and has reached 71 today.
Because we’re living longer, our focus is starting to shift toward well-being. This transformation is happening slowly. If you divide scientific breakthroughs into these two categories—things that improve quantity of life versus quality of life—the TR10 list from 2009 looks not so different from this year’s. Like most forms of progress, the change is so gradual that it’s hard to perceive. It’s a matter of decades, not years—and I believe we’re only at the midpoint of the transition.
To be clear, I don’t think humanity will stop trying to extend lifespans anytime soon. We’re still far from a world where everyone everywhere lives to old age in perfect health, and it’s going to take a lot of innovation to get us there. Plus, “quantity of life” and “quality of life” are not mutually exclusive ideas. A malaria vaccine would both save lives and make life better for children who might have otherwise been left with developmental delays from the disease.
We’ve reached a point where we’re tackling both ideas at once, and that’s what makes this moment in history so interesting. If I had to predict what the TR10 will look like a few years from now, I bet technologies that alleviate chronic disease will be a big theme. This won’t just include new drugs (although I would love to see new treatments for diseases like Alzheimer’s on the list). These innovations might look like a mechanical glove that helps a person with arthritis maintain flexibility or an app that connects someone experiencing a major depressive episode with the help they need.
If we could look even further out—let’s say the TR10 list 20 years from now—I would hope to see technologies that center almost entirely on well-being. I think the brilliant minds of the future will focus on more metaphysical questions: How do we make people happier? How do we create meaningful connections? How do we help everyone live a fulfilling life?
I would love to see these questions shape the 2039 list, because it would mean that we’ve successfully fought back disease (and dealt with climate change). I can’t imagine a greater sign of progress than that. For now, though, the innovations driving change are a mix of things that extend life and things that make it better. My picks reflect both. Each one gives me a different reason to be optimistic for the future, and I hope they inspire you, too.
My selections include amazing new tools that will one day save lives, from simple blood tests that diagnose cancer to toilets that destroy deadly pathogens. I’m equally excited by how other technologies on the list will improve our lives. Wearable health monitors like the wrist-based EKG will warn heart patients of impending problems, while others let diabetics not only track glucose levels but manage their disease. Advanced nuclear reactors could provide carbon-free, safe, and secure energy to the world.
One of my choices even offers us a peek at a future where society’s primary goal is personal fulfillment. Among many other applications, AI-driven personal agents might one day make your email inbox more manageable—something that sounds trivial until you consider what possibilities open up when you have more free time.
The thirty minutes you used to spend reading emails could be spent doing other things. I know some people would use that time to get more work done—but I hope most would use it for more fulfilling pursuits, like connecting with a friend over coffee, helping your child with her homework, or even volunteering in your community.
That, I think, is a future worth working toward.
The Youngest Continent
Giving the Mandela Lecture
Africa could change faster in the next generation than any continent ever has.

I was 9 years old when Nelson Mandela was sent to prison on Robben Island. As a boy, I learned about him in school, and I remember seeing reports about the anti-Apartheid movement on the evening news. Decades later, I got to meet him and work with him. In person he was even more inspiring than I had imagined. His humility and courage left an impression that I will never forget.
So it was a special honor to be invited to give the Nelson Mandela Lecture in Pretoria, South Africa. I eagerly accepted the invitation and quickly began working on my remarks.
I decided to share my optimism about Africa’s future—to explain why I think the continent has the potential to change faster in the next generation than any continent ever has.
It’s because Africa is the world’s youngest continent, and youth can go hand in hand with a special dynamism. I was 20 years old when Paul Allen and I started Microsoft. The entrepreneurs driving startup booms in Johannesburg, Lagos, and Nairobi are just as young, and the thousands of businesses they’re creating are already changing lives across the continent. The potential will only grow as the digital revolution brings more advances in artificial intelligence and robotics.
But positive change across Africa won’t happen automatically. The real returns will come only if Africans can unleash this talent for innovation in all of the continent’s growing population. That depends on whether all of its young people are given the opportunity to thrive.
It is still an open question, and it is the crux of my speech, which I gave today at the University of Pretoria. It was an honor to give this lecture, and I’m grateful to the Nelson Mandela Foundation and the university for inviting me. You can read my full speech below the video.
Remarks as delivered
Nelson Mandela Annual Lecture
University of Pretoria, South Africa
July 17, 2016
BILL GATES:
Well, thank you. Good evening, ladies and gentlemen. Graça Machel, Professor Ndebele, Vice Chancellor de la Rey, members of the Mamelodi families, friends and dignitaries.
I can’t think of a greater honor than giving a lecture named after Nelson Mandela.
I’m also thrilled that the theme of this lecture this year is “living together.”
It’s truly fitting because in many ways, “living together” was also the theme of Nelson Mandela’s life.
The system he fought against was based on the opposite idea—that people should be kept apart, that our superficial differences are more important than our common humanity.
Today, South Africans are still striving to “live together” in the fullest sense. But you are so much closer to that ideal because Nelson Mandela and so many others believed in the promise of one South Africa.
I was only nine years old when Nelson Mandela was sent to Robben Island. As a boy, I learned about him in school. I remembered seeing reports about the anti-Apartheid movements regularly on the evening news.
The first time I got to speak to him was in 1994 when he called me to help fund South Africa’s election.
I was running Microsoft, and largely focused on software most of the time, but I admired him so much, and I knew the election was historic. So I did what I could to help.
My first trip to Africa had been just the year before that in 1993 when my wife Melinda and I had traveled to East Africa.
The landscape was beautiful, the people were friendly, but the poverty there, which we were seeing for the first time, disturbed us. It also energized us.
Obviously, we knew parts of Africa were poor, but being on the continent turned what had been an abstraction into an injustice we couldn’t ignore.
Melinda and I had always known that we’d give our wealth to philanthropy eventually. But when we were confronted with such glaring inequity, we started thinking about how to take action sooner.
This sense of urgency was further spurred on by another trip in 1997 when I came to Johannesburg for the first time as a representative of Microsoft.
I spent most of the time in the richer part of the city in business meetings, but I also went to the community center in Soweto where Microsoft was donating computers.
My visit to Soweto, which was quite different then than it is now, taught me how much I had to learn about the world outside the comfortable bubble I’d lived in all my life.
As I walked into the community center, I noticed there weren’t any electrical connections. To keep the computer on, the one I was donating, they had rigged up an extension cord connected to a diesel generator outside. I realized the minute I left, the generator would get moved to something more important.
So as I read my remarks about the importance of the technology gap, I knew that it was only a small part of the story. Computers could help people do very important things, and in fact, they are part of how life on the continent can be revolutionized. But computers alone can’t feed disease or cure children. And if they can’t be turned on, they can’t do much at all.
So after that, Melinda and I moved to start our foundation because the cost of waiting had become clear.
Our work is based on the simple idea that every person, no matter where they live, should have the opportunity to lead a healthy and productive life.
We’ve spent the past 15 years learning about the issues and looking for the leverage points where we can do the most to help people seize their opportunity.
It was when I started coming to Africa regularly for the foundation that I got to know Nelson Mandela personally. AIDS was one of the first issues our foundation worked on, and Nelson Mandela was both an advisor and an inspiration.
One thing we talked about was the stigma around AIDS. So I remember 2005 very clearly when his own son died of AIDS. Rather than stay silent about the cause of his son’s death, Nelson Mandela announced it publicly because he knew that stopping the disease required breaking down the walls of fear and shame that surrounded it.
It is important to recall Nelson Mandela’s legacy, and I’m grateful for the opportunity to do so.
But Nelson Mandela was concerned about the future. He believed people could make the future better than the past. And so that’s what I want to focus on for the remainder of my talk.
What can South Africa become? What can Africa become? What can the world become? And what must we do to make it that way?
The Millennium Development Goals adopted by the United Nations in 2000 laid a foundation that enabled the world, including Africa, to achieve extraordinary progress over the last 15 years.
And the Sustainable Development Goals that recently replaced them set even more ambitious targets for creating the better world we all want.
When I talk about progress, I always start with child survival because whether children are living or dying is such a basic indicator of a society’s values.
Since 1990, child mortality in sub-Saharan Africa has been reduced by 54 percent. That means one million fewer children dying each year compared to 25 years ago.
Ten African countries achieved the very ambitious MDG target of reducing child mortality by over two-thirds.
At the same time, the incidence of poverty and malnutrition is down. And though economic growth has slowed in the past few years, it’s been very robust in many African countries for more than a decade.
This is real progress, but the Africa Rising narrative doesn’t tell the whole story about the life on the continent.
First, the progress have been uneven. You know this very well here in South Africa.
In last year’s Nelson Mandela Annual Lecture, the French economist, Thomas Piketty, pointed out that income inequality in South Africa is, quote, “higher than pretty much anywhere else in the world.”
In general, African countries tend to have higher rates of inequality than countries on other continents.And despite healthy average GDP growth in the region, many countries have not yet shared in it. Inequalities exist within countries and between countries.
So until progress belongs to all people everywhere, the real promise of living together will remain elusive.
Second, even with the great progress Africa has made, it still lags behind the rest of the world in most indicators. In sub-Saharan Africa, one in 12 children still die before they turn five. Now, that’s a vast improvement compared to 25 years ago, but African children are still 12 times more likely to die than the average child in the world.
And because rates of poverty and malnutrition aren’t shrinking as fast as the population is growing, the number of people who are poor or malnourished has actually gone up since 1990.
Finally, the progress is fragile. The continent’s two largest economies, here in South Africa and in Nigeria, are facing serious economic challenges. And new threats require attention. The Ebola crisis pointed out weaknesses in many national health systems. The effects of climate change are already being felt among farmers in many countries.
In short, to meet the ambitious goals of the Sustainable Development Goals, Africa needs to do more, do it faster, and make sure everybody benefits. It won’t be easy, but I believe it can be done.
The successes and failures of the past 15 years have generated examples and lessons we can follow. Phenomenal advances in science and technology are expanding the range of solutions available to solve development challenges. And then there is the ingenuity of the African people.
One topic that Nelson Mandela came back to over and over again was the power of youth. He knew what he was talking about because he started his career as a member of the African National Congress Youth League when he was still in his 20s.
Later on, he understood that highlighting the oppression of young people was a powerful way to explain why things must change. There is a universal appeal to the conviction that youth deserve a chance.
I agree with Mandela about young people, and that is one reason I am optimistic about the future of this continent. Demographically, Africa is the world’s youngest continent. And its youth can be the source of a special dynamism.
In the next 35 years, two billion babies will be born in Africa. By 2050, 40 percent of the entire world’s children will live on this continent.
Economists talk about a demographic dividend. When you have more people of working age and fewer dependents for them to take care of, you can generate phenomenal economic growth. Rapid economic growth in East Asia in the 1970s and 1980s was partly driven by the large number of young people moving into their workforce.
But, for me, the most important thing about young people is the way their minds work. Young people are better than old people at driving innovation because they’re not locked in by the limits of the past.
When I started Microsoft at the age of 19, computer science was a young field. We didn’t feel beholden to old notions about what computers could or should do. We dreamed about the next big thing and we scoured the world around us for the ideas and tools that would help us create it.
But it wasn’t just Microsoft. Steve Jobs was 21 when he started Apple. Mark Zuckerberg was only 19 when he started Facebook.
The African entrepreneurs driving startup booms in the Silicon Savannahs from Johannesburg and Cape Town to Lagos and Nairobi are just as young in chronological age, but also in their outlook. The thousands of businesses they’re creating are already changing daily life across the continent.
In a few days, I’ll be meeting with some of these young innovators. People like the 21-year-old who founded Kenya’s first software coding school to provide other young people with computer programming skills. And like the 23-year-old social entrepreneur here in South Africa who manufactures school bags from recycled plastic shopping bags. Besides being highly visible to protect children as they’re walking to school, these school bags sport a small solar panel that charges a lantern during the journey to and from school, providing illumination so students can study at home.
The full returns will come if we can multiply this talent for innovation by the whole of Africa’s growing youth population. That depends on whether Africa’s young people—all of Africa’s young people—are given the opportunity to thrive.
Nelson Mandela said, “Poverty is not natural, it is man made and it can be overcome and eradicated by the actions of human beings.”
We are the human beings that must take action. And we have to decide now because this unique moment won’t last. We must clear away the obstacles that are standing in young people’s way so that they can seize all of their potential.
If young people are sick and malnourished, their bodies and brains will never fully develop. If they are not educated well, their minds will lie dormant. If they do not have access to economic opportunities, they will not be able to achieve their goals.
But if we invest in the right things, if we make sure the basic needs of Africa’s young people are taken care of, then they will have the physical, cognitive, and emotional resources they need to change the future. Life on this continent will improve faster than it ever has. And the inequities that have kept people apart will be erased by broad-based progress that is the very meaning of the words “living together.”
When Melinda and I started our foundation 15 years ago, we asked ourselves: What are the areas of greatest impact? It was clear to us that investing in health was high on the list. When people aren’t healthy, they can’t turn their attention to other priorities. But when health improves, life improves by every measure.
Over the last 15 years, our foundation has invested more than $9 billion in Africa. And we are committed to keep on investing to help Africa.
In the next five years, we will invest another $5 billion.
Some of this money has gone into discovering and developing new and better vaccines and drugs to help prevent infectious disease. We’ve also invested in global partnerships that work closely with countries across the continent to get these solutions to the people who need them most.
We’ve been fortunate to work with amazing partners, and together we’ve seen incredible progress.
For example, the entire continent of Africa has been polio free for two years, which puts us within reach of wiping polio out from the face of the earth forever.
The newest vaccines that protect children from two of the most devastating diseases—pneumonia and diarrhea—are reaching children across Africa at the same time they’re available for children in wealthier countries.
Countries that invest in strong, community-based primary healthcare systems—including Malawi, Ethiopia, and Rwanda—are making great progress reducing child mortality.
Malaria infections and deaths are down significantly thanks to better treatment and prevention tools.
And efforts like the Ouagadougou Partnership in West Africa are helping millions of women get access to contraceptives, which make it easier for them to care for their families.
HIV/AIDS is another area where there’s been good progress. Though it’s a complicated story, and there are still big challenges ahead.
In a few days, I’ll be speaking at the International AIDS Conference in Durban. When the global AIDS community last met there in 2000, only a few thousand Africans were receiving antiretroviral drugs. Today, more than 12 million Africans are on treatment, more than a quarter of them living here in South Africa.
So this is a huge achievement, and millions of lives have been saved. But the rate of new infections remains high. In sub-Saharan Africa, more than 2,000 young people under the age of 24 are infected every single day. The number of young people dying from HIV has increased fourfold since 1990.
We need to get people to get diagnosed, we need people to seek treatment, and people who are on treatment need to be fully adherent.
Along with HIV, we have high rates of tuberculosis, including here in South Africa where TB/HIV co-infection continues to wage a devastating toll.
So we need more creative ways to make testing and treatment accessible and easier to use.
We need to get much more out of existing prevention methods like condoms, voluntary medical male circumcision, and oral anti-HIV medicine.
And we’re going to have to invent new and better preventative solutions like medicines you only have to take once a month or an effective vaccine.
If we don’t act both on today’s treatment and create these tools, the hard-earned gains made against HIV in sub-Saharan Africa over the last 15 years could actually be reversed. Because of the population growth, just doing what we are today is not enough. We need to do more.
Nutrition is another critical area of focus for Africa. Nearly one-third of the continent’s children suffer from malnutrition that stunts their growth and robs them of their physical and cognitive potential. Millions more suffer from micronutrient deficiencies. These are impacts that last a lifetime and impact whole generations of African youth.
African Development Bank President Akin Adesina put it best when he said recently that the greatest contributor to Africa’s economic growth is not physical infrastructure, but gray matter infrastructure, people’s brainpower. The best way to build that infrastructure includes proper nutrition.
Without eliminating malnutrition, we won’t get the great potential that’s there.
We know that when mothers and infants get good nutrition, that breast feeding is a key part of that. We know that certain vitamins and minerals are essential for children.
We have a number of ways to intervene to help nutrition, things like fortified cooking oil, sugar fortified with vitamin A, and sugar and flour enriched with iron, zinc, and vitamin B.
One of the most exciting advances is the breeding of crops so they are naturally more nutritious. For example, when adolescents eat high-iron pearl millet, their likelihood of iron deficiency is reduced six-fold. And just half a cup of biofortified orange sweet potato is all it takes to meet a child’s daily vitamin A needs.
The toll of micronutrient deficiency is huge, but the costs of fighting it are not.
Recent estimates done in Nigeria and Uganda indicate that every dollar invested to reduce stunting returns $17 in greater earning capacity in the workplace.
When children’s bodies and brains are healthy, the next step is an education that helps them develop the knowledge and skills to become productive contributors to society.
Improving education is hard work. I’ve learned this first hand through our foundation’s efforts to create better learning outcomes for primary, secondary, and university students in the United States.
But this hard work is incredibly important. A good education is the best lever we have for giving every young person a chance to make the most of their lives.
In Africa, as in the United States, we need new thinking and new educational tools to make sure that a high-quality education is available to every child.
In Uganda, young innovators at the NGO called Educate! are helping high schools prepare young people for the workplace by teaching students how to start their own business.
And with the high level of mobile phone penetration in Africa, technology using mobile phones to connect to the Internet have the potential to help students build foundational skills while giving teachers better feedback and support.
Globally, the educational technology sector is innovating and growing rapidly and it’s exciting to see new models and tools emerging to meet the needs of educators and students who are not connected to current systems.
At the university level, we need not only to broaden access, we have to also ensure that we have high-quality public universities that will launch the next generation of scientists, entrepreneurs, educators, and government leaders.
South Africa is blessed with some of the best universities in Africa, like the one we’re at today.
For our foundation, we partner with these universities to do our work in health and agricultural research. Maintaining the quality of this country’s higher-education system, while expanding access to more students will not be easy, but it is critical to South Africa’s future.
Other countries in the region will do well to follow South Africa’s example and provide the highest-level university education to the largest number of qualified students.
Healthy, educated young people are eager to make their way in the world. But Africa’s youth must have economic opportunity to channel their energy into progress.
Some of those youths will work in agriculture, where still over half of the workforce toils today.
We need advances to make agriculture far more productive. Today, the seeds that are used are unproductive, the soils are not very good, and so many farmers grow just enough to feed their family.
With climate change leading to more severe weather, doing more of the same will not be good enough.
The key to this is a series of innovation at every step along the way from farm to market.
First, farmers need better tools to avoid disasters and grow surplus. Things like seeds that can tolerate drought, floods, pests, and disease; affordable fertilizers that have the right mix of nutrients to replenish the soil; and easy-to-administer livestock vaccines that can help prevent flocks and herds from being wiped out.
Next, farmers need to be connected to a market where they can buy these inputs at a good price, and sell their surplus, and earn a profit that they can invest not only in their family’s basic needs, but also back into the farm.
This, in turn, will provide employment opportunities both on and off the farm as more prosperous farmers begin to support a range of agribusinesses like seed dealers, trucking companies, and processing plants.
I recently met with a group of young crop breeders, one from Ethiopia, one from Kenya, one from Nigeria, one from Uganda. I really love talking about the science of plant productivity. And in this case, I was amazed at the expertise all of these scientists brought to their work on cassava, a staple crop that provides more than one-third of the calories in many African diets.
Some had ways of improving the nutritional content of cassava. Others were breeding a variety that can resist both of the devastating diseases that are threatening to wipe out the cassava crop.
Our foundation is also working with a young computer scientist from Makerere University who designed a mobile phone app that lets farmers upload a picture of their cassava plants to find out whether it’s infected or not.
These are examples of the kind of innovators who can drive an agricultural transformation across the continent if they have the support they need. For many decades, agriculture has suffered from dramatic underinvestment. Many governments didn’t see the link between their farmers and economic growth.
Now, however, this misconception is gone. And through the Comprehensive African Agricultural Development Program, countries have a framework for transforming agriculture. The investment needs to follow so that young Africans have the means to create the thriving agriculture they envision.
With Africa’s farms as a base, the next step in economic growth is to promote job creation in other sectors. Doing this will require investment in infrastructure including energy.
Seven in 10 Africans lack access to power, which makes it harder to do everything. Harder to get healthcare in a dark clinic. Harder to learn in school when it’s boiling hot. Harder to be productive when you can’t use labor-saving machinery.
Ultimately, a shortage of power, like many African countries—including South Africa—have experienced, is also a drag on economic growth.
Businesses will not invest fully in places where they can’t operate efficiently.
A recent report projected that 500 million Africans won’t have electricity even in 2040. We need to change that.
What Africa needs is what the whole world needs: An energy advance that provides cheap, clean energy for everyone.
I’ve spent a lot of my time in the last two years working on this issue because it’s such an important advance. I’m involved with a group of business people who are collaborating with governments to not only increase energy R&D, but also to vastly increase the private investment in this area.
I get angry when I see that Africa is suffering the worst effects of climate change, although Africans had almost nothing to do with causing this.
The rich countries need to follow through on their commitment to double their energy R&D budgets so that we get the breakthroughs that are applicable globally, and we need to do that urgently.
Africa needs power now. And so there are many pragmatic steps we need to take even in advance of these new inventions.
In parts of Africa, there’s hydro and geothermal sources which are both reliable and renewable that can be exploited. There’s been a lot of work on small-scale grids and the use if micro solar. This approach can provide individuals with electricity for basic purposes, but we also need large-scale power including well-managed electrical grids.
It means organizing the power system so that it’s economic, so that the electronic bills are paid for, and so that the network is reliable 100 percent of the time.
Once we get economic viability for these utilities, then it bootstraps the economy. It allows investments that are job creating.
So there are many challenges that I’ve laid out here: Challenges in health, education, agricultural productivity, energy, and creating enough job opportunities.
These advances only happen in the context of governments that function well enough to enable them. I applaud initiatives like Mo Ibrahim’s Annual Index of African Governments, which looks objectively at multiple measures of government performance in each country on the continent.
Citizens in other regions would be well served by this kind of comprehensive effort to spotlight and spread effective governance.
A lot can be accomplished by focusing on fiscal governance and accountability. Here in South Africa, the government gets strong marks for the budget information it provides to the public.
The International Budget Partnership, an independent monitoring organization, also ranks South Africa highly for its oversight of government spending.
In some countries, individual citizens are leading the way. In Nigeria, 30-year-old Oluseun Onigbinde gave up a career in banking years ago to devote himself full time to pulling back the curtain on the Nigerian federal expenditure.
With savvy use of data and social media, he founded BudgetIT Nigeria, which provides facts and figures the average Nigerian can understand. No doubt, he’s a thorn in the side of some of Nigeria’s elite, but to me he’s an example of what one person can do to make a difference.
Governments have an opportunity not only to learn from what’s been done in the past, but to do things in new ways. One of the exciting prospects is the role they can play in accelerating use of digital technology to leapfrog traditional models and costly infrastructure associated with banking and delivery of government services.
By using mobile phones, tens of millions of people are already storing money digitally and using their phones to make purchases as if they were debit cards.
A good example of this is M-PESA in Kenya. These services don’t just give people a better way to move money around, they give people a place to save cash to fund a startup of a micro enterprise or pay a child’s school fee. They create informal insurance networks of friends and families who can help with unexpected shocks. And they increase the profitability of small businesses by lowering transaction costs, making it easy to order products and supplies, and having greater security of financial assets.
A digital financial connection can also help governments deliver services more efficiently. Studies from India show the government able to save tens of billions a year by connecting households to a digital payment system and automating all government payments.
The early evidence suggests that similar programs in Africa can also yield substantial benefits. For example, recent research in Uganda showed that providing people with digital cash transfers rather than direct food subsidies not only saved the cost of delivery, it also improved nutrition because recipients used the money to purchase a greater diversity of foods and to space out meals as needed.
Governments can accelerate this digital transformation by implementing policies that encourage commercial investment, innovation, and healthy competition.
Countries like Kenya, Tanzania, and Nigeria are already investing in the building blocks of this new digital financial platform. And I believe they’ll see substantial positive returns.
If there’s one thing I’m sure of, it’s this: Africa can achieve the future it aspires to.
That future depends on the people of Africa working together across economic and social strata and across national borders to lay a foundation so that Africa’s young people have the opportunities they deserve.
Recently, I had a meeting with students at Addis Ababa University. I started asking them the kinds of questions you would ask college students in the United States like, “What do you want to do after you graduate? What fields are you thinking of going into?”
They looked at me like I was kind of crazy for asking those questions. Each of them had a plan for their future. They felt their parents had sacrificed for decades so they could go to this university. They weren’t weighing their options, they had come to the university to get specific training, and they were eager to take that training and use it to make their country more prosperous.
They saw themselves as part of a large community with great needs.And they were going to dedicate themselves to serving that community by meeting those needs.
I see that sense of purpose when I come to Africa, and especially when I talk to young Africans. I think it’s a unique asset that people see the need to change and that they want to give back.
The students here believe not only in themselves, they also believe in their countries and the future of the continent. Our priority is to make sure they have the opportunity to turn those beliefs into action because young people with this sense of purpose can make the difference between stagnation and faster progress.
Nelson Mandela said, “Young people are capable, when aroused, of bringing down the towers of oppression and raising the banners of freedom.” But our duty is not merely to arouse, our duty is to invest in these young people, to put in place the basic building blocks so they can build the future.
And our duty is to do it now because the innovations of tomorrow depend on the opportunities available to children today.
I’m sure it’s clear to everyone that these are big and complicated challenges. But it’s just as clear that people with bravery, energy, intellect, passion, and stamina can face big, complicated challenges and overcome them.
There is so much more work to be done to create a future in which we can all live together, but there are also so many people who are eager to get to work.
Let’s do everything within our power right now to help build the future that Nelson Mandela dreamed of and the future that we will achieve together.
Thank you.
Coop Dreams
Why I would raise chickens
I’m excited about the poverty-fighting power of poultry.

If you were living on $2 a day, what would you do to improve your life?
That’s a real question for the nearly 1 billion people living in extreme poverty today. There’s no single right answer, of course, and poverty looks different in different places. But through my work with the foundation, I’ve met many people in poor countries who raise chickens, and I have learned a lot about the ins and outs of owning these birds. (As a city boy from Seattle, I had a lot to learn!) It’s pretty clear to me that just about anyone who’s living in extreme poverty is better off if they have chickens.
In fact, if I were in their shoes, that’s what I would do—I would raise chickens.
Here’s why:
- They are easy and inexpensive to take care of. Many breeds can eat whatever they find on the ground (although it’s better if you can feed them, because they’ll grow faster). Hens need some kind of shelter where they can nest, and as your flock grows, you might want some wood and wire to make a coop. Finally, chickens need a few vaccines. The one that prevents the deadly Newcastle disease costs less than 20 cents.
- They’re a good investment. Suppose a new farmer starts with five hens. One of her neighbors owns a rooster to fertilize the hens’ eggs. After three months, she can have a flock of 40 chicks. Eventually, with a sale price of $5 per chicken—which is typical in West Africa—she can earn more than $1,000 a year, versus the extreme-poverty line of about $700 a year.
- They help keep children healthy. Malnutrition kills more than 3.1 million children a year. Although eating more eggs—which are rich in protein and other nutrients—can help fight malnutrition, many farmers with small flocks find that it’s more economical to let the eggs hatch, sell the chicks, and use the money to buy nutritious food. But if a farmer’s flock is big enough to give her extra eggs, or if she ends up with a few broken ones, she may decide to cook them for her family.
- They empower women. Because chickens are small and typically stay close to home, many cultures regard them as a woman’s animal, in contrast to larger livestock like goats or cows. Women who sell chickens are likely to reinvest the profits in their families. Read more about women and chickens in Melinda’s blog post.
Dr. Batamaka Somé, an anthropologist from Burkina Faso who has worked with our foundation, has spent much of his career studying the economic impact of raising chickens in his home country. In this video he explains why he is so passionate about poultry.
A big bet on chickens
Our foundation is betting on chickens. Alongside partners throughout sub-Saharan Africa, we are working to create sustainable market systems for poultry. It’s especially important for these systems to make sure farmers can buy birds that have been properly vaccinated and are well suited to the local growing conditions. Our goal: to eventually help 30 percent of the rural families in sub-Saharan Africa raise improved breeds of vaccinated chickens, up from just 5 percent now.
When I was growing up, chickens weren’t something you studied, they were something you made silly jokes about. It has been eye-opening for me to learn what a difference they can make in the fight against poverty. It sounds funny, but I mean it when I say that I am excited about chickens.
The big chill
Can this cooler save kids from dying?
These innovations are helping deliver vaccines to the most remote places on earth.

Two of the things I love most about my job are getting to see amazing innovations and talk to remarkable people. During a recent trip to New York, I got to check both boxes. I met a woman named Papa Blandine Mbwey who is using a revolutionary new invention to help more kids get vaccinated.
Blandine has worked as a vaccinator in a remote part of the Democratic Republic of the Congo for over a decade. Most days, she travels on foot to villages all over her region so she can vaccinate kids who live too far from a health clinic to make the trip themselves.
Blandine’s job is complicated by a simple fact: vaccines must be kept between 2 and 8° C. If they get too warm, they spoil. If they get too cold, the water in them freezes, and they can stop working. Vaccines must stay within this temperature range through each step of what’s called the “cold chain.”
By the time Blandine reaches the children, the vaccines she’s carrying have traveled nearly 5,100 miles. They could have spoiled at any point during that journey, but vaccines are particularly at risk during the last two stops.
First there’s the health clinics where vaccinators like Blandine usually pick up their supply of vaccines. Many of these clinics are in areas with frequent power outages or no electrical grid at all, which means the refrigerators can’t always keep the vaccines cold.
But even if the vaccines survive the clinic, they still need to make it to the children. Most vaccinators carry them in ice-lined coolers. If you’ve used a cooler to keep your drinks cold at a picnic, you know the big problem with ice: it starts melting as soon as you take it out of the freezer. This means that some of the kids never get vaccinated, because coolers can’t keep vaccines cold long enough to reach them.
Several years ago, I asked a group of inventors called Global Good that I support to take on the cold chain problem. They came up with two remarkable innovations that are changing the game for vaccinators like Blandine.
The first is the MetaFridge. Although it looks like a regular refrigerator, MetaFridge has a hidden superpower: it keeps vaccines cold without power for at least five days. The electrical components are designed to keep working through power surges and brown-outs. During extended outages, an easy-to-read screen tells you how much longer it can stay cool without power so health workers know when to run a generator or move vaccines elsewhere. And if the fridge stops working properly, it transmits data remotely to a service team so they can fix it before vaccines are at risk of spoiling.
The other innovation Global Good invented is the Indigo cooler, which is the device you see Blandine using in the video above. It keeps vaccines at the right temperature for at least five days with no ice, no batteries, and no power required during cooling.
It sounds counterintuitive, but the Indigo needs heat before you can use it. When exposed to a heat source, water inside its walls evaporates and moves into a separate compartment. It can then sit on a shelf for months after heating, ready for use.
When it’s finally time to head out to the children, you open a valve, and the water starts moving back where it started. Because the pressure inside the Indigo has been lowered to the point where water evaporates at 5° C, the water particles take heat with them (the way sweating lowers your body temperature) and cool the storage area down to the perfect temperature for vaccine storage.
Both inventions are already making an impact in the field. A Chinese manufacturer started selling the MetaFridge last year, and a new solar-powered version will hit the market soon. One of the biggest surprises so far is just how much we’ve learned from its remote data monitoring capabilities. We knew the electrical grids in sub-Saharan Africa were unreliable, but we now know exactly how much the power fluctuates. This information will be helpful moving forward for health providers and anyone designing a product meant to work in these areas.
The Indigo is in the field trial phase. It’s still early, but the data suggests that the Indigo is allowing vaccinators to reach four times as many places as they could with the old ice-based coolers. That’s a big deal, and I’m excited to learn more.
Keeping vaccines cold when you’re delivering them to the most remote places on earth is a tough problem—and these devices show how innovation can help solve tough problems. I hope MetaFridge and Indigo inspire other inventors to find creative solutions.
Ring the alarm
The next epidemic is coming. Here’s how we can make sure we’re ready.
I was honored to be asked to give this year’s Shattuck Lecture.

Four years ago, the world was stunned by the Ebola outbreak in West Africa. Panic broke out all over the globe. Governments scrambled to contain the infection. By the time the last patient tested negative for the disease, the outbreak claimed thousands of lives and caused billions of dollars in economic losses.
The 2014 Ebola outbreak was a stark reminder of how vulnerable our society is to epidemics of infectious diseases. We weren’t ready then, and we’re still not ready now—but we can be. We don’t know when the next epidemic will strike, but I believe we can protect ourselves if we invest in better tools, a more effective early detection system, and a more robust global response system.
When the Massachusetts Medical Society asked me to deliver this year’s Shattuck Lecture, I knew I wanted to talk about epidemic preparedness. I was honored to address their annual meeting earlier today. Here is the full text of my prepared remarks:
BILL GATES:
Thank you, Dr. Drazen, for that kind introduction. It’s an honor to be invited to deliver the Shattuck Lecture.
Most of the speeches I give on global health are about the incredible progress and exciting new tools that are helping the world reduce child mortality and tackle infectious diseases. Thanks to better immunization and other interventions, child mortality has been reduced by more than 50 percent since 1990. We are on the verge of eradicating polio. HIV is no longer a certain death sentence. And half the world is now malaria-free.
So usually, I’m the super-optimist, pointing out that life keeps getting better for most people in the world.
There is one area, though, where the world isn’t making much progress, and that’s pandemic preparedness. This should concern us all, because if history has taught us anything, it’s that there will be another deadly global pandemic.
We can’t predict when. But given the continual emergence of new pathogens, the increasing risk of a bioterror attack, and how connected our world is through air travel, there is a significant probability of a large and lethal, modern-day pandemic occurring in our lifetimes.
Watching Hollywood thrillers, you’d think the world was pretty good at protecting the public from deadly microorganisms. We like to believe that somewhere out there, there is a team ready to spring into action – equipped with the latest and best technologies.
Government agents like Jack Bauer in 24. Harvard professors like Robert Langdon in Inferno. And WHO epidemiologists like Dr. Leonora Orantes in Contagion – who even risked getting kidnapped as she pursued “Patient Zero.”
In the real world, though, the health infrastructure we have for normal times breaks down very rapidly during major infectious disease outbreaks. This is especially true in poor countries. But even in the U.S., our response to a pandemic or widespread bioterror attack would be insufficient.
Several things in the last decade have made me pay closer attention to the risk of future pandemics. One was the outbreak of Swine Flu in 2009. While H1N1 wasn’t as lethal as people initially feared, it showed our inability to track the spread of disease and develop new tools for public health emergencies.
The Ebola epidemic in West Africa four years ago was another wake-up call. As confirmed cases climbed, the death toll mounted, and local health systems collapsed. Again, the world was much too slow to respond.
And, as biological weapons of mass destruction become easier to create in the lab, there is an increasing risk of a bioterror attack.
What the world needs – and what our safety, if not survival, demands – is a coordinated global approach. Specifically, we need better tools, an early detection system, and a global response system.
Today, I’d like to speak with you about some of the advances in tools – vaccines, drugs, and diagnostics – that make me optimistic we can get a leg up on the next pandemic. And I’ll talk about some of the gaps we must address in preparedness and response.
Interestingly, the first Shattuck Lecture – given back in 1890 – focused on a pandemic . . . the Russian flu that struck Massachusetts the previous year. The Russian flu was not especially deadly. But it was the first flu pandemic to spread across continents connected by rail travel – and between continents connected by fast ocean liners. The virus circled the globe in just four months.
But the world was soon in for much worse. Less than 30 years later, the Boston area was one of the first places in the U.S. to feel the deadly effects of the 1918 flu. Military personnel getting off and on ships at the Commonwealth Pier – near where we are meeting today – helped carry the pathogen across the U.S. and back to the battlefields of World War I.
This animation shows how quickly the virus spread across the United States. It took five weeks and killed 675,000 people.
The death toll was so great that average life expectancy in the U.S. for that period dropped by 12 years.
Worldwide, the 1918 flu killed an estimated 50 million people, perhaps more.
We have better tools today than we did a century ago. We have a seasonal flu vaccine, although it’s not always effective, you have to get one every year, and most people in the world never get the shot. We also have antibiotics for secondary infections of bacterial pneumonia.
Despite these advances, this animated simulation by the Institute for Disease Modeling shows what would happen if a highly contagious and lethal airborne pathogen – like the 1918 flu – were to occur today.
Nearly 33 million people worldwide would die in just six months.
That’s the sobering news. The good news is that scientific advances and growing interest on the federal level, in the private sector, and among philanthropic funders makes development of a universal flu vaccine more feasible now than 10 or 20 years ago.
Our foundation is involved in a variety of research partnerships, including a collaboration between the Icahn School of Medicine at Mount Sinai, GlaxoSmithKline, and PATH.
Their work focuses on several vaccine candidates that did well in animal trials and which are now in human trials.
We are also supporting efforts by others, including the National Institute of Allergy and Infectious Diseases, whose vaccine candidate is expected to advance to human safety trials in about a year.
To broaden efforts even further, today we are launching a $12 million Grand Challenge in partnership with the Page family to accelerate the development of a universal flu vaccine. The goal is to encourage bold thinking by the world’s best scientists across disciplines, including those new to the field.
Lucy and Larry Page are also supporting efforts by the Sabin Vaccine Institute to encourage innovative approaches that eliminate the threat of a deadly flu pandemic.
However, the next threat may not be a flu at all. More than likely, it will be an unknown pathogen that we see for the first time during an outbreak, as was the case with SARS, MERS, and other recently-discovered infectious diseases.
The world took an important step last year to begin addressing this risk with the launch of a public-private partnership called the Coalition for Epidemic Preparedness Innovations (CEPI).
With funding commitments of more than $630 million, CEPI’s first order of business is advancing the development of vaccines for three of the priority diseases on the WHO list for public health R&D: Lassa fever, Nipah virus, and Middle East Respiratory Syndrome.
CEPI is also working on rapid-response platforms to produce safe, effective vaccines for a range of infectious diseases – almost as quickly as new threats emerge. Later this year, CEPI will announce grants to several companies working with a variety of technologies – including nucleic acid vaccines, viral vectors, and other innovative approaches. The goal is to be able to develop, test, and release new vaccines in a matter of weeks or months, rather than years.
I’m a big fan of vaccines, but they may not be the answer when we have to respond immediately to rapidly spreading infectious disease pandemics. Not only do vaccines take time to develop and deploy; they also take at least a couple of weeks after the vaccination to generate protective immunity. So, we need to invest in other approaches like antiviral drugs and antibody therapies that can be stockpiled or rapidly manufactured to stop the spread of pandemic diseases or treat people who have been exposed.
Earlier this year, the Shionogi pharmaceutical company received approval in Japan for a new influenza anti-viral, Xofluza This single-dose drug stops flu in its tracks by inhibiting an enzyme that the virus needs to multiply.
And PrEP Biopharm, a development stage biopharmaceutical company, has demonstrated in human challenge studies that pre-activating the innate immune response through intranasal delivery of a double-stranded viral RNA “mimic” can prevent both influenza and rhinovirus.
Since the host’s innate immune response is non-virus specific, such an approach has the potential to offer protection against other types of respiratory viruses as well.
Monoclonal antibody therapies have also made incredible advances in the last couple of decades, leading to several products for cancer and autoimmune diseases. During the Ebola outbreak in West Africa several years ago, researchers were able to identify and test a promising combination of monoclonal antibodies to treat infected patients.
And a growing pipeline of broadly neutralizing antibodies are being discovered in some individuals exposed to infectious diseases. For example, a small percentage of people infected with HIV develop antibodies with high potency and breadth of coverage sufficient to protect against many strains of the virus. The same is true for some people infected with the flu.
Different sets or cocktails of these exceptional antibodies may protect against a pandemic strain of a virus even if it has genetically evolved. It is conceivable that we could create libraries of these antibodies, produce manufacturable seed stocks, and have them ready for immediate use in an outbreak—or ready to scale up manufacturing if a pandemic ensues. If we can learn how to use RNA or DNA gene delivery effectively, we may not need to make the antibodies at all.
Rapid diagnosis is also critical, especially at the beginning of an outbreak when quarantine, treatment, and other public health measures are most effective. To that end, researchers at the Broad Institute and at UC-Berkeley have developed a highly-sensitive point-of-care diagnostic test that harnesses the powerful genetic engineering technology known as CRISPR.
But instead of using CRISPR to edit DNA, they have programmed an associated protein called Cas13 to hunt for specific pieces of RNA. When Cas13 locates the relevant genetic sequence, it releases a signal molecule that indicates the presence or absence of the target.
In a paper published yesterday in the journal, Science, the Broad researchers highlighted the field-use potential of this new diagnostic. Using paper strips similar to a pregnancy test – and with minimal sample processing – the diagnostic can check a patient’s blood, saliva, or urine for evidence of a pathogen.
What’s more, it can test for multiple pathogens at once. It could, for example, identify if someone is infected with Zika or dengue virus, which have similar symptoms.
There are also some interesting advances that leverage the power of computing to help predict where pandemics are likely to emerge and model different approaches to preventing or containing them.
Over the last few years, researchers at the Institute for Health Metrics and Evaluation at the University of Washington have developed a sophisticated computer model that combines data from dozens of sources with geospatial mapping to predict the pandemic risk of infectious diseases.
They recently looked at the pandemic potential of four viral hemorrhagic fevers in Africa – including Ebola. Their analysis confirmed that Guéckédouprefecture in Guinea – where the West African Ebola outbreak originated – was indeed one of the most likely places where an individual Ebola case could lead to a widespread epidemic.
The research also pinpointed dozens of other African communities that are at high risk of outbreaks of hemorrhagic fevers.
Meanwhile, researchers at the Institute for Disease Modeling are pushing the boundaries of computational epidemiology to provide a deeper understanding of both the spread of infectious diseases and the effectiveness of different control and eradication strategies.
In the effort to eliminate malaria, for example, IDM is combining surveillance data with computational modeling to tailor antimalarial efforts to unique local conditions. They are also using quantitative analysis and modeling to evaluate various control strategies for HIV, TB, and to eradicate polio. This kind of research could provide valuable information to help predict disease transmission and identify prevention measures and intervention tactics for epidemics and pandemics.
At the Munich Security Conference last year, I asked world leaders to imagine that somewhere in the world, there is a weapon that exists – or that could emerge – that is capable of killing millions of people, bringing economies to a standstill, and casting nations into chaos.
If this were a military threat, the response – of course – would be that we should do everything possible to develop countermeasures. In the case of biological threats, that sense of urgency is lacking.
The world needs to prepare for pandemics the way the military prepares for war. This includes simulations and other preparedness exercises so we can better understand how diseases will spread and how to deal with things like quarantine and communications to minimize panic.
We need better coordination with military forces to ensure we can draw on their mobilization capacity to transport people, equipment, and supplies on a mass scale.
We need a reserve corps of trained personnel and volunteers, ready to go at a moment’s notice. And we need manufacturing and indemnification agreements in place with pharmaceutical companies –with expedited review processes for government approval of new treatments.
Last month, Congress directed the administration to come up with a comprehensive plan to strengthen global health security – here and abroad. This could be an important first step if the White House and Congress use the opportunity to articulate and embrace a leadership role for the U.S. in global health security.
No other country has the depth of scientific or technical expertise that we do – drawing on the resources of institutions like the NIH, the CDC, and advanced research organizations like DARPA and BARDA.
Our biopharmaceutical industry is the global leader in biomedical innovation. And, on the world stage, the U.S. is an influential member of international forums like the UN, the WHO, the G7, and the G20.
The point is that the U.S. can and should play a leadership role in creating the kind of pandemic preparedness and response system the world needs.
As I said at the start, I’m fundamentally an optimist, and that gives me hope that we can get prepared for the next big pandemic.
The global community eradicated smallpox, a disease that killed an estimated 300 million people in the 20th century alone.
We are on the verge of eradicating polio, a disease that 30 years ago was endemic in 125 countries and that paralyzed or killed 350,000 people a year.
And today, nearly 21 million people are receiving life-saving HIV treatment, thanks primarily to the support of the world community.
America’s global HIV initiative, PEPFAR, was the catalyst for world action on the AIDS crisis. It’s an example of the kind of leadership we need from the U.S. on a broader effort to make the world safer from other infectious disease threats. With strong bipartisan support, PEPFAR has saved millions of lives and shown that national governments can work together to address pandemics.
Somewhere in the history of these collective efforts is a roadmap to create a comprehensive pandemic preparedness and response system.
We must find it and follow it because lives – in numbers too great to comprehend – depend on it.
Thank you for the opportunity to address you today.
Buzz Kill
Could this be the first country in sub-Saharan Africa to defeat malaria?
Swaziland’s success fighting malaria can teach the world valuable lessons.

In the tiny African kingdom of Swaziland*, one of the most effective tools in the fight against malaria is a telephone number: 977.
When someone tests positive for the mosquito-borne disease at a Swazi clinic, a nurse immediately dials those three digits to report the case to the country’s national emergency response center. The call triggers a text message to the national malaria program team, which dispatches investigators—armed with computer tablets that have built-in satellite maps and GPS software—to interview the patient and test all people living within a one-kilometer radius of their home. A separate team is called in to reapply insecticide to the walls of homes in the community to help protect other families from infection.
Such vigilance is one of the reasons why Swaziland may become the first malaria-free country in sub-Saharan Africa, where most malaria deaths occur.
Swaziland’s well-coordinated malaria program—including a robust surveillance and control system—has helped reduce the number of cases in the country by more than 90 percent since 2002. Now, Swaziland aims to eliminate malaria entirely within its borders by 2020.
Swaziland’s bold goal is evidence of the incredible progress the world has made against malaria. Between 2000 and 2015, the combination of increased donor investment, strengthened political commitment, and new tools (including artemisinin combination therapies, rapid diagnostic tests, indoor residual spraying, and insecticide-treated bed nets), led to a 60 percent decline in malaria deaths.
At the same time, the difficulties Swaziland has experienced trying to become malaria free are a sobering reminder of the challenges the world faces to reach its goal of eradicating the disease. While the number of malaria cases in Swaziland has fallen to just a few hundred cases each year, tackling those final cases is more difficult than anyone imagined. Swaziland thought it would eliminate the disease by the end of 2015, and again by the end of 2017, but each time fell short of its goal. Last year, Swaziland saw its number of malaria cases rise sharply.
Globally, progress in the malaria fight has stalled. Further progress is in peril given the plateauing funding levels which make it impossible to fill remaining gaps in prevention and treatment of malaria and address the challenges of drug and insecticide resistance. After years of dramatic declines in malaria cases and deaths, the world is starting to lose ground. In 2017, the World Malaria Report showed that for the first time in years the number of malaria cases went up.
These setbacks should not lead to despair. They should serve as a wake-up call. As I told health officials at the Malaria Summit in London last week, the world needs a new strategy to meet the challenges ahead. That means developing innovations that will keep driving down malaria cases and malaria deaths, while tailoring interventions to address the specific needs of a country or region.
Swaziland is a good example of how countries can adapt their malaria control strategies to meet their unique circumstances. One of Swaziland’s biggest challenges is the cross-border movement of people infected with the disease from outside the country. Mozambique, Swaziland’s next-door neighbor, has one of the highest malaria burdens in the world. Workers from Mozambique may come into Swaziland with malaria. And when Swazis go to Mozambique, they sometimes return with the disease, which can then be passed on to their neighbors. Unpredictable weather also poses a challenge. The sudden spike of new cases last year was driven by heavier rainfall in the region, resulting in more mosquito breeding.
Swaziland and Mozambique are part of the Elimination 8 regional malaria elimination effort, which aims to wipe out malaria from eight countries in southern Africa. Last year, as part of that effort, Swaziland and Mozambique set up malaria posts along their border. As people go back and forth between the two countries, they are offered malaria tests and treatment to help prevent the importation of new cases. Since the posts were set up last year, thousands of people have been tested and treated and the national malaria program is optimistic that the number of cases will fall this year as a result.
At the same time, Swaziland remains committed to the painstaking work of investigating every new malaria case and responding swiftly to reduce the chance the disease will spread. The country also organized intensive media campaigns to warn residents and travelers of the danger of malaria and teach them how to protect themselves. Malaria diagnosis and treatment are free to everyone in private and public clinics.
I look forward to hearing more about Swaziland’s progress in the months ahead. If successful eliminating malaria within its borders, Swaziland can achieve a major milestone toward a goal once thought impossible—making Africa malaria free. I hope to see many more countries follow its lead.
* Just before I posted this, King Mswati III of Swaziland announced that the name of the country was changing to the Kingdom of eSwatini. In order to avoid confusion, I’ve used Swaziland in this post.
Out for blood
This animal kills more people in a day than sharks do in a century
I’m bringing back Mosquito Week on the Gates Notes.

Mosquitoes keep me up at night.
If you ask someone about what things scare people the most, there’s a list of usual suspects: shark attacks, heights, enclosed spaces, etc. Mosquitoes usually don’t make the cut—but they frighten me more than almost anything else.
This fear might be a bit irrational in Seattle, where I live. Our climate is too mild for the types of mosquitoes that harbor serious diseases. In other parts of the world, however, families have good reason to be afraid. Mosquitoes and the diseases they carry kill more than half a million people every year. Consider this mind-blowing statistic:
Of all the illnesses mosquitoes spread, malaria is the worst by far. More than 200 million people suffer from it every year, and a child dies from malaria every other minute of every day. If you survive, it can leave you vulnerable to other debilitating diseases and chronic anemia. It’s an awful, painful disease (I wrote about what it feels like to have malaria a couple years ago).
Melinda and I encounter a lot of suffering through our work, but one of the worst things I’ve ever seen is a child having seizures from cerebral malaria in Tanzania. I will never forget watching his small body twist in agony, as his parents waited to find out if he would survive. I wouldn’t wish that experience on anyone.
So why exactly are people more afraid of sharks than mosquitoes? The late Hans Rosling would argue that humans are hardwired to fear things that cause us physical harm. This instinct is practical if you live in poverty (on level 1 or 2), where an animal attack is more likely to kill you. But if you can afford life-saving healthcare, it can distort your perception of how significant a threat really is.
Even if you know that you’re 50,000 times more likely to get killed by a mosquito than a shark, human instinct wins out. A photo of a shark attack victim on the evening news evokes a visceral reaction, because the threat is obvious. A picture of a malaria victim in a hospital ward doesn’t trigger our fear instinct in the same way.
Despite this, I’m determined to spread the word about mosquitoes—which is why I’m bringing back Mosquito Week here on Gates Notes.
Everything I’m posting this week is dedicated to my least favorite pest. You can read some good news about a country that hopes to eliminate malaria by 2020. You can see how the bed nets the Mozambique Ministry of Health and World Vision distributed last year on behalf of the Gates Notes Insider community are making a difference. I’m going to be talking about mosquitoes on my social channels all week, and I hope you’ll join the conversation.
As long as Hollywood keeps making blockbusters about sharks, I’ll keep talking about why everyone should be more scared of a tiny bug than a 3,000-pound carnivore. Jaws is nothing compared with the flying terror that is a mosquito.
Covered
Net impact
Learn how a new, long-lasting mosquito net is helping save lives in the southern African country of Mozambique.

The world is making incredible progress against malaria. New innovations—including more effective drugs for treatment, rapid diagnostic tests, and better insecticides—have helped prevent more than 600 million cases of malaria and saved 6.8 million lives between 2000 and 2015. One new tool that helps protect families in Africa is a long-lasting type of bed net. Learn more about the impact these bed nets are having in the southern African country of Mozambique.
Fourteen-month-old Judite Luis battles malaria (and complications from malnutrition) at Chicuque Rural Hospital in Inhambane, Mozambique with her mother, Adozinda Augusta, at her side. Malaria is the leading cause of death among children under 5 in Mozambique. Judite died the day after this photo was taken.

A boy points out the holes in an old mosquito net used in his home. While the older generation of bed nets helped protect families from malaria in Mozambique, they had some downsides. They needed to be soaked in insecticide every six months and didn’t stand up to repeated washings when they got dirty, leading to tears that mosquitoes could fly through.

In November, thousands of families in Inhambane, Mozambique lined up to receive long-lasting insecticidal mosquito nets from the Mozambique Ministry of Health’s National Malaria Control Program and World Vision partnership. The nets protect people from mosquitoes for three years and can even be washed when they get dirty. (The bed net donation was made possible, in part, by the participation of Gates Notes readers in a bed net giveaway campaign last year. Thanks for your help!)

Clayton Pedro Albert, age 6, and his 11-month-old sister, Sharmila, go to bed under one of the long-lasting insecticidal nets. “There is no malaria in this house this year. Last year, it was so many times,” said Carolina Alberto, their mother. Across Mozambique, World Vision, in partnership with the Ministry of Health, has distributed more than 21 million bed nets. Ensuring families use their new bed nets is critical for controlling malaria. World Vision follows up with households to show families how to hang and care for their nets and remind them of the importance of sleeping under them every night.

Silvina Jorge Mahoche and her daughter, Celineza Mahoche, share their new insecticidal net. The Mahoche family has had malaria more times than they can remember. What they don’t forget are the painful symptoms: “A fever, chills, joint pain, headaches, and vomiting,” Silvina said. Since receiving the net last year, no one in the family has been sick from malaria.

Villagers return home after receiving new mosquito nets. Ensuring communities have universal coverage of nets and follow up to ensure appropriate use is critical to achieving malaria control and elimination. Some mosquitoes are now developing resistance to the pyrethroid insecticides used in bed nets—so researchers are working on next generation nets that use combinations of insecticides and appear effective against all mosquitoes, including insecticide-resistant ones. Much more work needs to be done to eliminate malaria in Africa, but continued innovation in bed nets and other tools will ensure that the world will continue to make progress against this deadly disease.

Beans & rice
Lunchtime in Africa
More than a meal: The humblest of school lunches can transform lives and entire nations.

Could a plate of beans and rice help change the world?
Last month, I squeezed into a child’s-size desk to have lunch with a class of primary school students in Tanzania. I was there to join them for the launch of their new school lunch program. On the menu: red beans cooked with tomatoes and onions served over rice.
You can join us in this video. (We’ve saved a plate for you.)
Lunch was delicious. More than that, it filled me with hope. Watching my 67 lunchmates—most of them 8-year-olds—dig into their piles of rice and beans, I was reminded that even the humblest of meals can have a far-reaching impact not just for individuals, but entire nations.
Here’s why: This month, as children around the globe begin another school year, millions of students in the poorest countries (and even some in wealthy countries) will turn up for classes on an empty stomach, making it difficult for them to learn and continue their schooling. According to the World Food Program, 66 million primary school-age children attend classes hungry across the developing world, with 23 million in Africa alone.
A school lunch program, however, can make a world of difference. It encourages kids to come to school, gives them energy to learn, and improves their overall health. The benefits don’t stop at the classroom door. Economic modelling shows that every US$1 invested in school meals programs brings a US$3-10 economic return from improved health, education and productivity. And a new research paper by the World Food Program found that school meals can contribute to help achieving the Global Goals, including ending hunger, quality education, and gender equality and indirectly to reducing poverty, contributing to the economy, and helping to reduce inequality.
Not too bad for a plate of beans and rice.
Stay tuned for more stories from my trip to Tanzania in the months ahead.
Bug zappers
Mosquito wars
The progress we’ve made to reduce malaria deaths is one of the most remarkable global health stories in recent years.

We’ve come a long way since the days of blaming the stars.
Malaria has terrorized humankind for thousands of years, but for most of that time, we had no idea what caused it. The ancient Greeks thought Sirius the dog star might be responsible. A Chinese medical text from 270 BCE speculated that three demons spread the disease. As recently as the mid-1800s, doctors believed malaria was caused by the stinky fumes that wafted into cities from nearby swamps (the word malaria means “bad air” in Italian).
Today, we know exactly who our enemy is: the mosquito. Doctors no longer subject malaria sufferers to unpleasant (and pointless) treatments like blood-letting and chewing tree bark. Most importantly, we’ve made massive progress in fighting a disease that as recently as 2000 killed nearly 870,000 people in a single year.
This progress is one of the most remarkable global health stories in recent years. Malaria claimed more than 429,000 lives last year, mostly in Africa and Southeast Asia. While that figure is still way too high, it represents a 50 percent reduction overall from the disease’s peak in the early 2000s. I don’t throw the word “miracle” around lightly, but that number is nothing short of miraculous.
How did we get here? I give credit to an unprecedented scale-up in global commitment and cooperation—malaria funding rose by 1,000 percent from 2000 to 2015. This money fueled a number of amazing scientific breakthroughs, enabled us to deliver them at scale, and focused more brainpower on improving both control and treatment efforts.
This October marks a decade since Melinda and I first called for eradicating malaria. It was a controversial move at the time, but the progress made since then has convinced many that this is a realistic goal (although some are still skeptical).
If I had known back in 2007 how much progress we would make in ten years, I would’ve been thrilled by how much we’ve cut the death rate. I’d also be impressed by how many insecticidal bed nets are now in use, how new treatments are helping people with the most severe cases of malaria, and how rapid diagnostic tests have made it easier to find and treat people. But it wouldn’t all be good news.
In 2007, I thought we’d have a long-lasting malaria vaccine by now. The WHO plans to begin pilot demonstration projects of a first-generation malaria vaccine in sub-Saharan Africa next year, although without a booster dose it only protects a child for less than six months. I’m hopeful that researchers will develop a next generation vaccine that offers much longer protection within the next 10 years, but a decade ago I was overly optimistic about where we’d be today.
There are still plenty of reasons to believe we can eradicate malaria, though. In the war against malaria and the mosquitoes who carry it, we’re already fighting on every front. Consider the wide array of innovations in development right now:
- New Insecticide-Treated Bed Nets: The older generation of bed nets needed to be soaked in a special insecticide solution every six months. The long-lasting nets we will distribute in Mozambique through our giveaway protect people from mosquitoes for three years and can even be washed when they get dirty. Unfortunately, some mosquitoes are now developing resistance to the pyrethroid insecticides used in these nets—so researchers are working on next generation bed nets that use combinations of insecticides and appear effective against all mosquitoes, including insecticide-resistant ones.
- Tackling Drug Resistance: In Southeast Asia, we’ve seen some types of the malaria parasite develop resistance to the drug combinations we use to cure and prevent the disease. If this drug resistance spread to Africa, it’d be a disaster. Fortunately, we have partners on the front lines finding ways to fight back. Watch this video about the amazing work one team of researchers is doing to combat drug resistance in Thailand:
- Disease Mapping: We know more today about where malaria is occurring than we have at any other point in history. Public health experts are combining anonymous data from mobile phone records with data on malaria incidence to track the movements of infected mosquitoes. That's super valuable, because it helps countries use their limited resources in places that have the highest disease burden.
- Eave Tubes: Many houses in hot climates have a gap between the roof and the walls to keep the inside cool. By sealing these gaps and inserting special tubes just below the roofline, air still flows into the house but keeps mosquitoes out with a mesh filter. Since the tubes are too high for children to reach them, the mesh can be coated with a high enough dose of insecticide to kill even insecticide-resistant mosquitoes.
- Genome Editing: Our foundation has invested a lot of money into editing the genetic code of mosquitoes. We’re still in the very early stages of development, but scientists are exploring whether this technique could one day render a small number of key mosquito species infertile or unable to carry the malaria parasite.
- Attractive Targeted Sugar Baits: Only female mosquitoes bite people, and they only do it when they’re breeding. The rest of the time, they rely on sugar for energy. These calendar-sized traps hang on the outside of homes and contain a minimum risk toxin that kills more than 95 percent of the mosquitoes that flock to their sweet scent without affecting pollinators. Trials are underway in Mali.
I think we will see an end to malaria in my lifetime. It’s a preventable and curable disease, and the public health community has already demonstrated that it’s possible to shrink the map and save lives. These new tools in the development pipeline will play a huge role in reaching our goal. While we’re still decades away from wiping malaria off the map for good, one thing is clear: the mosquito has met its match.
Loaf actually
The bread lab in my backyard
These Washington state researchers are doing cool things with baked goods.

I’ve been to lots of labs, but until recently I had never seen one that was centered on a full working kitchen. Last month I got my chance when I visited the Bread Lab, located a couple hours north of my hometown Seattle. It brings together local farmers, expert plant breeders, and world-class bakers with the goal of producing wheat for baked goods that are both delicious and good for you.
I could smell the baking bread the minute I walked in the door. Canisters of flour from different types of wheat lined the walls. Bakers were pulling warm rolls out of large commercial ovens. In the corner there was a farinograph, a machine that measures the strength of dough.
It was all very impressive. But deep down, I was a little skeptical: How would the breads actually taste? The Bread Lab emphasizes using whole grains, and not just wheat—lab director Steve Jones loves buckwheat because it’s unusually high in lysine and other nutrients. Although eating whole-grain bread might make me feel virtuous, in my experience it just never seems to taste as good as white bread.
But I got to sample lots of their baked goods, and I’m happy to report that everything I ate was delicious—even the croissants, which are especially hard to get right when you’re using whole grains.
The lab is part of Washington State University, and although most of their work is with rich-world companies including Clif Bar, La Brea Bakery, and Chipotle, they are also applying their expertise to the problem of malnutrition in poorer countries. For example, I met a Pakistani Ph.D. student, Farah Ahmad, who’s looking at ways to make chapatis, cookies, and other foods from her home country using approaches developed by the Bread Lab.
Here’s a video from my visit:
Beasts of the southern tropics
What cowboys can teach us about feeding the world
Could a cattle ranch in Australia improve food security in Africa?

Beyond breeding, Wylarah Station uses technology to ensure that their herds receive proper nutrition. I was surprised to see their ranch hands use smart watches to track how much the cows are drinking.
In the past someone had to manually inspect all of the water troughs scattered across the ranch, driving hundreds of kilometers every day. Now they receive a notification on their watch when a sensor detects that a tank needs attention. The whole operation was a far cry from the John Wayne cowboy movies I used to watch as a kid.
Not all of AACo’s innovative approaches could work in the poor world. It’s unlikely that every farmer in Africa will be wearing a smart watch anytime soon (if ever). But as smartphone usage continues to grow across the continent, it’s easy to imagine a future where Africans might use an app to order the perfect bull DNA or make sure their cattle are eating enough—something that an African ICT company called iCow is promoting in Kenya, Ethiopia, and Tanzania with help from our foundation.
Farmers across sub-Saharan Africa are already raising cattle—beef and dairy—in massive numbers. Ethiopia, Sudan, and Tanzania are among the world’s top 15 cattle producing countries. While there are legitimate questions about whether the world can meet its appetite for animal products without destroying the environment, it’s a fact that many poor people rely on cattle for both nutrition and income. I believe they should be able to raise cattle as efficiently as farmers in rich countries do.
I’m optimistic that technology can improve the quality of African cattle. A typical dairy cow in the United States produces nearly 30 liters of milk every day. Compare that to your average cow in Ethiopia, which produces just 1.69 liters of milk a day. If you want to increase milk yield, you can’t just take a high-producing Holstein cow from Wisconsin and drop it into the tropical savannah. Unlike indigenous breeds, temperate cattle have no natural resistance to tropical diseases—like trypanosomiasis, or sleeping sickness—and they struggle to get enough nutrition from local food sources.
Instead, you could breed cattle that will flourish in the local climate. That means using artificial insemination—like the process they use at Wylarah Station—to crossbreed a native female cow (with her built-in resilience to tropical heat and diseases) with a bull from a genetic line that produces lots of milk.
Our foundation is already tackling this, but AACo’s technology could make the process much more precise than it is today. One of the things that amazed me most during my visit was how much they know about the ancestry of their cattle. The animals on their ranch have a more detailed family history than most people do. If farmers in Africa were equipped with the same level of knowledge, they could handpick the best possible cow parents and breed a better calf. But that leads us to another problem.
Because they lack adequate storage, most African farmers rely on artificial insemination stations (yes, that’s what they’re really called) to provide sperm samples. Depending on how far a farmer lives from a station, the sample can sometimes heat up too much and effectively die before it is delivered. Many farmers decide not to take the risk. Instead they get their cows pregnant the old-fashioned way, which makes it harder to control genetic integrity and can lead to calves that are less resilient or produce less milk.
AACo is looking into methods that extend the viability of sperm samples. Similar technology is currently used in Europe to improve the success rate of fertilization, but it hasn’t been tried yet with tropical cattle. If successful, it could double the amount of time a sample can survive outside of storage and make it easier for more farmers across Africa to use artificial insemination.
Beyond breeding, Wylarah Station uses technology to ensure that their herds receive proper nutrition. I was surprised to see their ranch hands use smart watches to track how much the cows are drinking.
In the past someone had to manually inspect all of the water troughs scattered across the ranch, driving hundreds of kilometers every day. Now they receive a notification on their watch when a sensor detects that a tank needs attention. The whole operation was a far cry from the John Wayne cowboy movies I used to watch as a kid.
Not all of AACo’s innovative approaches could work in the poor world. It’s unlikely that every farmer in Africa will be wearing a smart watch anytime soon (if ever). But as smartphone usage continues to grow across the continent, it’s easy to imagine a future where Africans might use an app to order the perfect bull DNA or make sure their cattle are eating enough—something that an African ICT company called iCow is promoting in Kenya, Ethiopia, and Tanzania with help from our foundation.
There’s a lot we can learn from Wylarah Ranch about how to more efficiently raise cattle, but I can’t ignore the big question: should we rely on animals for food at all? Eating too much meat contributes to higher levels of obesity and heart disease, and raising animals contributes to climate change. That’s why I’ve invested in companies working on meat substitutes, which could one day eliminate the need to raise and slaughters animals entirely.
Although it might be possible to get people in richer countries to eat less, we can’t expect people in low income countries to follow suit. When I went vegetarian for a year in my late 20s, all I had to do to get my daily serving of protein was buy a can of beans or a container of tofu at the grocery store. It’s not so easy for families in poor communities to get the nutrition they need.
For them, meat and dairy are a great source of high-quality proteins that help children fully develop mentally and physically. Just 20 grams of animal protein a day can combat malnutrition, which is why our foundation’s nutrition strategy wants to get more meat, dairy, and eggs into the diets of children in Africa. Cattle are also a huge economic driver in some parts of Africa. In Ethiopia alone, cattle account for 45 percent of their agricultural GDP. In addition, livestock can actually contribute to ecosystems by stimulating pasture growth, enhancing biodiversity, and recycling energy and nutrients.
As more people in poor countries move into the middle class, they will likely eat more beef and drink more milk. But we can mitigate the impact of that growth on the environment by increasing production from the cows they already have. The cowboys of Wylarah Ranch have mastered the art of raising tropical cattle. I don’t know yet how African farmers can benefit from their expertise—our foundation is just starting to dig into this—but I’m excited about the possibilities.
Safety first
Foreign aid keeps Americans safe
The strategic case for fighting disease and poverty abroad.

You may have seen in the news that elected officials in Washington, D.C., are working on next year’s federal budget. One of the ideas that has been floated is to make deep cuts in foreign aid—the investments that America makes to help other countries fight poverty and disease.
That would be a big mistake.
For one thing, these programs amount to less than 1 percent of the federal budget. For anyone worried about the budget deficit, cutting 1 percent will not make a dent.
More importantly, these programs give American taxpayers a phenomenal return on investment, one of the best anywhere in government. They do this in three ways:
- Making Americans safer and the world more stable
- Creating jobs at home and promote trading partners that will buy American goods
- Saving lives and building up health systems so other countries can take better care of their people
Together these three points make what you might call the strategic case for aid—the argument that aid helps the countries that give it as well as those that receive it.
To be honest, the strategic case is not what prompted Melinda and me to get involved in this work more than 17 years ago. We were moved by what you could call the moral case: the idea that it is terribly unjust that people in poor countries—especially children—die of diseases that can be prevented. That is still the main thing that drives us today. But over the years we have come to see the compelling strategic case too. And we have found that people often support aid who aren’t convinced by the moral argument but are by the strategic one.
In this post I want to focus on point #1 above. I’ll come back to #2 and #3 in subsequent posts.
Let’s look at how promoting health and development keeps Americans safe.
Preparing for the next epidemicYou may remember the Ebola epidemic of 2014–16. It killed more than 11,000 people in three West African countries. Each of those deaths was a tragedy, but the epidemic could have been far worse. If it had spread to neighboring Nigeria, home to more than 180 million people and a busy international travel hub with daily flights to the world’s capitals, it would have been very hard to contain. It could have easily jumped the Atlantic and infected Americans, and spread throughout Europe or Asia.
Why didn’t that happen? One key reason is that a number of health workers were stationed in Nigeria as part of the global campaign to stamp out polio. As the Ebola epidemic took hold, they were quickly reassigned from polio to Ebola. They already had a system in place for identifying possible cases, tracking them, and reporting the data to people organizing the response. They helped contain the disease and keep it from spreading farther than it did.
The polio eradication program helped stop Ebola and saved countless people, including Americans. Its biggest public funder? The United States government.
In addition, Ebola may have been only a preview of what is to come. The next epidemic—say, a virulent flu as bad as the Spanish Flu of 1918—could be far worse. Epidemiologists estimate it could kill 30 million people, more than three times the population of New York City.
Funding from the U.S. government helps keep that from happening. It helps other countries strengthen their health systems so they can identify dangerous diseases and contain them before they get out of control.
It is no accident that the Ebola epidemic hit hardest in three countries—Guinea, Sierra Leone, and Liberia—with especially weak health systems. Helping them improve makes it more likely that we can prevent a worldwide epidemic that destabilizes entire regions of the world and kills tens of millions of people.
Stabilizing vulnerable countriesPreventing pandemics is one specific way that U.S. funding makes Americans safer. There is also a broader point here: by fighting poverty and disease, we make the world a more stable place.
For example, both evidence and common sense tell us that when people don’t have reliable food supplies, they will pick up and move someplace else—becoming migrants or refugees—and that leads to more instability. Look at the countries with the least reliable food supplies in the world: Sudan, South Sudan, Eritrea, Burundi. Each of them is either at war or recently emerged from conflict.
Syria is another tragic example. In 2007, the country suffered the worst drought in its history. More than 1 million people fled rural areas for the cities, where they hoped to find food. This migration stoked political tensions and created the foundation for the horrific civil war that continues today. Of course that war has many causes, and not every drought-stricken country will become another Syria. But it is clear that the world is not a safer place when more people are going hungry—and that when we strengthen food and farming systems, we tackle some of the root causes of migration and instability.
Improving health is another way to make countries more secure. One of my favorite all-time examples is PEPFAR, the program America launched in 2003 to stop the spread of AIDS. Today it provides life-saving medicine for more than 11 million people living with HIV in some of the world’s poorest countries. Those 11 million people are teachers, health-care workers, and police officers—people who build strong, self-sufficient societies. So it should not be surprising that in countries where PEPFAR has a presence, political instability fell by 40 percent between 2004 and 2013. In non-PEPFAR countries, it dropped only 3 percent. And the PEPFAR countries grew three times faster.
Shoring up national securityAmerican military leaders understand that fighting poverty and disease is part of a smart national-security strategy. It was true after World War II, when the United States invented modern development assistance to combat instability in Europe and prevent a third World War, and it’s true today. The more stable poor countries are, the lower the odds that America will need to intervene in them.
More than 120 retired generals and admirals recently wrote a letter to Congress arguing that U.S. aid programs “are critical to preventing conflict and reducing the need to put our men and women in uniform in harm’s way.” While he was the head of U.S. Central Command, overseeing American operations in Syria, Pakistan, Afghanistan, and elsewhere, Secretary of Defense James Mattis said: “If you don’t fully fund the State Department”—which houses many aid programs—“then I need to buy more ammunition.”
Aid is an important part of our broad diplomatic and security relationships. Out of 135 countries that receive some health or development aid from the United States, we have bilateral defense agreements with 131 of them.
These are some of the arguments I have been making in Washington on behalf of American aid. In future posts I will explain how aid not only keeps Americans safe, but also creates jobs in the United States and helps other countries become more self-sufficient. All reasons why I believe this money is well-spent and ought to be maintained.
Progress 360
Strong coffee, stronger women
How Ethiopia’s 38,000 health workers have helped save children’s lives and improved the health of their nation.

Of all the charts I’ve seen, this one is the most beautiful:
Why?
First, that descending red line captures one of the most amazing stories of human progress: It shows how the number of deaths of children under 5 per year has been cut in half since 1990.
Second, hidden along that line are millions of stories of the incredible work being done by health officials, governments, donors, and parents around the world to help save all those lives.
Here’s one of those stories. It begins with some remarkable women I met in Ethiopia. They are part of an innovative program that’s improved the health of millions of children in their country.
You can meet them yourself (and join us for a cup of coffee) in this video.
Back in 1990, Ethiopia had one of the highest rates of child mortality in the world. One in five children were dying before their 5th birthdays. With few doctors and most of its population living in rural areas, Ethiopia struggled to provide basic health services to the country. Most women in rural areas gave birth at home.
Then in 2000, the Ethiopian government made a commitment to improve its healthcare system. Ethiopia signed on to the United Nations’ Millennium Development Goals, which focused the world’s attention on fighting disease and ending poverty by using data to measure progress on health and development progress. As part of the goals, Ethiopia pledged to reduce under-five death rates by at least two-thirds by 2015.
To achieve it, Ethiopia needed to find an effective way to deliver healthcare to the remotest corners of the country. But training thousands of new doctors to staff them would take years and would be extremely costly. Instead, Ethiopia created a community health worker program. They selected thousands of people, primarily young women with at least a 10th grade education, and trained them in a set of basic health skills—including how to deliver babies, administer immunizations, and provide family planning support—that are proven to save lives. Most of the health workers were recruited from the communities they served, helping to quickly build public trust in the new effort.
In 2012, I made my first trip to Ethiopia to see the program in action for myself. I was amazed. I visited a remote health post south of Addis Ababa run by two health workers, Yetagesu Alemu and Betula Shemesie. They spent many of their days walking from door to door in their village caring for pregnant women and families with newborns. Their health post didn’t have electricity or any high tech medical equipment. Still, their efforts had made an impact on the health of the families in their community.
What was exciting to see was how this success was being repeated in villages across the country. Despite being one of the poorest countries in the world, Ethiopia managed to dramatically reduce the rate of child mortality. By 2012, Ethiopia had met the target for the Millennium Development Goal on child survival, with under-five death rates dropping by 66 percent since 1990.
One of the key reasons the program has been so effective is that the health workers are dedicated to measuring their progress. Covering nearly every square inch of the walls of the health post I visited were large charts, where the health workers would track births, immunizations, malaria cases, and other indicators. Each indicator helped them understand how well they were performing and which areas demanded more attention.
Today, Ethiopia has more than 15,000 health posts delivering primary health care to the farthest reaches of this rural country of 100 million people. The health posts are staffed by 38,000 health workers like Betula and Yetagesu.
Last summer, I had a chance to visit Ethiopia again. I caught up with Yetagesu and Betula over coffee and to learn more about how the health worker program was going. They told me how women who once delivered their babies at home were now choosing to give birth at health centers. Their communities also had access to ambulances that would pick up any woman who is ready to give birth. Yetagesu and Betula were also proud to report that they had received additional medical training to sharpen their health skills.
To be sure, there’s a lot more work to be done to improve health services in rural Ethiopia. Their communities need more ambulances. Just one vehicle serves 17 health posts, Yetagesu said. They also hoped the country would hire more health workers so they would have the time to provide families with more comprehensive services. And as Melinda and I discussed in this year’s annual letter, one of the biggest challenge in child survival is newborn deaths. In Ethiopia, about 44 percent of all childhood deaths occur within the first 28 days of life. We need to find innovative ways to solve this challenge.
Still, I’m confident that Ethiopia will continue to make progress in child survival. And what’s most exciting is that Ethiopia’s health program has been so successful that it now serves as a model for other countries to follow. Sharing lifesaving innovations like Ethiopia’s ensures that in the years ahead the most beautiful chart in the world will become even more beautiful.
A real bargain
How foreign aid helps Americans
It makes the country more secure, prevents epidemics, and saves lives.

Foreign aid is often in the hot seat, but today the heat is cranked up especially high. The United States government, one of the world’s most influential donors, is considering dramatic cuts to health and development programs around the world. I understand why some Americans watch their tax dollars going overseas and wonder why we’re not spending them at home. Here’s my answer: These projects keep Americans safe. And by promoting health, security, and economic opportunity, they stabilize vulnerable parts of the world.
This is a lesson I’ve learned myself. When I first got involved in health and development more than 15 years ago, the main motivation was to save and improve people’s lives around the world. That’s still true today, but over the years I have come to see the tangible ways in which American aid benefits Americans too.
For one thing, it helps prevent epidemics. The most recent Ebola outbreak in West Africa killed more than 11,000 people, but the death toll would have been much worse if the disease had spread widely in neighboring Nigeria, an international travel hub that’s home to 180 million people. What contained it? Among other things, a group of health workers who were stationed there for an anti-polio campaign. They were quickly reassigned to the Ebola fight, and their efforts helped stop the disease—and keep it from crossing the Atlantic to the United States.
The biggest public funder of anti-polio work has been the U.S. government, and for good reason. It is protecting Americans and helping us get ready for the next epidemic, which could be orders of magnitude deadlier than Ebola. To stop emerging diseases, we need the infrastructure built by consistent funding of well-run health programs.
Another example is America’s global HIV/AIDS effort, known as PEPFAR, which began under President George W. Bush and works with some of the world’s poorest countries. PEPFAR is an undeniable success. There are 11 million people with HIV who are alive today because of the medicines that it provides. Many more never got the virus in the first place because of prevention efforts supported by PEPFAR.
This is not simply a humanitarian accomplishment. For those countries it means more teachers, entrepreneurs, police officers, and health-care workers contributing to strong, stable societies. According to one bipartisan study, political instability and violent activity in African countries with PEPFAR programs dropped 40 percent between 2004 and 2015. Where there was no PEPFAR program, the decline was just 3 percent.
Better health puts nations on the path to self-sufficiency. How? When health improves, people decide to have fewer children, because they’re confident that the children they do have will survive into adulthood. As family size drops, it gets easier for countries to feed, educate, and provide opportunity for their people—and that is one of the best ways to stabilize any vulnerable region.
A more stable world is good for everyone. But there are other ways that aid benefits Americans in particular. It strengthens markets for U.S. goods: of our top 15 trade partners, 11 are former aid recipients. It is also visible proof of America’s global leadership. Popular support for the U.S. is high in Africa, where aid has such a dramatic impact. When you help a mother save her child’s life, she never forgets. Withdrawing now would not only cost lives, it would create a leadership vacuum that others would happily fill.
Syria is a tragic example of what can happen when the key ingredients of stability don’t come together. Beginning in 2007, the country experienced the worst drought in its history, driving more than a million people from rural areas into the cities, stoking political tension, and laying the foundation for the horrific civil war that continues today. Of course there were many causes of that war, and not every country that has a severe drought collapses as badly as Syria did. But the world will not be a safer place if the U.S. stops helping other countries meet their people’s needs.
None of this is lost on our military leaders. More than 120 retired generals and admirals recently wrote a letter to Congress arguing that U.S. programs “are critical to preventing conflict and reducing the need to put our men and women in uniform in harm’s way.” Secretary of Defense James Mattis famously said, back when he was commander of U.S. forces in Afghanistan, Pakistan, and other hotspots: “If you don’t fully fund the State Department”—which runs many of America’s key programs—“then I need to buy more ammunition.”
Protecting Americans, preventing epidemics, strengthening markets, saving lives: aid delivers phenomenal benefits, and for a bargain. It represents less than 1 percent of the federal budget, not even a penny out of every dollar. It is some of the best return on investment anywhere in government. This money is well spent, it has an enormous impact, and it ought to be maintained.
This post originally appeared on time.com.
Future investment
Preparing for the next epidemic: a first step
A new organization will help accelerate the development of vaccines we’ll need to contain future outbreaks.

At a time when world leaders are understandably focused on terrorism and other security threats, another enemy is being largely overlooked—the next epidemic.
We don’t know when the next pathogen will emerge, what it will be, how it will spread, or who will be affected, but we do know that the world is not prepared to deal with it. That was the tough lesson that Ebola (and the Zika outbreak since) taught us. Ebola claimed thousands of lives, caused billions of dollars in economic losses, and showed how vulnerable our society is to epidemics of infectious diseases. As I’ve written about before, the world lacks an effective system to detect, respond to, or prevent the next outbreak.
That’s why I’m excited this week, at the World Economic Forum in Davos, to participate in the launch of a new organization that will help the world get ready for future epidemics. Backed by the governments of Norway, India, Japan, and Germany, along with the Wellcome Trust and our foundation, the Coalition for Epidemic Preparedness Innovations (CEPI) will invest in innovations to accelerate the development of vaccines we’ll need to contain outbreaks.
CEPI’s focus on vaccine development is a critical part of getting prepared for whatever pathogens threaten us next. We know from the world’s defeat of smallpox and its successful fights against polio, measles, and other diseases that vaccines are incredibly effective tools for preventing disease and saving lives. Now, this alliance of governments, philanthropies, vaccine manufacturers, academia, NGOs, and other partners needs to work together to develop new vaccines to make the world safe from future epidemics.
Traditional approaches to making new vaccines are too slow to respond to a sudden disease outbreak. Currently, the development of a new vaccine, including testing and deployment, is a process that can typically take more than 10 years. Fast-moving epidemics don’t allow us to be that patient. In 1918, an extremely infectious and deadly strain of the flu infected about one-fifth of the world’s population and killed at least 30 million people in less than two years. Ebola and Zika were also both frightening viruses, but the way they are transmitted—through bodily fluids and mosquitoes—helped limit their spread globally. A highly-contagious airborne disease would pose a far greater threat. It would thrive in densely populated urban areas and could easily cross national borders and oceans by air travel.
My great hope for CEPI is that it will help enable the world to produce safe, effective vaccines as quickly as a new threat like this emerges. With $460 million in initial funding, CEPI will work to bring together the most advanced vaccine technologies and resources from the private and public sector that can help lead to new breakthroughs in vaccine development. CEPI’s vaccine development strategy includes two areas of focus: “just in time” vaccines for those currently unknown pathogens that will emerge, and “just in case” vaccines for pathogens that we know are at high risk of causing another outbreak, like Ebola and Middle East respiratory syndrome or MERS.
One promising area of vaccine development research is using advances in genomics to map the DNA and RNA of pathogens and make vaccines. The vaccines can be decoded by human cells to make their own vaccines and antibodies inside the body. If successful, this technology could dramatically reduce the development timeline from years to possibly months or weeks.
What’s exciting about these new technologies is that they wouldn’t just protect us from future epidemics. They also would help us to develop vaccines for existing health threats to hundreds of millions of people around the world, including HIV, malaria, and TB.
At the same time, CEPI will work to minimize regulatory hurdles that further delay the deployment of vaccines. CEPI will fund studies to evaluate these newly-developed vaccines and build vaccine stockpiles before epidemics begin, so countries can move swiftly to full vaccine efficacy trials and emergency deployment during an outbreak.
As pleased as I am to see CEPI’s work get underway, it’s important for everyone to understand that this effort is just the first step toward getting us prepared for the next epidemic. It’s an important step, but CEPI alone won’t be enough to protect us. We have a lot more work to do.
We need a global warning and response system for outbreaks. It begins with strengthening local health systems in poor countries, which have gotten hit the hardest during recent epidemics. The thousands of remote health clinics around the world will be the backbone of our global effort to defeat future epidemics. They must have trained health workers who can provide primary health care, deliver vaccines, and monitor the health of their communities.
We must have a better disease surveillance system, which includes a global database so countries can share information on cases. We also need trained medical personnel ready to mount a rapid response to an outbreak.
Last, we need to continue to invest in health research to develop not just vaccines, but also new drugs and diagnostic tests that will strengthen our ability to respond quickly and effectively to the next epidemic.
Still, we’ll never know exactly when a new disease outbreak will emerge. It could arrive tomorrow, next month, next decade, or next century. But that uncertainty shouldn’t be an excuse for inaction. I hope that today’s announcement marks the first of many steps the world will take to get prepared for the next epidemic. All of our futures depend on it.
HIV’s Deadly Partner
Let’s make TB history
By investing in R&D, I know it will be possible to discover new innovations that will make TB a disease of the past.

I visited South Africa earlier this year to learn more about the progress the country is making in the fight against HIV. I toured health clinics, met with doctors and researchers, and listened to the stories of people living with HIV. Again and again, our conversations turned to an often forgotten disease which is HIV’s lethal partner: tuberculosis.
Tuberculosis, or TB, is an infection of the lungs that kills about 1.8 million every year, including 400,000 people with HIV and TB. Historically, TB was dubbed “consumption” because it caused such severe weight loss that the disease appeared to “consume” its patients.
Together, HIV and TB form a deadly duo. HIV weakens the immune system, which makes it susceptible to TB infection and much harder for the body to fight the disease. Last year, about one-third of people living with HIV were also infected with TB bacteria, and about 35 percent of deaths among HIV-positive people were due to TB. Worldwide, South Africa has the largest number of people infected with TB and HIV.
Since 2000, better testing and treatment programs have helped drive down TB deaths by more than 20 percent, saving tens of millions of lives. But a new World Health Organization report found that the TB epidemic is larger than previously estimated. New surveillance and survey data revealed hundreds of thousands of new cases, the bulk of them in India. In 2015, there were an estimated 10.4 million new TB cases worldwide, up from 9.6 million cases in 2014. The WHO report also found that of the 10.4 million people with TB, 4.3 million of them did not receive quality care because of significant gaps in testing, treatment, and reporting of TB by health providers. TB deaths climbed to 1.8 million, up from 1.6 million in 2014.
One of the key concerns among health officials fighting TB is the rising threat of drug resistance, something I learned about during a previous visit to South Africa. New strains of the disease have emerged that do not respond to the most commonly used drug treatments available. Treating people with drug-resistant TB is complicated and costly. It also places incredible hardships on the patients who must undergo months of treatment using drugs which are toxic and have serious side-effects.
Last year, Simbongile, a young mother living outside of Cape Town, learned she was infected with drug-resistant TB and started the difficult road to recovery. Her story is heartbreaking, but she is among the lucky ones. In 2015, nearly 600,00 people fell ill from drug resistant TB treatment worldwide. Just 1 in 5 received treatment.
While the impact of drug-resistant TB is a serious problem, the vast majority of TB cases are drug sensitive, meaning they can be cured effectively with medicines so long as they are taken properly. Drug resistance emerges because of incorrect prescriptions by health providers, low-quality drugs, and patients stopping treatment prematurely. That’s why the best way to prevent drug resistance is to improve TB testing and treatment programs for drug-sensitive cases.
TB, like so many other diseases, primarily impacts the world’s poorest people. If you live in a wealthy country, it might be easy to think, as many people do, that TB is a disease of the past. That fact is reflected in the lack of funding for TB programs around the world. In 2016, global support for TB care and prevention fell $2 billion short of the $8.3 billion needed.
Stories like Simbongile’s, however, are a powerful reminder that TB is still an active threat and the world is in dire need for new innovations to prevent and treat it. By investing more in research and development, I know it will be possible to create a new generation of TB drugs and develop a new and effective TB vaccine.
TB is not a disease of the past, but if the world works together to fight it, I have no doubt it can be.
So Long, Sucker
Mapping the end of malaria
Defeating the world’s deadliest creature and the terrible disease it carries is one of the greatest success stories in global health.

A few years ago, I pulled off a purposeful prank. While I was giving a TED Talk on malaria to a room full of influential people, I opened a canister and let loose a small swarm of mosquitoes. “There’s no reason that only poor people should have the experience,” I said. I let the audience squirm in their seats for about half a minute before I let on that the mosquitoes were not infected with malaria. My gimmick worked. A distant problem suddenly got very close to home.
Today, gimmicks are no longer necessary for convincing Americans of the danger of mosquito-borne diseases. The spread of Zika virus in south Florida, Puerto Rico, and other parts of the U.S. has given millions of Americans a direct understanding what it’s like to live with the fear of mosquitoes and the harm they can do, especially to pregnant women and children.
The world must focus serious attention and resources on ending the Zika epidemic. At the same time, we should keep in mind that the overwhelming toll of mosquito-related illness and death comes from malaria. Malaria is the key reason mosquitoes are the deadliest animal in the world.
Over the years, I have been in hospitals in several African countries when malaria is at its peak. I’ve seen beds out in the corridors and two children to a bed. There’s nothing more painful to see than a child experiencing cerebral malaria, when the parasite is attacking the brain and causing horrible seizures. As a parent, these memories will stay with me for life.
That’s why it gives me great joy to share a new report published todayin The New England Journal of Medicine. Rigorous new data show that the malaria death rate in sub-Saharan Africa has declined by a stunning 57% since 2000. With almost 500,000 children still dying of malaria every year, we obviously have a long way to go. But cutting the death rate by more than half is a miracle. It’s one of the greatest success stories in the history of global health.
We’ve known for some time that malaria deaths have been declining steeply. The significance of this new study, which was produced by the Institute for Health Metrics and Evaluation, is that we now have the strongest evidence ever of just how steep the decline has been.
This progress on malaria is no accident. It’s the result of an unprecedented increase in focus and commitment by rich and poor countries alike. The amount of money available to pay for bed nets, effective medications, and malaria research rose by 1,000 percent from 2000 to 2015, fueling massive new prevention and control efforts in countries hit hard by malaria.
In Tanzania, a country that has led the way with a major scale-up, the mortality rate fell more than 80 percent from 2000 to 2015. I remember visiting Tanzania years ago during the rainy season and seeing overflowing hospitals. When I went back years later, there were almost no children in the wards.
Tanzanian health authorities have launched major campaigns to distribute insecticide-treated bed nets and encourage people—especially children—to sleep under them every night. They’ve done widespread spraying of insecticides inside homes and in urban ponds, puddles, and marshes where mosquitoes breed. And they’ve used great medications that contain a drug called artemisinin, which earned its discoverer, Youyou Tu, the 2015 Nobel Prize in Medicine. If you take three days’ worth of these pills, you can get rid of the malaria parasites in your bloodstream, which helps you and also stops you from being the source of malaria spreading back to other people.
And now we have an awesome new tool in our arsenal: precision malaria maps. In the same New England Journal article I mentioned above, the authors report on cutting-edge mapping efforts that have given us an ability to see at a very high degree of granularity (5 km by 5 km) the burden of malaria in sub-Saharan Africa. That’s super valuable for short-term interventions, like helping a country determine where to deploy health staff. It’s just as valuable for long-term efforts to reduce the rate of transmission and shrink the malaria map.
When you zoom in with these high-definition maps, you can quickly home in on the hot spots where malaria is hitting hard and yet existing tools like bed nets are not being used widely enough. These maps show that in most countries it’s actually a very small percentage of the country where the disease burden is high and you need to focus your interventions.
And here’s more good news: After years of investment, we now have better diagnostics for detecting infections in people who show no physical symptoms (because people who are infected with malaria parasites but don’t show signs of illness are a big part of the chain of transmission). We have helped private-sector companies develop new, safe insecticides that will allow us to preserve the gains we have made against malaria. We have also helped bring to market simple technologies to protect families from mosquitoes, such as “eave tubes” that kill mosquitoes trying to enter homes and new traps which exploit mosquitoes’ attraction to sugar to kill them outdoors.
As a result of all this progress, I am confident that we can pursue the end goal of not just shrinking the malaria map but wiping malaria off the map altogether. Last year, Ray Chambers, the UN Secretary General’s special envoy for malaria, and I put forward a concrete plan for eradicating the disease by 2040. The potential upside is enormous: 11 million lives and $2 trillion dollars of economic impact. And the alternative to eradication—controlling the disease forever without eliminating it—is biologically and politically untenable. It would require endless investment in the development of new drugs and insecticides just to stay one step ahead of disease resistance. I also believe it would be impossible to maintain strong political commitment to fighting malaria unless we can define a clear end point. History has shown that unless countries rid themselves of malaria altogether, they eventually see the disease come roaring back on a massive scale.
To achieve eradication by 2040, we’ll need several other key innovations under development to come to fruition.
First, we’ll need new classes of drugs that completely clear malaria parasites from the body with just one dose. We should have these new cures in about a decade.
Second, we need new tools that can prevent malaria transmission. This can either be done with an effective malaria vaccine or by reducing mosquito populations. We will soon have a first-generation vaccine, but it protects a child for less than six months without a booster dose. I’m betting that within the next 10 years, researchers can produce a vaccine that provides much longer protection.
We have another potential game-changer in the works. Our foundation is supporting scientists who are using a powerful new tool called “genome editing” to introduce genetic changes in the Anopheles gambiae species of mosquito, one of the most effective transmitters of malaria in Africa. These genetic edits cause females to produce mostly male, sterile offspring. In theory, scientists could drive this trait throughout entire populations of mosquitoes in much of Africa, dramatically reducing malaria transmission in a very short time. While I’m excited about the potential of this technology, I know that changing the mosquito genome in a permanent way is something that should be done only with incredible caution and care. My hope is that it will be possible to deploy some version of this technique in a safe manner within 10-12 years.
In 1999, Melinda and I made our first major investment in malaria—a grant to establish the Malaria Vaccine Initiative. Funding for malaria research was so diminished at the time that we nearly doubled the resources with that one single grant. That blew my mind.
Today, this is no longer a lonely fight. More than 50 countries have joined together to mobilize billions of dollars through The Global Fund. And these resources are coming not just from wealthy countries. African countries such as Benin, Côte d’Ivoire, Kenya, Namibia, Nigeria, Senegal, South Africa, Togo, and Zimbabwe are contributing as well. In fact, African countries are now, for the first time ever, mobilizing more of their own resources for malaria than they’re receiving from donors.
So the next time you hear skeptics charging that foreign aid doesn’t work, point to malaria. Foreign assistance has not chased away local resources. On the contrary, it’s encouraged African nations to step up their own health efforts. And the results have been nothing short of remarkable.
360⁰ of Connection
South Africa: Virtually There
Travel with me to South Africa to see how the country is hoping to win the fight against AIDS.

If you could shuffle all of the homes in the world like a deck of cards so that people in wealthy countries lived side by side with people from poor countries, it would transform the world’s fight against poverty, hunger, and disease. It would be impossible for people to look away, impossible for them not to help.
I was naïve about the deep poverty in the world until I took my first trip to Africa with Melinda in 1993. Seeing the disparities with our own eyes made all the difference and inspired us to start our foundation.
Since then, I’ve continued to travel regularly to Africa, India, and other parts of the developing world. I always return from my trips humbled and inspired. My one disappointment is that I wish everyone could have seen what I did. I have no doubt it would help more people become aware of the challenges the world’s poorest people face. It would also leave them as optimistic as I am about the incredible progress the world is making in health and development.
During my trip to South Africa in July, I tried something new that I hope will allow people to experience what I have. I had highlights of my visit recorded in virtual reality. It’s still an emerging technology but what excites me about it is that it allows viewers to immerse themselves in another world. You can look up and down. Turn right or left. Listen to sounds all around you. I used to think there was no substitute to being there and seeing things for yourself. But virtual reality is a close second. It fulfills my dream of allowing people to see what I’m seeing and, perhaps, feel what I’m feeling, too.
In this video, you will hear the stories of young women living with HIV. Sit beside me as I drive from the leafy suburbs of Johannesburg to the dusty township of Soweto. Feel what it’s like to be in the center of a stomping gumboot dancing troupe. And be inspired by the power of South Africa’s youth, who will drive the next generation of innovations to create a future free of AIDS.
If you want to know more about my trip to South Africa, you can read about my visit here and here. I also encourage you to learn more about The Global Fund, which has helped provide lifesaving treatment to millions of people living with HIV.
Thanks for watching and look out for more virtual reality videos in the months ahead.

Status Check
We Haven’t Turned the Corner on AIDS
Why we need to invest more in the fight.

Next week I’ll be traveling to Durban, South Africa, to attend the International AIDS Conference. It’s an important opportunity for members of the AIDS community to discuss our ongoing efforts to fight the disease. I’ll be there to listen and learn. But I’ll also be delivering my own message.
The good news is that the fight against AIDS has seen many successes. The infection rate declined for several years and millions of people have been put on treatment, allowing them to live full, productive lives.
But we have not turned the corner. The infection rate has essentially stopped declining. That’s a particular problem in sub-Saharan Africa, which has a growing population of young people, who are most susceptible to the disease. If the infection rate stays the same while the at-risk population rises, then the number of people in sub-Saharan Africa who contract HIV each year could start going up instead of down.
One reason the infection rate has stagnated is that AIDS funding has stagnated. Another reason is that the current prevention tools have not had as much impact as any of us had hoped. Voluntary medical male circumcision is a very effective prevention approach, but the programs offering the procedure have not been scaled up sufficiently to reach all those who would benefit. The newest tool, using AIDS treatment as a way to prevent HIV infection among healthy people, has not been rolled out fast enough, and asking people to take a pill every day for prevention presents its own challenges.
There is the idea of “treatment as prevention”: Treating people who have HIV not only saves their life, it also makes them much less likely to pass the virus along to others. This is a promising approach and certainly we should treat as many people as possible so we can save their lives. But it is not yet clear to me that it is financially feasible to treat enough people to get a large prevention effect. I hope to learn more about this question at the conference next week.
For all these reasons, we need to invest more in both delivering the best prevention tools we have and developing new ones that are even more effective. For example, researchers are working on prevention and treatment tools that last for several months after a single dose, which would make it easier for people to stick to the regimes. I am also optimistic that within a decade we will have an AIDS vaccine that provides an acceptable level of protection.
In this video, I explain what it will take to make the most of these opportunities and ensure that AIDS cases keep going down:
17 Million Saved
Let’s preserve this lifesaver
Why we need to keep supporting the Global Fund.

Let me cut to the chase. There’s a program that has helped save the lives of 17 million people in poor countries since 2002. It’s called the Global Fund to Fight AIDS, TB, and Malaria. It’s poised to do even more good in the years ahead, but to continue its work, it needs donors to make new funding pledges.
I just got back from Europe, which is starting to think through many tough decisions surrounding Brexit. Despite that challenge, the governments of France and Italy became the latest to make commitments to the Global Fund, building on recent pledges from Japan, Canada, the United States, and the European Commission. When I was in London, a senior member of the British government confirmed to Parliament that they remain committed to the Global Fund’s success. Although I’m confident the Global Fund will raise the money it needs—donors have consistently recognized that it’s an effective and low-cost way to save lives—we are not there yet.
Since the Global Fund started, Melinda and I have committed $1.6 billion to it. Here are four reasons why we are such big believers:
- Saving lives. In countries where the Global Fund operates, deaths from HIV, TB, and malaria have dropped by a third since 2002. Certainly the Fund doesn’t deserve sole credit for that phenomenal progress, but it has played an irreplaceable role. And its work is far from finished: Three million people still die every year from these diseases.
- Getting rid of diseases so we never have to fight them again. In my lifetime I expect to see the end of malaria, which kills nearly half a million children every year. When you eradicate a disease, you not only save lives, you free up billions of dollars and many hours of effort. One reason I’m so optimistic about ending malaria is the work of the Global Fund, which has slowed the spread of the disease and saved lives by distributing hundreds of millions of bed nets.
- Helping poor countries become more self-sufficient. If you ever hear people say “poor countries just keep getting foreign aid forever,” tell them about the Global Fund. It helps the countries it works with improve their health systems so they can take better care of their people. They also devote an increasing share of their own budgets to health (they have promised to spend 50 percent more between 2015 and 2017 than they did in the previous three years). That translates into less spending by rich governments.
- Using aid efficiently. The Fund has a done a great job keeping costs low and streamlining its work. Its operating costs are just over 2 percent of all the grants it gives out. That means the vast majority of the money that flows through the Global Fund is reaching the people who need it most.
The Global Fund raises money in three-year batches; the current batch will cover the years 2017-19. They’re asking for $13 billion, which will go toward delivering lifesaving drugs and bed nets as well as developing new tools like better diagnostics and next-generation prevention techniques. To put that number in context, it’s about 3 percent of the total foreign aid that rich countries give over three years. And consider the payoff: By one estimate, the $13 billion raised by the Global Fund will generate about $300 billion in economic benefits.
It is never easy to raise large sums of money like this, and it certainly isn’t easy now, with the refugee crisis in Europe compounding an already difficult global economy. Although I don’t think anyone would argue that fighting disease will directly end wars or stop the flow of refugees, improving health certainly makes countries more stable and more prosperous—and less likely to spread disease and instability to their neighbors.
If you want to save and improve lives, health is one of the most effective investments you can make. And if you want to improve health, the Global Fund is one of the most effective investments you can make. It is one of the kindest things people have ever done for one another, and I am inspired by the countries and leaders who are stepping up to support it.
Innovation Nation
America’s secret weapon
By investing in R&D, the U.S. creates jobs at home and helps people around the world.

This presidential election has the country captivated. As many commentators have pointed out, the primaries are more focused on personalities than policy. While the parties focus on who is going to represent them in the fall, I want to make the case for something that I hope every candidate will agree on in November: America’s unparalleled capacity for innovation. When the United States invests in innovation, it creates companies and jobs at home, makes Americans healthier and safer, and saves lives and fights poverty in the world’s poorest countries. It offers the next president a tremendous opportunity to help people in America and around the world.
Of course, America’s capacity for innovation is nothing new. We have been inventing for more than two centuries: think of Benjamin Franklin, Margaret Knight, Thomas Edison. By the end of World War II, the United States led the world in automobiles, aerospace, electronics, medicine, and other areas. Nor is the formula for success complicated: Government funding for our world-class research institutions produces the new technologies that American entrepreneurs take to market.
What is new is that more countries than ever are competing for global leadership, and they know the value of innovation. Since 2000, South Korea’s R&D spending (measured as a percentage of GDP) has gone up 90 percent. China’s has doubled. The United States’ has essentially flatlined. It’s great that the rest of the world is committing more, but if the U.S. is going to maintain its leading role, it needs to up its game.
I have seen first-hand the impact that this type of research can have. I was lucky enough to be a student when computers came along in the 1960s. At first they were very expensive, so it was hard to get access to them. But the microchip revolution, made possible by U.S. government research, completely changed that. Among other things it enabled Microsoft, the company I co-founded, to write software that made computers an invaluable tool for productivity. Later, the Internet—another product of federal research—changed the game again. It is no accident that today most of the top tech companies are still based in the United States, and their advances will have a massive impact in every area of human activity.
My favorite example is health. America’s investment in this area creates high-paying jobs at universities, biotech companies, and government labs. It leads to new treatments for disease, such as cancer therapies. It helps contain deadly epidemics like Ebola and Zika. And it saves lives in poor countries. Since 1990, the fraction of children who die before age 5 has fallen by more than half. I think that’s the greatest statistic of all time, and the United States deserves a lot of credit for making it happen.
The next few years could bring even more progress. With a little luck we could eradicate polio, a goal that is within reach because of vaccines developed by U.S. scientists. (Polio would be the second disease ever eradicated, after smallpox in 1979—in which the U.S. also played an irreplaceable role.) There is also exciting progress on malaria: The number of deaths dropped more than 40 percent from 2000 to 2012, thanks in part to America’s support for breakthrough tools like drugs and bed nets. But to make the most of these opportunities, we need to invest more in basic health research and specific areas like vaccines.
Energy is another great example. American-funded research defines the state of the art in energy production. Early advances in wind and solar technology were developed with federal money. And this research offers a strong return on investment. Between 1978 and 2000, the Department of Energy spent $17.5 billion (in today’s dollars) on research on efficiency and fossil fuels, yielding $41 billion in economic benefits. Yet until this year, the DOE’s research budget hadn’t seen a real increase since the Reagan administration.
If we step up these investments, we can create new jobs in the energy sector and develop the technologies that will power the world—while also fighting climate change, promoting energy independence, and providing affordable energy for the 1.3 billion poor people who don’t have it today. Some of the more promising areas include making fuel from solar energy, much the way plants do; making nuclear energy safer and more affordable; capturing and storing carbon; and creating new ways to store energy that let us make the most of renewables.
There’s a lot of momentum right now on clean energy research. Last year the leaders of 20 countries, including the United States, committed to double federal investments in this area. Complementing that crucial effort, I helped launch the Breakthrough Energy Coalition, a group of private investors who will back promising clean-energy companies. The next president will have a chance to accelerate this momentum.
Investing in R&D isn’t about the government picking winners and losers. The markets will do that. It’s about doing what we know works: making limited and targeted investments to lay a foundation for America’s entrepreneurs. This approach has been fundamental to U.S. leadership for decades, and it will become only more important in the years ahead.
By the end of this summer, the political parties will have chosen their leaders and will start looking ahead to the November election. The nominees will lay out their vision for America and their agenda for achieving it. These visions will probably have more differences than similarities. But I hope we can all agree that, no matter how you see America’s future, there will always be an essential role for innovation.
This article was originally published by Reuters News Agency.
Lessons From Ebola
We’re not ready for the next epidemic
We’re not ready for it. But we can get there.

I am in Vancouver this week attending the TED conference. I just gave a brief talk on a subject that I’ve been learning a lot about lately—epidemics.
The Ebola outbreak in West Africa is a tragedy—as I write this, more than 10,000 people have died. I’ve been getting regular updates on the case counts through the same system we use to track new cases of polio. Also, last month I was lucky enough to have an in-depth discussion with Tom Frieden and his team at the Centers for Disease Control and Prevention in Atlanta.
What I’ve learned is very sobering. As awful as this epidemic has been, the next one could be much worse. The world is simply not prepared to deal with a disease—an especially virulent flu, for example—that infects large numbers of people very quickly. Of all the things that could kill 10 million people or more, by far the most likely is an epidemic.
But I believe we can prevent such a catastrophe by building a global warning and response system for epidemics. It would apply the kind of planning that goes into national defense—systems for recruiting, training, and equipping health workers; investments in new tools; etc.—to the effort to prevent and contain outbreaks.
This is what my TED talk was about. You can watch it here:
The more I learn about what it takes to respond to an epidemic, the more impressed I am by the health workers who have been risking their lives to care for the sick. Just putting on a protective suit is huge undertaking. Once it’s on, it’s hard to hear what anyone else is saying, and you start to sweat after just a few minutes.
Here’s a short photo essay about one attempt to solve this problem that I was involved with.
At TED we also put together an exhibit where attendees could try on a suit for themselves:
Finally, if you’re interested in learning more, you might want to check out this op-ed I wrote for the New York Times. And if you are willing to read a little more (okay, a lot more), here is a longer paper I wrote for the New England Journal of Medicine.
Melinda and I remain committed to improving the health of the poorest 2 billion. The good news is, many of the steps required to save lives in poor countries—such as strengthening health systems—also improve the world’s ability to deal with epidemics. So I’m optimistic that we can solve this problem. Making the right investments now could save millions of lives.
An Anti-Viral Campaign
Hard questions about the next epidemic
I hit the road to talk about preventing epidemics. Here’s what I heard.

Normally when I post here on TGN, give a speech, or write an op-ed, I’m out to share good news about how the world is getting better. But last month I made an exception. In a TED talk, an op-ed in the New York Times, and a longer paper in the New England Journal of Medicine, I wanted to highlight a sobering fact: The world is not prepared to handle a major epidemic. I shared a few thoughts about what it might take to get ready, based on lessons from the Ebola epidemic in West Africa.
I was curious to hear people’s feedback on my suggestions, so it was great to meet in Berlin with a group of health experts from governments, non-profits, and pharmaceutical companies, and then with U.S. senators in Washington, D.C. In this post, I want to share a few of the things I heard.
There is general agreement that this is a big challenge. Everyone I talked to, politicians and technical experts alike, felt strongly that the world isn’t doing enough to prepare. There is also broad agreement about what to do: we need to create a global alert and response system for epidemics.
As we got into the details, though, we ran into some tough issues.
For example, I argued that in a severe epidemic, the military has to play a role. It’s the only group that can quickly move large numbers of people and equipment in and out of an affected area. But in my conversations in D.C., it became clear that the U.S. military is not chartered for this work and doesn’t prepare for it, which meant that in West Africa they were learning on the fly.
In addition, what happens when there’s an outbreak in a region where people see the army—whether it’s domestic or foreign—as the bad guy? Some NGO leaders and health workers worry that being associated with armed forces could put them in harm’s way by making them a target.
This is one of the toughest issues that came up and it deserves more discussion. At a minimum I think we need a diverse set of military groups from different countries ready to help. And we can take steps to make it clear that troops are on a humanitarian mission, for example by running simulations in different countries so citizens can see what they’re up to.
Another big topic was drug trials. In an epidemic you want to develop and test new treatments very quickly. But how do you make that happen when the usual drug-approval process takes years? Should there be an emergency regulator who decides which drugs to test, how to test them quickly, and whether to deploy one? Should (and can) they indemnify whoever is producing the drug to protect them from lawsuits?
All these conversations raised a larger issue that is fascinating to me: How should the world get ready for rare, potentially cataclysmic events? When an epidemic strikes, we will want the best health and logistics experts ready to spring into action. But which group has the budget to maintain that kind of spare capacity? Even more importantly, how do we get brilliant people to sit around waiting for an event that has a small chance of occurring in any given year?
The closest analogy I can think of is the military, where troops might go years at a time without seeing combat. They use training exercises and war games to stay sharp. I think we should be doing something similar—germ games—for epidemics.
What happens next? Even though the experts mostly agree on the broad strokes of what should be done, I don’t know whether the world will choose to put meaningful resources into this effort. But I am hopeful that it will happen. The group I joined in Berlin is providing input to German Chancellor Angela Merkel and the G7 group of wealthy countries as they think about how they can help solve this problem. Creating a global plan would help more nations see how they can contribute and hopefully draw them in. The United Nations and WHO are also looking at various steps that could improve their ability to respond. And at the Gates Foundation we’re talking about how we might be able to assist.
It is great to see this issue rising up the global agenda. The world isn’t ready yet for a serious epidemic, but I think we have a good chance to make real progress in the next few months.
Well Suited
Arming doctors to fight Ebola
As I learned recently, it’s one thing to find a new tool that will help the people fighting this deadly disease. Getting it to them is another story.

Getting new tools into the hands of the people fighting Ebola is much harder than it needs to be. I have experience with one alarming example.
Health workers in protective suits get so hot that they have a hard time caring for their patients. (For example your goggles fog up and you sweat profusely.) I asked a team of experts who work on technology for keeping vaccines cold to refocus on keeping the medical workers cool.

Within days, the team had found an existing solution: a vest with pockets where you could insert cooling packs.
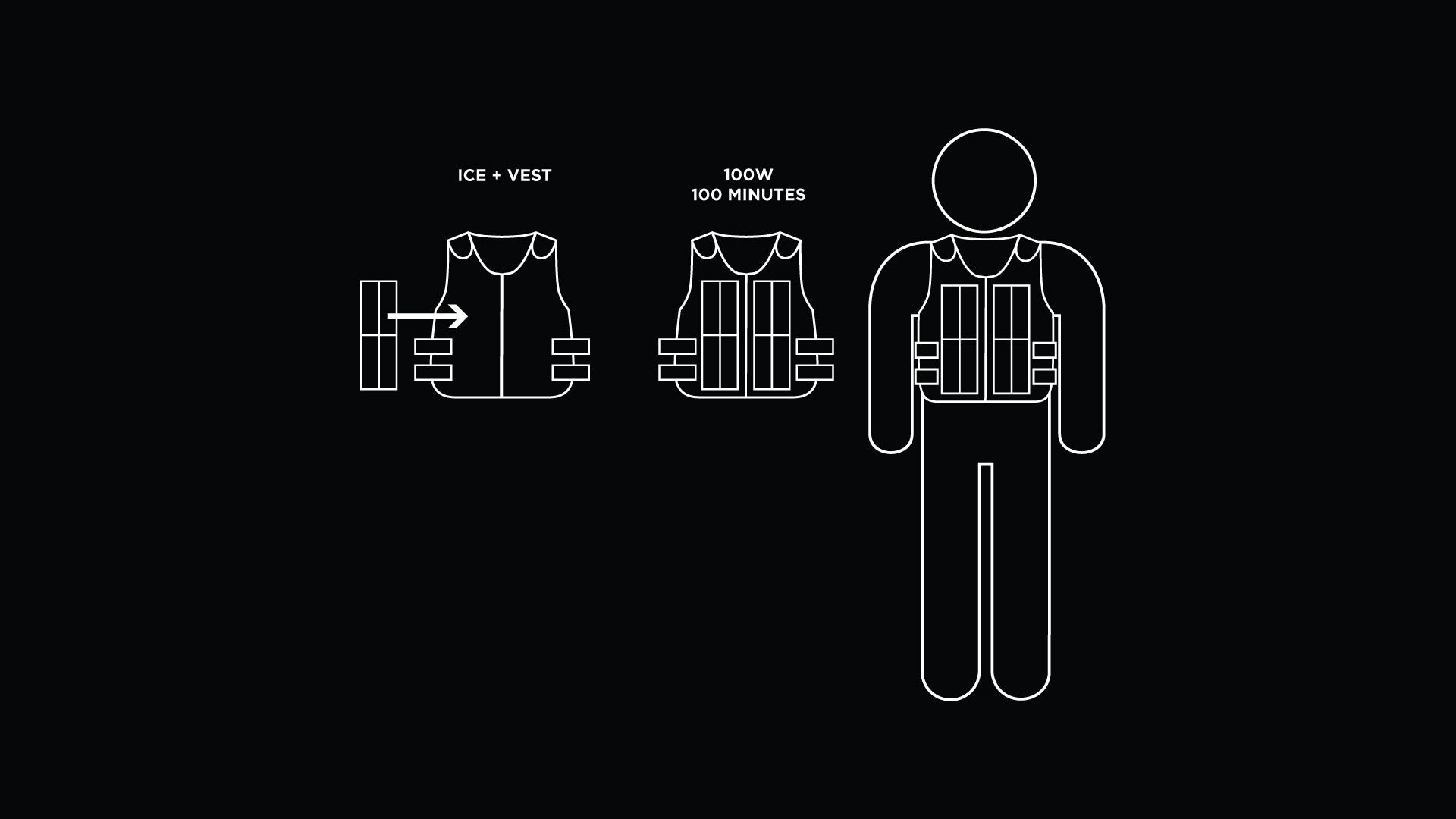
Doctors who had treated Ebola patients in West Africa helped test and improve these cooling vests. Here you see Dr. Colin Bucks of Stanford University testing a vest and suit at home while under quarantine after working in Liberia. He rode a stationary bike to simulate the heat of West Africa.

Unfortunately, there was no coordinated system for getting the vests to West Africa. The team had to create new distribution channels by working directly with treatment centers in the region. They eventually got the suits to over a thousand health workers.

Although this wasn’t a critical issue, it is just one example of the challenge of preparing for a highly infectious disease. We see similar breakdowns in detecting outbreaks early, training and deploying volunteers, coordinating with the military, and more. But I’m optimistic that if we start now and stay focused, we can get ready for the next epidemic.

Dino-Might
How dinosaurs could help us fight malnutrition
Research on ancient reptiles may help us understand how children grow.

Kids love dinosaurs. When you’re three feet tall and can’t have dinner unless somebody brings you food, the idea of enormous, powerful creatures that have fangs to defend themselves and claws to capture their own meals seems pretty great.
I loved dinosaurs as much as anyone, but eventually I grew tall enough to get my own dinner, and my interest in dinosaurs waned.
My friend Nathan Myhrvold, though, never stopped loving dinosaurs. Actually, there are a lot of things Nathan never stopped loving—he’s published best-selling cookbooks and essays on bioterrorism, among other things—but if you ask him about his longest-running obsession, he’ll tell you it’s dinosaurs. His office is full of dinosaur bones, some of which he dug up himself, along with a model of a dinosaur whose tail moved so fast it broke the sound barrier.

Because he’s so curious, Nathan can take what he knows about these great reptiles and apply it to fields that seem completely unrelated—fields like childhood nutrition, one of the most important and misunderstood areas in all of development.
Here’s a short video in which he explains the connection:
Dinosaur growth rates, it turns out, are hard to study. There may be only thirty fossils of a particular dinosaur species in the world, and none of them may be complete. So how do you know whether a bone is shaped a certain way because that’s how triceratops grew or whether your particular specimen just had a funny-looking head?
In poor countries, children’s physical development is also hard to study, though for different reasons. For one thing, measurements are notoriously inaccurate. If you’re measuring a crying, squirming baby who doesn’t want a cold tape measure pressed up against his body, you might not get the numbers exactly right. There’s also a host of reasons a child could be short. Is this girl short because she’s malnourished? Is she from a short family? Or has she just not hit her growth spurt yet?
What that means is that in both areas, dinosaur growth and childhood growth, you end up with problematic data; with children, it’s messy, and with dinosaurs, it’s sparse. In both cases, though, the problem is the same: looking at the data from the wrong angle gives you the wrong answers.
Nathan thinks he’s figured out a systematic way to look at the growth records from the right angle. Since we started working with him he’s shared some promising ideas about how to measure children’s growth accurately, analyze the trends, and take action on the analysis. For example, some researchers recently looked at the relationship between gross domestic product and childhood stunting and, to everyone’s surprise, they found no correlation—until Nathan pointed out that they were using the wrong statistical methods to analyze the information. The methods he suggested instead—based on his work on dinosaurs—showed that the relationship was actually even stronger than many people in the field had thought. And that could have a big impact on how policymakers and health-care workers approach the problem of childhood nutrition.
This is a great example of a trend I hope we’ll see a lot more of: taking scientific advances from lots of different fields and using them to solve problems in global health.
Ever since dinosaurs were discovered, kids have showered them with love. Thanks to this work, we may have found a way for dinosaurs to pay them back.
Spending Pennies, Saving Lives
The Miracle of Vaccines
Vaccines, one of the best investments you can make for improving health.

Imagine there’s an infectious disease spreading through your community. It leaves some people crippled; others die from it. Then someone comes along and says: “Here’s something that will protect you from this disease for the rest of your life. You and your family can have it, for free.” You would be very relieved, right?
This scenario may seem hypothetical (though perhaps less so given how much the Ebola virus has been in the news). But it is very real for millions of people in the world’s poorest countries. Vaccines that were once out of reach for them are being delivered in greater numbers every year. That means more parents are feeling the relief of knowing their families are protected.
I’ve been looking at some of the data on vaccines and thought I would share what I’m seeing. At a time when so many news headlines are grim, it is inspiring stuff.
I’ll start with polio. Cases are down more than 99 percent since 1988. Earlier this year, we celebrated a fantastic achievement: India was declared polio-free. And in Nigeria, the number of polio cases is at an all-time low, just 6 so far this year versus more than 50 by this time last year. It’s one of only three countries that have never been polio free (the others are Pakistan and Afghanistan).
Wherever we make progress on polio, it’s a testament to the amazing work of many people: political leaders who prioritize stopping the disease, donors who help fund the effort, and—most importantly—the health workers who doggedly go from house to house to deliver vaccines. Thanks to all this work (and with a little luck), 2015 could be the first time Nigeria goes a year without a case of wild poliovirus, and the first time all of Africa is polio-free. If we maintain this commitment, I’m quite optimistic that by 2018 we will get rid of this crippling disease, everywhere, forever.
There’s also fantastic progress in delivering basic immunizations for diseases like measles and pneumonia. The impact is phenomenal: By next year, the public-health group known as Gavi, the Vaccine Alliance will have helped prevent 3.9 million deaths. And expanding vaccine coverage over the next five years can save as many as 6 million lives and unlock more than $100 billion in economic benefit.
Along those lines, we hit a big milestone in September. With the addition of South Sudan, pentavalent vaccine—which protects against five debilitating diseases—has now been introduced in all 73 countries that get financial support from Gavi. Pentavalent replaced a vaccine that protected against only three diseases, which means kids are protected from more diseases without getting any extra shots. This would never have happened without Gavi: By negotiating with manufacturers and bringing in new suppliers, it drove down the cost of pentavalent vaccine from $30 per dose in rich countries to just $1.19 for poor countries.
Another big step has been the rollout of a vaccine for rotavirus, which causes severe diarrhea. Rotavirus is one of the reasons Melinda and I first got involved in global health; in the late 1990s, we were shocked by a newspaper article that said it killed 800,000 children a year—nearly all of them in poor countries—more than almost any other disease. After more research, we decided rotavirus should be a focus of our giving. We’re gratified to see that 65 countries are now rolling out rotavirus vaccines, and more are signing up. Manufacturers in India are working on a new vaccine and talking about exporting it to other countries, which would help save even more children.
We’re also getting closer to solving some big delivery problems, like the fact that many vaccines spoil if they get too warm. Researchers are field-testing a specially designed container that keeps vaccines cold for a month or more, using just a single batch of ice and no electricity. These trials are helping thousands of African children get immunized. I’m very hopeful that containers like this one will eventually help health workers reach far more people.
A Ripple Effect
Vaccines save lives, which is reason enough to make sure they get out there. But that’s not their only benefit. Healthy children spend more time in school, and they learn better while they’re there. When health improves, poor countries can spend more on schools, roads, and other investments that drive growth, which makes them less dependent on aid.
Vaccines deliver all this for, in some cases, just pennies per shot. That’s why I say that if you want to save and improve lives around the world, vaccines are a fantastic investment.
How You Can Help
One way you can help is to ask your political leaders to support Gavi next year, when donor governments need to renew their commitments. In the United States you can do that through Shot@Life, whose website makes it easy to send a message to your representatives.
You can also help by donating to Shot@Life. For $20, you can help protect a child from pneumonia, diarrhea, polio, and measles. And Shot@Life has teamed up with Walgreens for a “Get a shot. Give a shot” program: Get a vaccine at Walgreens and they will provide one for a child in a poor country.
This is flu season in the United States, so you may already be planning to get immunized. Why not help out someone else while you’re at it?
On the Front Lines of an Epidemic
“Your blood tested positive for Ebola. I am sorry.”
A Nigerian doctor’s harrowing account of outlasting the deadly virus.

Once in a while, you read something that’s so compelling, you want to share it with everyone you can. Dr. Ada Igonoh’s story had that effect on me.
Dr. Igonoh is a physician in Lagos, Nigeria, where she helped care for Patrick Sawyer, the patient who introduced Ebola into Nigeria in July. After coming down with the deadly virus herself, she spent two harrowing weeks getting treatment in isolation wards.
When I met her at a conference in New Orleans last week, Dr. Igonoh handed me a written account of her experience. Even knowing she was going to be okay, I couldn’t stop reading—I had to know what happened next. Her optimism was inspiring. Her story also gave me a deeper appreciation for all the health workers who are heroically caring for patients and trying to stop this epidemic. And it is a good reminder of the way uncertainty reigns in the early days of an epidemic. The world’s response since then has been remarkable, and Nigeria has now been certified free of Ebola.
I want to thank Dr. Igonoh for her courage, and for agreeing to let me share her story here. It is well worth your time to read it. — Bill Gates
On the night of Sunday July 20th, 2014, Patrick Sawyer was wheeled into the emergency room of the First Consultants Medical Centre, Obalende, Lagos, with complaints of fever and body weakness. The male doctor on call admitted him as a case of malaria, and took a full history.

Knowing that Mr. Sawyer had recently arrived from Liberia, the doctor asked if he had been in contact with an Ebola patient in the last couple of weeks, and Mr. Sawyer denied any such contact. He also denied attending any funeral ceremony recently. Blood samples were taken for full blood count, malaria parasites, liver function test, and other baseline investigations. He was admitted into a private room and started on antimalarial drugs and analgesics. That night, the blood count result came back as normal and not indicative of infection.
The following day, however, his condition worsened. He barely ate any of his meals. His liver function test result showed his liver enzymes were markedly elevated. We then took samples for HIV and hepatitis screening.
At about 5:00 p.m. he requested to see a doctor. I was the doctor on call that night, so I went in to see him. He was lying in bed with his intravenous (IV) fluid bag removed from its metal stand and placed beside him. He complained that he had stooled about five times that evening and that he wanted to use the bathroom again.
I picked up the IV bag from his bed and hung it back on the stand. I told him I would inform a nurse to come and disconnect the IV so he could conveniently go to the bathroom. I walked out of his room and went straight to the nurses' station where I told the nurse on duty to disconnect his IV. I then informed my consultant, Dr. Ameyo Adadevoh, about the patient's condition, and she asked that he be placed on some medications.
The following day, the results for HIV and hepatitis screening came out negative. As we were preparing for the early morning ward rounds, I was approached by an ECOWAS [Economic Community of West African States] official who informed me that Patrick Sawyer had to catch an 11 o'clock flight to Calabar for a retreat that morning. He wanted to know if it would be possible. I told him it wasn't, as he was acutely ill. Dr. Adadevoh also told him the patient could certainly not leave the hospital in his condition. She then instructed me to write very boldly on his chart that on no account should Patrick Sawyer be allowed out of the hospital premises without the permission of Dr. Ohiaeri, our Chief Medical Consultant. All nurses and doctors were duly informed.
During our early morning ward round with Dr. Adadevoh, we concluded that this was not malaria, and that the patient needed to be screened for Ebola Viral Disease. She immediately started calling laboratories to find out where the test could be carried out. She was eventually referred to Professor Omilabu of the LUTH Virology Reference Lab in Idi-Araba, whom she called immediately.
Prof. Omilabu told her to send blood and urine samples to LUTH straightaway. She tried to reach the Lagos State Commissioner for Health but was unable to contact him at the time. She also put calls across to officials of the Federal Ministry of Health and National Centre for Disease Control.
Dr. Adadevoh at this time was in a pensive mood. Patrick Sawyer was now a suspected case of Ebola, perhaps the first in the country. He was quarantined, and strict barrier nursing was applied with all the precautionary measures we could muster. Dr. Adadevoh went online, downloaded information on Ebola, and printed copies which were distributed to the nurses, doctors and ward maids. Blood and urine samples were sent to LUTH that morning. Protective gear, gloves, shoe covers and facemasks were provided for the staff. A wooden barricade was placed at the entrance of the door to keep visitors and unauthorized personnel away from the patient. Despite the medications prescribed earlier, the vomiting and diarrhea persisted. The fever escalated from 38°C to 40°C.
On the morning of Wednesday, 23rd July, the tests carried out in LUTH showed a signal for Ebola. Samples were then sent to Dakar, Senegal for a confirmatory test. Dr. Adadevoh went for several meetings with the Lagos State Ministry of Health. Thereafter, officials from the Lagos State came to inspect the hospital and the protective measures we had put in place.
The following day, Thursday 24th July, I was again on call. At about 10:00 p.m. Mr. Sawyer requested to see me. I went into the newly created dressing room, donned my protective gear and went in to see him. He had not been cooperating with the nurses and had refused any additional treatment. He sounded confused and said he received a call from Liberia asking for a detailed medical report to be sent to them. He also said he had to travel back to Liberia on a 5:00 a.m. flight the following morning and that he didn't want to miss his flight. I told him that I would inform Dr. Adadevoh. As I was leaving the room, I met Dr. Adadevoh dressed in her protective gear, along with a nurse and another doctor. They went into his room to have a discussion with him, and as I heard later to reset his IV line which he had deliberately removed after my visit to his room.
At 6:30 a.m., Friday 25th July, I got a call from the nurse that Patrick Sawyer was completely unresponsive. Again I put on the protective gear and headed to his room. I found him slumped in the bathroom. I examined him and observed that there was no respiratory movement. I felt for his pulse; it was absent. We had lost him.
It was I who certified Patrick Sawyer dead. I informed Dr. Adadevoh immediately and she instructed that no one was to be allowed to go into his room for any reason at all. Later that day, officials from WHO came and took his body away. The test in Dakar later came out positive for Zaire strain of the Ebola virus. We now had the first official case of Ebola virus disease in Nigeria.
It was a sobering day. We all began to go over all that happened in the last few days, wondering just how much physical contact we had individually made with Patrick Sawyer. Every patient on admission was discharged that day and decontamination began in the hospital. We were now managing a crisis situation.
The next day, Saturday 26th July, all staff of First Consultants attended a meeting with Prof. Nasidi of the National Centre for Disease Control, Prof. Omilabu of LUTH Virology Reference Lab, and some officials of WHO. They congratulated us on the actions we had taken and enlightened us further about the Ebola Virus Disease. They said we were going to be grouped into high risk and low risk categories based on our individual level of exposure to Patrick Sawyer, the "index" case. Each person would receive a temperature chart and a thermometer to record temperatures in the morning and night for the next 21 days. We were all officially under surveillance. We were asked to report to them at the first sign of a fever for further blood tests to be done. We were reassured that we would all be given adequate care. The anxiety in the air was palpable.
The frenetic pace of life in Lagos, coupled with the demanding nature of my job as a doctor, means that I occasionally need a change of environment. As such, one week before Patrick Sawyer died, I had gone to my parents' home for a retreat. I was still staying with them when I received my temperature chart and thermometer on Tuesday, 29th of July. I could not contain my anxiety. People were talking about Ebola everywhere—on television, online, everywhere.

I soon started experiencing joint and muscle aches and a sore throat, which I quickly attributed to stress and anxiety. I decided to take malaria tablets. I also started taking antibiotics for the sore throat. The first couple of temperature readings were normal. Every day I would attempt to recall the period Patrick Sawyer was on admission—just how much direct and indirect contact did I have with him? I reassured myself that the contact with him was quite minimal. I completed the anti-malarials but the aches and pains persisted. I had loss of appetite and felt very tired.
On Friday, 1st of August, my temperature read a high 38.7°C. As I type this, I recall the anxiety I felt that morning. I could not believe what I saw on the thermometer. I ran to my mother's room and told her. I did not go to work that day. I cautiously started using a separate set of utensils and cups from the ones my family member were using.
On Saturday, 2nd of August, the fever worsened. It was now at 39°C and would not be reduced by taking paracetamol. This was now my second day of fever. I couldn't eat. The sore throat was getting worse. That was when I called the helpline and an ambulance was sent with WHO doctors, who came and took a sample of my blood. Later that day, I started stooling and vomiting. I stayed away from my family. I started washing my plates and spoons myself. My parents, meanwhile, were convinced that I could not have Ebola.
The following day, Sunday, 3rd of August, I got a call from one of the doctors who came to take my sample the day before. He told me that the sample which they had taken was not confirmatory, and that they needed another sample. He did not sound very coherent and I became worried. They came with the ambulance that afternoon and told me that I had to go with them to Yaba. I was confused. Couldn't the second sample be taken in the ambulance like the previous one? He said a better-qualified person at the Yaba Centre would take the sample. I asked if they would bring me back. He said "yes." Even with my symptoms, I did not believe I had Ebola. After all, my contact with Sawyer was minimal. I only touched his IV fluid bag just that once without gloves. The only time I actually touched him was when I checked his pulse and confirmed him dead, and I wore double gloves and I felt adequately protected.
I told my parents I had to go with the officials to Yaba and that I would be back that evening. I wore a white top and a pair of jeans, and I put my iPad and phones in my bag.
A man opened the ambulance door for me and moved away from me rather swiftly. Strange behavior, I thought. They were friendly with me the day before, but that day, not so. No pleasantries, no smiles. I looked up and saw my mother watching through her bedroom window.
We soon got to Yaba. I really had no clue where I was. I knew it was a hospital. I was left alone in the back of the ambulance for over four hours. My mind was in a whirl. I didn't know what to think. I was offered food to eat but I could barely eat the rice.
The ambulance door opened and a Caucasian gentleman approached me but kept a little distance. He said to me, "I have to inform you that your blood tested positive for Ebola. I am sorry."
I had no reaction. I think I must have been in shock. He then told me to open my mouth and he looked at my tongue. He said it was typical Ebola tongue. I took out my mirror from my bag and took a look and was shocked at what I saw. My whole tongue had a white coating, looked furry, and had a long, deep ridge right in the middle. I then started to look at my whole body, searching for Ebola rashes and other signs, as we had been recently instructed. I called my mother immediately and said, "Mummy, they said I have Ebola, but don't worry, I will survive it. Please go and lock my room now; don't let anyone inside and don't touch anything." She was silent. I cut the line.
I was taken to the female ward. I was shocked at the environment. It looked like an abandoned building. I suspected it had not been in use for quite a while. As I walked in, I immediately recognized one of the ward maids from our hospital. She always had a smile for me but not this time. She was ill and looked it. She had been stooling a lot, too. I soon settled into the corner and looked around the room. It smelled of feces and vomit. It also had a characteristic Ebola smell to which I became accustomed. Dinner was served—rice and stew. The pepper stung my mouth and tongue. I dropped the spoon. No dinner that night.
Dr. David, the Caucasian man who had met me at the ambulance on my arrival, came in wearing his full protective hazmat suit and goggles. It was fascinating seeing one live. I had only seen them online. He brought bottles of water and ORS, the oral fluid therapy, which he dropped by my bedside. He told me that 90 percent of the treatment depended on me. He said I had to drink at least 4.5 litres of ORS daily to replace fluids lost in stooling and vomiting. I told him I had stooled three times earlier and taken Imodium tablets to stop the stooling. He said it was not advisable, as the virus would replicate the more inside of me. It was better, he said, to let it out. He said good night and left.
My parents called. My uncle called. My husband called crying. He could not believe the news. My parents had informed him, as I didn't even know how to break the news to him.
As I lay on my bed in that isolation ward, strangely, I did not fear for my life. I was confident that I would leave that ward some day. There was an inner sense of calm. I did not for a second think that I would be consumed by the disease.
That evening, the symptoms fully kicked in. I was stooling almost every two hours. The toilets did not flush, so I had to fetch water in a bucket from the bathroom each time I used the toilet. I then placed another bucket beneath my bed for the vomiting. On occasion, I would run to the toilet with a bottle of ORS, so that as I was stooling, I was drinking.
The next day, Monday, 4th of August, I began to notice red rashes on my skin, particularly on my arms. I had developed sores all over my mouth. My head was pounding so badly. The sore throat was so severe I could not eat. I could only drink ORS. I took paracetamol for the pain. The ward maid across from me wasn't doing so well. She had stopped speaking. I couldn't even brush my teeth; the sores in my mouth were so bad. This was a battle for my life but I was determined I would not die.
Every morning, I began the day with reading and meditating on Psalm 91. The sanitary condition in the ward left much to be desired. The whole Ebola thing had caught everyone by surprise. Lagos State Ministry of Health was doing its best to contain the situation but competent hands were few. The sheets were not changed for days. The floor was stained with greenish vomitus and excrement. Dr. David would come in once or twice a day and help clean up the ward after chatting with us. He was the only doctor who attended to us. There was no one else at that time. The matrons would leave our food outside the door. They hardly entered in the initial days. Everyone was being careful. This was all so new. I could understand, was this not how we ourselves had contracted the disease? Mosquitoes were in our room until they brought us mosquito nets.
Later that evening, Dr. David brought another lady into the ward. I recognized her immediately as Justina Ejelonu, a nurse who had started working at First Consultants on the 21st of July, a day after Patrick Sawyer was admitted. She was on duty on the day Patrick reported that he was stooling. While she was attending to him that night, he had yanked off his drip, letting his blood flow almost like a tap onto her hands. Justina was pregnant and was brought into our ward bleeding from a suspected miscarriage. She had been told she was there only on observation. The news that she had contacted Ebola was broken to her the following day after results of her blood test came out positive. Justina was devastated and wept profusely—she had contracted Ebola on her first day at work.
My husband started visiting but was not allowed to come close to me. He could only see me from a window at a distance. He visited so many times. It was he who brought me a change of clothes and toiletries and other things I needed because I had not even packed a bag. I was grateful I was not with him at home when I fell ill or he would most certainly have contracted the disease. My retreat at my parents' home turned out to be the instrumentality God used to shield and save him.
I drank the ORS fluid like my life depended on it. Then I got a call from my pastor. He had been informed about my predicament. He called me every single day, morning and night, and he would pray with me over the phone. He later sent me a CD player, CDs of messages on faith and healing, and Holy Communion packs through my husband. My pastor, who also happens to be a medical doctor, encouraged me to monitor how many times I had stooled and vomited each day and how many bottles of ORS I had consumed. We would then discuss the disease and pray together. He asked me to do my research on Ebola since I had my iPad with me, and told me that he was also doing his study. He wanted us to use all relevant information on Ebola to our advantage. So I researched and found out all I could about the strange disease that had been in existence for 38 years. My research, my faith, and my positive view of life, the extended times of prayer, study and listening to encouraging messages boosted my belief that I would survive the Ebola scourge.
There are five strains of the virus, and the deadliest of them is the Zaire strain, which was what I had. But that did not matter. I believed I would overcome even the deadliest of strains. Infected patients who succumb to the disease usually die between 6 to 16 days after the onset of the disease from multiple organ failure and shock caused by dehydration. I was counting the days and keeping myself well-hydrated. I didn't intend to die in that ward.
My research gave me ammunition. I read that as soon as the virus gets into the body, it begins to replicate really fast. It enters the blood cells, destroys them and uses those same blood cells to aggressively invade other organs where they further multiply. Ideally, the body's immune system should immediately mount up a response by producing antibodies to fight the virus. If the person is strong enough, and that strength is sustained long enough for the immune system to kill off the viruses, the patient is likely to survive. If the virus replicates faster than the antibodies can handle, however, further damage is done to the organs. Ebola can be likened to multi-level, multi-organ attack, but I had no intention of letting the deadly virus destroy my system. I drank more ORS. I remember saying to myself repeatedly, "I am a survivor, I am a survivor."
I also found out that a patient with Ebola cannot be re-infected and they cannot relapse back into the disease as there is some immunity conferred on survivors. My pastor and I would discuss these findings, interpret them as it related to my situation and pray together. I looked forward to his calls. They were times of encouragement and strengthening. I continued to meditate on the Word of God. It was my daily bread.
Shortly after Justina came into the ward, the ward maid, Mrs. Ukoh, passed on. The disease had gotten into her central nervous system. We stared at her lifeless body in shock. It was a whole 12 hours before officials of WHO came and took her body away. The ward had become the house of death. The whole area surrounding her bed was disinfected with bleach. Her mattress was taken and burned.
To contain the frequent diarrhea, I had started wearing adult diapers, as running to the toilet was no longer convenient for me. The indignity was quite overwhelming, but I did not have a choice. My faith was being severely tested. The situation was desperate enough to break anyone psychologically. Dr. Ohiaeri also called us day and night, enquiring about our health and the progress we were making. He sent provisions, extra drugs, vitamins, Lucozade, towels, tissue paper; everything we needed to be more comfortable in that dark hole we found ourselves. Some of my male colleagues also had been admitted to the male ward two rooms away, but there was no interaction with them. We were saddened by the news that Jato, the ECOWAS protocol officer to Patrick Sawyer, who had also tested positive, had passed on days after he was admitted.
Two more females joined us in the ward; a nurse from our hospital and a patient from another hospital. The mood in the ward was solemn. There were times we would be awakened by the sudden, loud cry from one of the women. It was either from fear, pain mixed with the distress, or just the sheer oppression of the isolation.
I kept encouraging myself. This could not be the end for me. Five days after I was admitted, the vomiting stopped. A day after that, the diarrhea ceased. I was overwhelmed with joy. It happened at a time I thought I could no longer stand the ORS. Drinking that fluid had stretched my endurance greatly.
I knew countless numbers of people were praying for me. Prayer meetings were being held on my behalf. My family was praying day and night. Text messages of prayers flooded my phone from family members and friends. I was encouraged to press on. With the encouragement I was receiving, I began to encourage the others in the ward. We decided to speak life and focus on the positive.
I then graduated from drinking only the ORS fluid to eating only bananas, to drinking pap and then bland foods. Just when I thought I had the victory, I suddenly developed a severe fever. The initial fever had subsided four days after I was admitted, and then suddenly it showed up again. I thought it was the Ebola. I enquired from Dr. David, who said fever was sometimes the last thing to go, but he expressed surprise that it had stopped only to come back on again. I was perplexed.
I discussed it with my pastor, who said it could be a separate pathology and possibly a symptom of malaria. He promised he would research if indeed this was Ebola or something else. That night as I stared at the dirty ceiling, I felt a strong impression that the new fever I had developed was not as a result of Ebola but malaria. I was relieved. The following morning, Dr. Ohiaeri sent me an antimalarial medication, which I took for three days. Before the end of the treatment, the fever had disappeared.
I began to think about my mother. She was under surveillance along with my other family members. I was worried. She had touched my sweat. I couldn't get the thought off my mind. I came across a tweet by WHO saying that the sweat of an Ebola patient cannot transmit the virus at the early stage of the infection. The sweat could only transmit it at the late stage.
That settled it for me. It calmed the storms that were raging with me concerning my parents. I knew right away it was divine guidance that caused me to see that tweet. I could cope with having Ebola, but I was not prepared to deal with a member of my family contracting it from me.
Soon, volunteer doctors started coming to help Dr. David take care of us. They had learned how to protect themselves. Among the volunteer doctors was Dr. Badmus, my consultant in LUTH during my housemanship days. It was good to see a familiar face among the care-givers. I soon understood the important role these brave volunteers were playing. As they increased in number, so did the number of shifts increase and subsequently the number of times the patients could access a doctor in one day. That allowed for more frequent patient monitoring and treatment. It also reduced care-giver fatigue. It was clear that Lagos State was working hard to contain the crisis.
Sadly, Justina succumbed to the disease on the 12th of August. It was a great blow and my faith was greatly shaken as a result. I commenced daily Bible study with the other two female patients and we would encourage one another to stay positive in our outlook, though in the natural it was grim and very depressing. My communion sessions with the other women were very special moments for us all.
On the 10th day in the ward, the doctors having noted that I had stopped vomiting and stooling and was no longer running a fever, decided it was time to take my blood sample to test if the virus had cleared from my system. They took the sample and told me that I shouldn't be worried if it comes out positive as the virus takes a while before it is cleared completely. I prayed that I didn't want any more samples collected from me. I wanted that to be the first and last sample to be tested for the absence of the virus in my system. I called my pastor. He encouraged me and we prayed again about the test.
On the evening of the day Justina passed on, we were moved to the new isolation centre. We felt like we were leaving hell and going to heaven. We were conveyed to the new place in an ambulance. It was just behind the old building. Time would not permit me to recount the drama involved with the dynamics of our relocation. It was like a script from a science fiction movie. The new building was cleaner and much better than the old building. Towels and nightwear were provided on each bed. The environment was serene.
The following night, Dr. Adadevoh was moved to our isolation ward from her private room where she had previously been receiving treatment. She had also tested positive for Ebola and was now in a coma. She was receiving IV fluids and oxygen support and was being monitored closely by the WHO doctors. We all hoped and prayed that she would come out of it. It was so difficult seeing her in that state. I could not bear it. She was my consultant and my mentor. She was the imperial lady of First Consultants, full of passion, energy and competence. I imagined she would wake up soon and see that she was surrounded by her First Consultants family but sadly it was not to be.
I continued listening to my healing messages. They gave me life. I literally played them hours on end. Two days later, on Saturday the 16th of August, the WHO doctors came with some papers. I was informed that the result of my blood test was negative for the Ebola virus. If I could somersault, I would have, but my joints were still slightly painful. I was free to go home after being in isolation for exactly 14 days. I was so full of thanks and praise to God. I called my mother to get fresh clothes and slippers and come pick me up. My husband couldn't stop shouting when I called him. He was completely overwhelmed with joy.
I was told however that I could not leave the ward with anything I came in with. I glanced one last time at my CD player, my valuable messages, my research assistant, a.k.a my iPad, my phones and other items. I remember saying to myself, "I have life; I can always replace these items."
I went for a chlorine bath, which was necessary to disinfect my skin from my head to my toes. It felt like I was being baptized into a new life as Dr. Carolina, a WHO doctor from Argentina poured the bucket of chlorinated water all over me. I wore a new set of clothes, following the strict instructions that no part of the clothes must touch the floor and the walls. Dr. Carolina looked on, making sure I did as instructed.
I was led out of the bathroom and straight to the lawn to be united with my family, but first I had to cut the red ribbon that served as a barrier. It was a symbolic expression of my freedom. Everyone cheered and clapped. It was a little but very important ceremony for me. I was free from Ebola! I hugged my family as one who had been liberated after many years of incarceration. I was like someone who had fought death face to face and come back to the land of the living.
We had to pass through several stations of disinfection before we reached the car. Bleach and chlorinated water were sprayed on everyone's legs at each station. As we made our way to the car, we walked past the old isolation building. I could hardly recognize it. I could not believe I slept in that building for 10 days. I was free! Free of Ebola. Free to live again. Free to interact with humanity again. Free from the sentence of death.
My parents and two brothers were under surveillance for 21 days and they completed the surveillance successfully. None of them came down with a fever. The house had been disinfected by Lagos State Ministry of Health soon after I was taken to the isolation centre. I thank God for shielding them from the plague.
My recovery after discharge has been gradual but progressive. I thank God for the support of family and friends. I remember my colleagues who we lost in this battle. Dr. Adadevoh my boss, Nurse Justina Ejelonu, and the ward maid, Mrs. Ukoh were heroines who lost their lives in the cause to protect Nigeria. They will never be forgotten.
I commend the dedication of the WHO doctors, Dr. David from Virginia, USA, who tried several times to convince me to specialize in infectious diseases, Dr. Carolina from Argentina who spoke so calmly and encouragingly, Mr. Mauricio from Italy who always offered me apples and gave us novels to read. I especially thank the volunteer Nigerian doctors, matrons and cleaners who risked their lives to take care of us. I must also commend the Lagos State government, and the state and federal ministries of health for their swift efforts to contain the virus.

To all those who prayed for me, I cannot thank you enough. And to my First Consultants family, I say a heartfelt thank you for your dedication and for your support throughout this very difficult period.
I still believe in miracles. None of us in the isolation ward was given any experimental drugs or so-called immune boosters. I was full of faith, yet pragmatic enough to consume as much ORS as I could, even when I wanted to give up and throw the bottles away. I researched on the disease extensively and read accounts of the survivors. I believed that even if the mortality rate was 99 percent, I would be part of the 1 percent who would survive.
Early detection and reporting to hospital is key to patient survival. Please do not hide yourself if you have been in contact with an Ebola patient and have developed the symptoms. Regardless of any grim stories one may have heard about the treatment of patients in the isolation centre, it is still better to be in the isolation ward with specialist care, than at home where you and others will be at risk.
I read that Dr. Kent Brantly, the American doctor who contracted Ebola in Liberia and was flown out to the United States for treatment was being criticized for attributing his healing to God when he was given the experimental drug, Zmapp. I don't claim to have all the answers to the nagging questions of life. Why do some die and some survive? Why do bad things happen to good people? Where is God in the midst of pain and suffering? Where does science end and God begin? These are issues we may never fully comprehend on this side of eternity. All I know is that I walked through the valley of the shadow of death and came out unscathed.
Breaking a Fever
We can eradicate malaria—within a generation
New tools and a new strategy mean we can eradicate it in a generation.

I’m in New Orleans, where I just had the honor of speaking at the annual meeting of the American Society of Tropical Medicine and Hygiene (ASTMH). As you can imagine, given that this is a gathering of experts on infectious diseases in poor countries, Ebola is on everyone’s mind.
Even though I am confident that the U.S. and other countries with strong public health systems will contain the cases that are popping up within their borders, it’s devastating to see what this virus is doing to entire families in West Africa. At times like this, it’s easy for organizations like ASTMH to make the public case that global health matters to all of us in our increasingly interconnected world. I hope that will help strengthen the public will to do more to help poor countries lift the burden of disease—not just from emerging killers like Ebola but also from pathogens that have held back human potential for thousands of years.
That’s why, in my remarks at the conference, I addressed the Ebola crisis but devoted the bulk of my time to another killer disease: malaria. Based on the progress I’m seeing in the lab and on the ground, I believe we’re now in a position to eradicate malaria—that is, wipe it out completely in every country—within a generation. This is one of the greatest opportunities the global health world has ever had. Melinda and I are so optimistic about it that we recently decided to increase our foundation’s malaria budget by 30 percent.
Melinda and I first called for eradication back in 2007 along with Margaret Chan, who runs the World Health Organization. Melinda was eloquent and passionate in her call to action: “Any goal short of eradicating malaria is accepting malaria; it’s making peace with malaria; it’s rich countries saying: ‘We don’t need to eradicate malaria around the world as long as we’ve eliminated malaria in our own countries.’ That’s just unacceptable.”
Some people said then (and still say today) that we’re overly optimistic to be talking about eradication. After all, malaria is an enormously complex target and has defeated efforts to stamp it out in the past. They’re right that we shouldn’t promise the moon—you don’t get rid of a disease this complex overnight—but I am confident that the future will be different from the past.
Why? Because we’ve seen a huge scale-up in the resources and brainpower focused on this disease. Four countries have eliminated malaria since 2000, and two dozen more could do it in the next decade. Mortality rates worldwide have gone down by a remarkable 42 percent in that time—a good-news story that ought to make critics wary of trumpeting claims that foreign aid doesn’t work. More than 3.3 million people who would have died of malaria are alive today.
And we have tools today we’ve never had before—not everything we will need to achieve eradication, but more than we’ve ever had. Here are two of the recent innovations that fuel my optimism:
- Diagnostics: Malaria is not only treatable but also curable, thanks to a class of drugs derived from a flowering plant called Artemesia annua, or sweet wormwood. But until recently, there was no good way for most people who came down with a fever to find out whether they had malaria. In 2010, we got a great new tool, called the RDT (rapid diagnostic test). Armed with this 50-cent test, community health workers with little training can determine in minutes with 99 percent accuracy whether someone has malaria or not. Last year, we deployed 200 million of them in Africa alone.
- Modeling Systems: The digital revolution has produced fantastic new tools for tracking the disease. Public health experts are combining anonymous data from mobile phone records with data on malaria incidence to identify the key migration hotspots—allowing countries to target their resources in the most cost-effective and strategic ways. In Kenya, for example, these maps helped experts target large-scale tea plantations in the country’s Lake Zone. Comprehensive efforts at the plantations could make it possible to eliminate malaria from large swaths of the country’s highlands without even having to run elimination efforts there.
Just as important as any specific innovation, our team has converged on an eradication strategy that will make the whole greater than the sum of the parts. That strategy has three components: Complete Detection, Complete Cure, and Complete Prevention.
Complete Detection is a departure from current approaches, which focus on finding and treating only those people who have active malaria cases. To achieve eradication, health workers need to find all people who have the parasite in their blood, regardless of whether they’re showing symptoms. (I wrote about this work earlier this year, after Melinda and I saw it in action in Cambodia.) We’re supporting many efforts to develop and bring to market a new generation of diagnostic tools that are even more sensitive than the RDTs now in use and can identify the presence of malaria parasites in all infected individuals.
Complete Cure means using treatments that clear all malaria parasites from the body. Our best anti-malaria treatment today, known as ACT, generally cures the patient clinically but does not eliminate all forms of the parasites that are responsible for continued transmission. So we are trying to supercharge efforts to develop long-lasting, single-dose treatments for malaria that can completely clear malaria parasites from the body and provide a period of protection following the treatment. We believe that our largest partner in this effort, the Medicines for Malaria Venture, could bring these complete-cure drugs to market within five years.
Complete Prevention means reducing opportunities for mosquitoes to pass the parasite on to humans, and preventing the emergence of strains that resist drugs and insecticides. We’ll need next-generation vaccines that block transmission for six months to a year, so that once an area is cleared of the parasite, it stays clear. We’ll also need new insecticides to offset the widespread emergence of mosquito resistance to the chemical compounds we use most frequently today. We may even need cutting-edge approaches, like introducing special fungi into mosquito populations to kill them off or introducing modified genes that can stop mosquitoes from reproducing.
I believe it’s not only possible to eradicate malaria; I believe it’s necessary. Ultimately, the cost of controlling it endlessly is not sustainable. The only way to stop this disease is to end it forever.
If you want to join the fight, please consider donating to our partner Malaria No More.
Beyond the Plow
4 innovations for poor farmers
Four new tools that are helping poor farmers grow more food.

Whenever I visit small farmers in a poor country, I’m struck by how many are laboring with hoes, plows, and other implements that haven’t changed in generations. Yet farmers in wealthier countries have benefited from wave after wave of technological improvements. This gap is one big reason why some farmers produce much more food than others.
Thankfully, some of the brightest minds in Africa, India, and elsewhere are creating new tools to close the gap.
Here are four especially promising innovations…
For many years, so little agriculture research was being done in Africa that we knew less about the soil there than we did about the surface of Mars. Now that’s changing, thanks to an initiative to map the continent’s soil. The Africa Soil Information Service is creating digital maps that help farmers make informed decisions about which seeds to plant, which fertilizers to use, and how to raise their crop yields. They’re available free to anyone with a cell phone or Internet connection.
In Africa, half a billion people depend on cassava as a staple crop. But breeding more-nutritious, disease-resistant varieties of the root takes a long time—a decade or more. Now scientists with the Next Generation Cassava Breeding (NEXTGEN) project have cut that time in half, using computer modeling techniques and a treasure trove of new information on the plant’s genome. They have also improved the breeding cycle, so they can zero in on the most desirable traits earlier in the process.
How do you cheaply spread good information about farming? The Indian nonprofit Digital Green is having success with simple YouTube videos. They’ve shot thousands of videos featuring farmers sharing best practices. (See for yourself.) Farmers, they’ve found, are much more likely to listen to peers who look and sound like them. The idea isn’t limited to farming either: The UK’s development agency is now helping Digital Green use its platform to spread health messages.
Being a dairy farmer has risks. As I learned on a trip to Kenya, milk can spill or spoil on its way from the cow to the chilling station. So I asked the team at Global Good to study the problem. Working with Heifer International, they made a jug that’s easy to clean and won’t spill. Partners in Kenya and Ethiopia will make and sell them for about $5 each, versus up to $30 for other jugs. This modest step could help dairy farmers earn more money—and create new manufacturing and sales jobs too.
Cornell’s Corn
The love life of plants
Studying the love life of plants could help millions escape poverty.

Of all the things I did when I visited Cornell University recently, I probably had the most fun brushing up on how plants have sex.
Cornell is one of the world’s top universities for research on improving crops. Their work involves a lot of plant breeding. During one meeting, I got to try my hand at cross-pollinating wheat, which is a surprisingly delicate procedure. It gave me even more respect for the people who do it every day.
Cornell’s work on crop improvement also involves a lot of cutting-edge genetics. You might see the words “crop improvement” and “genetics” in the same sentence and think I’m talking about GMOs. Although Melinda and I do support research in that area—we don’t think poor farmers should be denied the choice to use any tools that might benefit them—the work I saw at Cornell is different. It’s focused on how the science of genetics can improve agriculture in other ways. And the advances are really exciting.
I got interested in crop breeding through my work with the Gates Foundation. Because most of the world’s poor people are farmers, helping farmers grow more food is one of the most powerful levers we have for fighting poverty. The faster we can improve crops—making them more nutritious or drought-tolerant, for instance—the faster we can help farmers become more productive.
My main guide was Dr. Ed Buckler, a scientist in his mid 40s who works at Cornell for the U.S. Department of Agriculture (USDA). Over the four hours we spent together I asked Ed dozens of questions (I’ve learned a lot about agriculture, but I’m still a city boy at heart), and he was always quick with an answer. Yet Ed and his colleagues aren’t just experts in their field—they’re also deeply passionate about their work. I can see why: The advances they’re working on will change people’s lives by dramatically accelerating a process that is now slow and laborious.
Here’s how it works today. Suppose you want a variety of corn with a natural resistance to a certain pest. You start by planting as much corn as you can. You wait 8 to 12 weeks for it to grow, and then you take pollen from some of the plants that aren’t infested and use it to pollinate others. If the offspring of those plants is pest-resistant, you’re in luck—your plant won the genetic lottery. If not, you have to start over. Because you’re limited by the growing season, the process can take seven to ten years.
Genetics research will cut that time in half.
Getting there takes three steps. One is to understand the crop’s genetic makeup. Ed took me on a short tour of a lab where machines called sequencers were analyzing DNA from thousands of plants. They were mapping the genes that give each plant its physical traits: its height, color, etc.
The second step is to go into the field and record those physical traits for each individual plant whose genes you’re studying. Cornell researchers are growing hundreds of acres of corn and other crops not far from campus, and they make regular treks out there to collect data. Unfortunately, I didn’t have time for a field trip on this visit.
Finally, you build a computer model that puts the two together—the genetic maps of individual plants, along with the data about their physical traits. Once you have that model, you no longer need to cross two plants and just hope for the best. You can ask the computer, “Out of all the plants I have in my field, which two should I breed in order to produce one that is pest-resistant?” Think of it as a highly sophisticated Match.com for plants.
Cornell and the USDA have already built such a model for some traits in corn; because people in rich countries eat corn, there’s a big market for better varieties. Meanwhile, crops that are eaten mostly by the poor have largely been ignored by scientists. But that’s starting to change.
With support from the British government, our foundation, and others, researchers at Cornell and the USDA are now working on a model for cassava, a root vegetable that’s a staple crop in many tropical regions. Partners in Uganda and Nigeria are growing lots of plants, recording their traits, and sending genetic samples to Cornell for sequencing. When the cassava model is finished, it will help breeders develop new varieties faster than ever. (Incidentally, I’m fascinated by cassava—and you may not know that it is responsible for the fun factor in bubble tea.)

During my visit, I learned about one trait that I had never thought about before: poundability. Over lunch with several graduate students, a Ugandan researcher named Paula Iragaba told me that women in her country do most of the work to turn cassava into flour, and they wish it were easier to process. “Women’s preferences have to be taken into account,” she said. I couldn’t agree more.
Keep in mind, none of the genetics research I saw changes the basics of plant sex. Breeders in the field still have to move pollen from one plant to another, as they have for ages. We’re just getting a lot smarter about helping them pick the best partners. And the result will be phenomenal—a much faster path to more-productive crops so that millions of people can eat better food, earn more money, and improve their lives.
My Favorite Root
The world’s most interesting vegetable
Here are a few facts about this intriguing root.

I’m kind of fascinated by cassava. You’ve probably eaten it, even if you didn’t know it. And it’s very important for feeding the world. Here are a few facts about this intriguing root.
1.
You Have Probably Eaten Cassava
If you’ve ever eaten tapioca pudding, you’ve had cassava. The starch takes its distinctive pearl shape when cooked slowly. It’s also responsible for the fun factor in bubble tea.
2.
Cassava Is the Stud of the Plant World
Cassava tolerates drought, resists most pests, grows well in poor soil, and unlike most crops, can be stored in the ground up to two years without rotting. This long harvest window means cassava can act as a kind of insurance against famine.
3.
Caution: May Contain Cyanide
Cassava’s natural pest resistance comes from naturally occurring traces of bitter cyanide in the vegetable. The poison is removed by cooking, soaking, and other methods.
4.
Breakfast, Lunch, and Dinner
In 2011, Melinda and I met Christina Daniel Mwinjipe (second from right), a farmer in Tanzania who grows at least four different varieties. She and her family eat the sweet ones for breakfast and boil the bitter ones into porridge for other meals. She also cooks the leaves, adding coconut for flavor.
5.
This Staple Crop Is At Risk
Cassava is tough, but it’s not invincible. Some of Christina’s plants were rotting (like the ones pictured here) because of a virus carried by flies. That meant she had to go to the market to buy extra just to feed her family.
6.
We Can Make It Better
Our foundation is working with researchers in Africa, the United States, and around the world to develop hardier varieties. We’re optimistic that one day all cassava farmers will be able to grow enough to feed their families and have some left over to sell for extra cash.
7.
Go Ahead, Ask Me About Cassava
Hopefully you can see why I think cassava is so interesting. In fact I have to remind myself not to talk too much about it at parties. Cassava is extremely important for feeding the world, and I’m quite hopeful about the opportunity to make real progress with it in the years ahead.
Short-Term Crisis, Long-Term Need
Ebola, beyond the headlines
What to do about the virus in the short term, and in the years to come.

I’ve spent the past week meeting with politicians, policymakers, and reporters in New York, Washington D.C., and Boston. One topic has pretty much dominated the conversation: Ebola virus.
It’s not surprising. Most of the headlines lately have focused on the undeniably awful news—the number of people who have died, the escalating rate of infection, the first case on U.S. soil. It is a tragedy for the families of those who have died. It is frightening for communities where people are sick. And it is yet another blow for countries that were already hit hard by poverty and other diseases.
Although you can never move too fast at a time like this, it’s easy to forget just how much has been done. Médecins Sans Frontières initiated a global call to action and has mobilized all its available resources to help combat the spread of the disease. Weeks ago, after the head of the Centers for Disease Control, Dr. Thomas Frieden, came back from Liberia with dire reports of the situation on the ground, President Obama sent the military to set up hospitals there. Congress agreed to pay for emergency supplies. The National Institutes of Health and other leading research institutions started working on drugs to treat the sick and vaccines to prevent the spread of the virus. France and the United Kingdom committed large sums of money and resources. Philanthropists, doctors, nurses, and other health workers from around the world have signed up to help the communities suffering the most. The global response has been remarkable.
Even as we do everything we can to stop this crisis, we should also be studying its long-term implications. It’s a reminder of the urgent need to strengthen health systems in the world’s poorest countries. (As former foundation’s CEO, Sue Desmond-Hellmann, wrote last week: “America has an incredibly responsive public health system that will ensure the virus is quickly contained, and that anyone suffering from it receives high-quality care in medical isolation.”) Health systems—which encompass everything from rural clinics to community health workers to hospitals—are the best protection against epidemics.
For example, as soon as the first case was identified in Nigeria, doctors and other people who were there to fight polio immediately helped set up a center to fight Ebola. This was critical in preventing the spread of the disease. Senegal, which has a more developed primary health care system than the most devastated countries, was also able to handle the first cases effectively and prevent a significant outbreak.
Improving health systems has other benefits beyond dealing with outbreaks. Providing basic health care raises the quality of life for everyone. It unlocks economic potential—healthy people are more productive. And countries with strong health systems can do a better job fighting both epidemics and ongoing diseases like malaria (which kills 600,000 people every year and leaves many more too sick to work for long periods).
What does this mean in practice? Liberia, Sierra Leone, and Guinea need support to strengthen their primary care systems now. Governments, donors, and other partners—from the private sector to NGOs and faith-based organizations—can join forces to build short-term capacity, while also building the foundation for health systems of the future. It will take an aggressive plan, with accountability measures in place, to start delivering core services such as routine immunization, maternal health, and family planning again.
So I hope we fight Ebola on two fronts: a short-term response to stop this crisis, and a long-term effort to build the health systems that will help prevent the next one.
Impressions of India
Meeting the new Prime Minister
India's Prime Minister has the country talking about toilets.

Narendra Modi has India talking about toilets.
As the New York Times put it before his visit to the United States recently, India’s Prime Minister has “pledged to cut through red tape, stamp out corruption, revive India’s economy and restore pride.” But he has also been quite outspoken on a subject you hear much less about: open defecation.
It may seem surprising when you think about all the innovation coming out of India, but 630 million people there defecate in the open because they don’t have access to a commode. Worldwide, the number is 2.5 billion people.
This is not the kind of issue that most politicians like to talk about. But I would guess that in the short time he has been in office, Prime Minister Modi has done more to raise the awareness of the need for toilets than any other leader since the country gained independence.
Creating good sanitation options for people—a safe place to poop—is a big focus of our foundation. So when Melinda and I met the Prime Minister in New Delhi last month, toilets were high on the agenda, along with vaccines, bank accounts, and health clinics. We came away impressed by his commitment to fighting poverty and improving health for India’s poorest people.
This was the third time Melinda and I had visited India together (we had each made several visits on our own too). It was an especially busy time there; President Xi of China was also visiting, and the government was responding to the deadly floods in Jammu and Kashmir. So we really appreciated all the ministers who made the time to see us. Prime Minister Modi was quite generous with his time: we ended up talking for more than an hour, twice as long as we had been scheduled for.

Judging from our time there, it sounds like he’s setting aggressive goals and pushing people to get them done quickly. He’s having a lot of intense meetings with various ministers, asking them, "What can you do in 100 days? Can you make your goals more concrete? More ambitious?”
We may have spent more time talking about sanitation than anything else. It was hardly the first time Melinda or I had discussed the topic in India, but usually we were the ones to bring it up. This time, the Prime Minister did. He made it clear that he is frustrated with the slow pace of improvement. He wants to end open defecation by 2019, and he walked us through a few of his ideas, including installing toilets in bus and rail stations in the country’s 500 biggest towns.
I talked about the opportunity to design 21st century toilets that don’t need big sewage systems and water treatment plants. Our foundation has co-hosted two Reinvent the Toilet fairs, including one in New Delhi, and I pointed out that two of the most advanced concepts are being tested in the Prime Minister’s home state of Gujarat. Some of the potential new designs take human waste and use it to create energy, fertilizer, or even drinkable water.
It wasn’t all toilets, all the time. We also discussed several other priorities of the Prime Minister’s, including extending banking services to every adult in the country. (Having a bank account is essential in building savings and escaping poverty—but today fewer than half of Indians have one.) We talked about India’s fantastic decision to provide its home-grown rotavirus vaccine to every child, as well as the Prime Minister’s efforts to fight malnutrition—which includes a particular focus on educating women and girls about good nutrition.
This is an exciting time, not just for India, but for everyone who cares about giving the poorest people a chance to lead healthy, productive lives. With all the attention and innovation going on in these areas—from health to financial services—we have a fantastic opportunity to make an impact. It’s inspiring to see India moving to the forefront of these efforts.
An Eye for Innovation
From idea to reality
A reminder from two young Aussies about what it takes to innovate.

There are two reasons I want to tell you about the pair of bright young people I met earlier this month. First, because they’re working on a project that could be a real life-saver in the developing world. And second, because the way they’re going about it is a great example for anyone who’s trying to turn an idea into reality.
Jarrel Seah and Jennifer Tang are medical students at Monash University in Australia who share a passion for technology. The 22-year-olds teamed up late last year to create an app called Eyenaemia, which lets people use their cell phone to screen for anemia. As the winners of this year’s Imagine Cup, a competition run by Microsoft, they visited the Seattle area and stopped by my office to talk about their work.
Anemia affects some 2 billion people around the world, and more than 290 million children. It’s an awful condition—you’re exhausted, your heart beats erratically, you get dizzy—and while it’s often caused by a lack of iron in your diet, it can also be a symptom of serious illnesses like malaria and bowel cancer. Jarrel told me, “In Australia’s aboriginal indigenous communities, over half of young children are anemic. And a large percentage of that is actually due to helminth infections—hookworms.”
Diagnosing anemia isn’t always easy. One method requires drawing blood and running lab tests, which simply isn’t possible in a lot of poor areas. And the cheapest test is very imprecise: A doctor pulls down your eyelid and checks the underside to see if it looks pale.
Eyenaemia is designed to take out both the expense and the guesswork. It lets you take a photo of the underside of your eyelid and then, judging by the color, tries to tell whether you’re anemic. “What's different about this is it’s noninvasive,” Jennifer said. “You don't need all that sterile equipment, and an untrained user can use it.” (Their idea is part of a promising trend: Researchers are studying whether cell phones can reduce the need for lab tests by detecting pneumonia, HIV, TB, and other conditions.)
It’s exciting to see bright young people like Jennifer and Jarrel applying their talents to problems that disproportionately affect the poor. As I told them, I could see a future version of Eyenaemia being used in developing countries, especially with pregnant women, since anemia contributes to nearly 20 percent of deaths during pregnancy.
So the tool has real promise. But Jennifer and Jarrel aren’t under any illusions. They know that having a great idea—“screen for anemia with a cell phone”—was only the beginning. In the early stages, they had a lot to learn: They went online to read up on design and cloud computing, which they didn’t know much about. Now the challenge is different. They have to keep improving their work.
We spent a lot of time talking about how they want to do that. For example, “We still have a high false positive rate,” Jarrel said. They’re looking at ways to bring it down by adding in factors like the patient’s age and gender, which they suspect affect the results by changing the color of the eyelid.
The idea that you have to keep refining your work might seem like old hat to a scientist who has spent decades perfecting a vaccine. Or to a software developer: When I was at Microsoft, we were maniacal about constantly learning from our customers and improving our products. But Jennifer and Jarrel’s efforts serve as a good reminder, especially for young people who are just getting started. Although innovation begins with a great idea, it certainly doesn’t end there.
John Green in Ethiopia
“It was invigorating and encouraging. And sad.”
The bestselling author reflects on our visit to Ethiopia.

I was playing bocce with a close friend recently when he told me, “I can’t bring myself to watch any of your videos about Ethiopia.”
Now, I don’t care if my friends watch my videos or read my books; I don’t know much about their jobs and don’t expect them to know much about mine. But the specificity of the comment surprised me, so I asked him why, and he said, “Well, it’s all just so SAD.”
I understand it: It’s difficult to look directly at suffering. And the challenges of our own lives can be so overwhelming that at times it feels like there’s no room left to consider the vast and tangled challenges of absolute poverty. We have to look away. “It’s too much,” my friend said.
But my visit to Ethiopia wasn’t sad—at least not merely so. It was invigorating and encouraging. And sad. And by being unable to look away—at least for a short time—I had the opportunity to listen to extraordinary people who’d brought tremendous positive change to Ethiopia.
The successes of the past twenty years are truly unprecedented in human history: Child mortality in Ethiopia has dropped by two thirds. Agricultural yields are improving. More kids are in school, and more of those kids go on to attend college.
Those are all very encouraging developments, but for narratively oriented people like me, it can be hard to internalize statistics until you see what this change looks like for individuals and families. At the rural health care outposts I visited, women told me about how radically the health care options for their children had improved. It was easier to get vaccines and antibiotics and rehydration solutions. Fewer of their kids were dying of malaria and pneumonia. Better family planning options allowed them to make choices about when to have kids. And while every mother I spoke to had been born at home, almost all of their kids had been born in a health care facility.
Maternal death is still far too common in Ethiopia, and infant mortality is still far too high. Ethiopia is a nation of 90 million people with just seven neonatologists. There are no CT scanners or MRI machines. Most of the people I met walked for miles twice a week to get water. And people die, every day, of easily preventable and treatable illnesses. But Ethiopia is also a nation with a growing middle class and an increasingly educated population (the University of Addis Ababa now has more than 40,000 students).
When we assume that stories about developing world countries will be merely sad, we do ourselves a great disservice, because the truth—as Oscar Wilde put it—is rarely pure and never simple. I emerged from my time in Ethiopia feeling not discouraged but energized. I was energized by people like Bill Gates and Sue Desmond-Hellmann, whose focus and commitment were inspiring. But mostly, I was energized by the parents and students and health workers I met in Ethiopia, who have helped bring radical improvement to their communities. There is, of course, so much still to do. But we shouldn’t look away or feel discouraged. We should get to work.
On the Subcontinent
Going—and listening—to India
What Melinda and I hope to discuss with the country’s leaders when we visit.

Melinda and I will visit India later this month. I’ve been there many times over the years, but I’m especially excited about this trip.
For one thing, India has reached some remarkable milestones in health. Earlier this year, the country was officially declared free of the polio virus for the first time ever, which is a huge accomplishment not only for India but for the global effort to eradicate the disease. Now India is starting to roll out its first home-grown vaccine, which protects children from rotavirus—a disease that each year kills more than 100,000 children in India and 400,000 worldwide. Overall, childhood deaths there have dropped by more than 50 percent since 1990.
All this adds up to a pivotal moment for India: If the country seizes the opportunity to improve health even more, especially for its poorest citizens, it can help hundreds of millions of people improve their lives and share in the country’s prosperity.
On our trip, Melinda and I will get to meet with several government leaders. We plan to do a lot of listening. Prime Minister Modi has made key commitments in some areas where our foundation works, like improving the health of women and girls, giving more people access to toilets, and expanding banking services to the poor. We hope to talk with India’s leaders about how we might help accomplish some of their goals.
Take India’s amazing efforts to fight child mortality. Along with the Health Minister, we will help launch a new plan for saving newborn lives by reaching every mother and baby with basic services. We’ll also see the leaders of Bihar and Uttar Pradesh, two of the poorest regions in India, for updates on efforts to strengthen the health systems there. We’re learning a lot through our partnerships there and hope they will ultimately serve as a model in other developing countries.
Sanitation is another priority. The Prime Minister has called for ending open defecation by 2019. Today some 630 million people in India—roughly half the country’s population—don’t have access to a toilet. That has terrible consequences: Poor sanitation will leave 62 million Indian children too sick to reach their physical and mental potential. It’s a tough challenge that requires building new infrastructure, developing new ways to handle waste, and persuading people to change longstanding hygiene habits. Among other things, our foundation co-hosted a Reinvent the Toilet Fair in India earlier this year, and it will be great to talk with the leaders there about how we can work together even more.
A third big goal of India’s is to extend banking services to every household in the country by next August. Giving poor families a safe place to save their money is one of the most effective ways to help them move out of poverty, but right now, fewer than half of Indian adults have access to a bank account. Our foundation’s work on reaching the unbanked puts a special focus on using digital technology, so we’ll be discussing that in detail.
No matter how many times I travel to India, I always come home impressed by the energy, intellect, and innovation I see there. I’m sure this time will be no different. I’ll post a few thoughts about the trip after we get home.
Africa’s Table
Why does hunger still exist in Africa?
Not starving, but still hungry in Africa.

When I first started traveling to Africa, I would often meet children in the villages I was visiting and try to guess their ages. I was shocked to find out how often I guessed wrong. Kids I thought were 7 or 8 years old based on how tall they were—would tell me that they were actually 12 or 13 years old.
What I was witnessing was the terrible impact of malnutrition in Africa. These children were suffering from a condition known as stunting. They were not starving, but they were not getting enough to eat, leaving them years behind in their development—and it was hard to see how they could ever catch up.
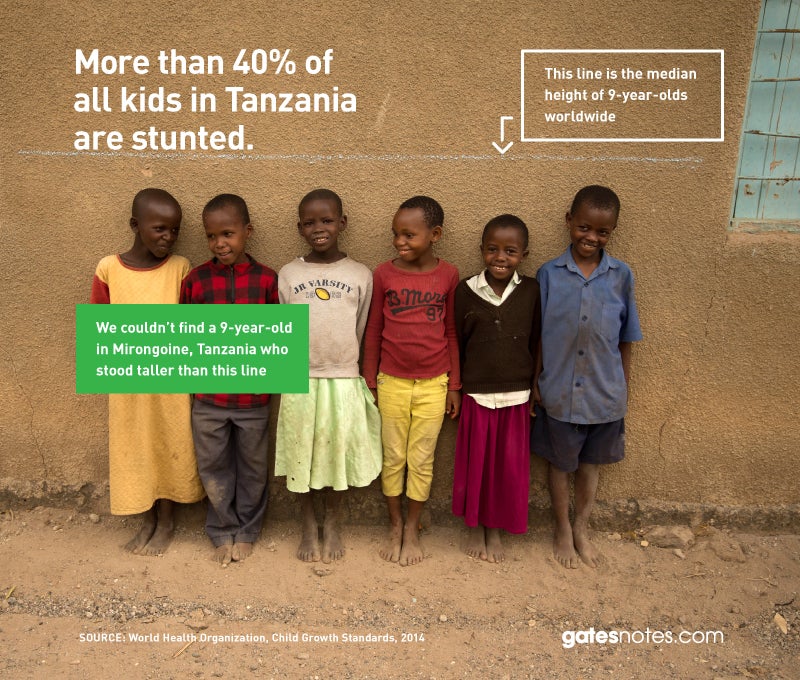
Stunting not only affects a child’s height. It also has an impact on brain development. Stunted children are more likely to fall behind at school, miss key milestones in reading and math, and go on to live in poverty. When stunted children don’t reach their potential, neither do their countries. Malnutrition saps a country’s strength, lowering productivity and keeping the entire nation trapped in poverty.
Worldwide, one in four children is stunted. Three-quarters of them live in South Asia and sub-Saharan Africa. However, while stunting has declined by more than a third in South Asia since 1990, in sub-Saharan Africa, the number of stunted children is still on the rise, up 12 million since 1990 to 56 million. Forty percent of all children in sub-Saharan Africa are stunted.
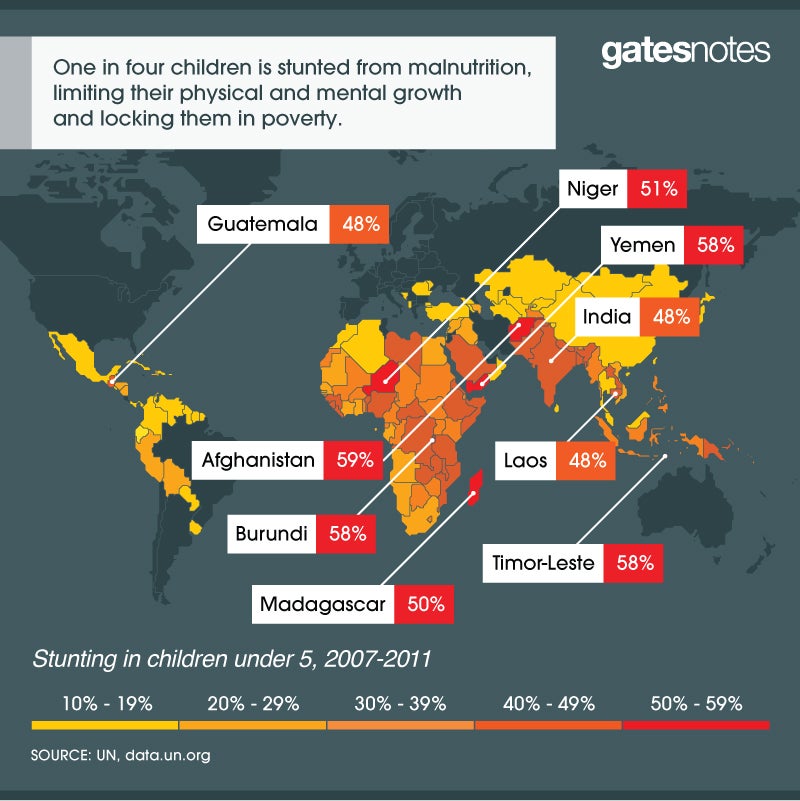
I run into a lot of people from rich countries who still think of Africa as a continent of starvation. The fact is, that’s an outdated picture (to the extent that it was ever accurate at all). Thanks to economic growth and smart policies, the extreme hunger and starvation that once defined the continent are now rare. As I saw when I was back in Africa last month with best-selling author John Green, today the issue isn’t quantity of food as much as it is quality—whether kids are getting enough protein and other nutrients to fully develop.
As Melinda and I have grown aware of the scale of this challenge, we’ve made improving nutrition a bigger priority for our foundation. One thing we’ve quickly come to appreciate is the problem’s complexity. There’s no vaccine to prevent stunting. Proper nutrition involves eating enough food, and the right kinds, every day of your life. While the global health community is still working to understand all of the causes and solutions to malnutrition, we do know a lot about how to ensure children get the nutrition they need for a healthy start to life.
We know that getting children the right nutrition in the first 1000 days—from the start of a woman’s pregnancy until her child’s 2nd birthday – is the best down payment on their future, giving them the opportunity to grow and develop physically and mentally. We also know that exclusive breastfeeding in the first six months of a child’s life is the single most effective intervention to help the brain develop and protect against life-threatening diseases. That’s why we continue to research the best ways to address cultural beliefs and other barriers that have kept almost half of all women from using optimal breastfeeding practices.
We know kids have a hard time getting the nutrients they need when fruits, meats, and vegetables are in short supply—so fortifying staple foods like cooking oil, flour, and salt with essential vitamins and minerals can fill the gap. We’re also beginning to develop new crops that are more-nutritious--including a sweet potato that’s enriched with vitamin A—and also produce a higher yield. Not only does this help smallholder farmers earn more income that can be used to diversify their family’s diet, it also puts more nutritious food directly on their table.
Providing better health care can make a difference too. Children who receive the rotavirus vaccine, for example, have fewer bouts of diarrhea, which can drain kids of vital nutrients and make them more susceptible to infection. Likewise, clean water and sanitation play a role in improving nutrition by reducing illness and disease.
We have many great interventions on our side, but with so many factors at play it can be difficult to measure which interventions have the most impact on improving nutrition and why. If I could have one wish, I would want the world to have a better understanding of malnutrition and how to solve it.
We have much more research to do in this area and we will continue to make progress. But what’s not in doubt is the importance of giving all children the nutrition they need for a healthy start to life. Their future depends on it. So does Africa’s.
Africa’s Table
Fortifying Africa’s future
Fortifying staple foods helps African children thrive.

I bet most people in the U.S. wish they ate better. More fruits and vegetables. Fewer donuts, chocolates, and—my favorite—hamburgers. The problem isn’t that we’re not getting enough to eat or all the essential vitamins and minerals. It’s that we’re getting too much of the things we don’t really need.
If you’re poor in Africa, you have the opposite problem. Your diet choices are often so limited—both in quantity and diversity—that you can end up shortchanged not just on calories but also essential nutrients, putting you at risk for severe infections, chronic medical conditions, and developmental problems.
In Tanzania, where I just visited as part of my trip to Africa, a typical meal for a poor family is a bowl of cornmeal with boiled vegetables. Meat is a luxury for most families, too expensive to buy except for special occasions. While these poor families don’t starve, they’re not getting enough to eat or enough of the vitamins and minerals we take for granted in rich countries. That’s why 42 percent of the children under 5 in Tanzania are stunted and many children suffer from deficiencies of vitamin A, iodine, and other key nutrients.
The lack of Vitamin A, for example, is the leading cause of childhood blindness in developing countries like Tanzania. It also compromises a child’s immunity, leaving them unable to fight common childhood infections such as measles or diarrhea.
One of the most effective ways to get kids the nutrients they need is to fortify staple foods to make them more nutritious. Bread, cereals, salt, and dozens of other everyday food items can be packed with essential vitamins and minerals, ensuring children get the nutrition they need. In rich countries, food fortification has been around for decades and we’ve seen the health of our children improve.
Now, fortification efforts are catching on in poorer countries. In 2011, the government of Tanzania passed a new food fortification law, which requires the country’s wheat flour millers and cooking oil producers to fortify their products. Iron, folic acid, and zinc are now added to wheat flour and cooking oil is made more nutritious with vitamin A. Working through our partners, Helen Keller International and the Global Alliance for Improved Nutrition, our foundation helped cooking oil factories in Tanzania get equipped with new systems to begin fortifying their oil. Every day, millions of families across Tanzania are now using the fortified oil to prepare their meals.
What’s remarkable about the fortification effort is how cost effective it is. For just pennies a year, a child can get the vitamin A they need for their healthy growth and development.
That is one of the best and smartest investments we can make in a child’s future.
Africa’s Table
Increasing awesome in Africa with John Green
John Green quizzes me on philanthropy, Ethiopia, and helicopters in Africa.

I didn’t know much about YouTube star John Green until a few months ago when my kids told me about his best-selling novel The Fault in Our Stars. It’s a deeply moving and, at times, surprisingly funny story about two teenagers with cancer who fall in love.
Later, I watched some of John’s video blogs and Crash Courses and was really impressed. People my age may not be John’s target audience, but I could quickly understand why millions of teens flock to his books and videos. One night I sat down to look at one of his online courses and then suddenly realized more than an hour had gone by as I watched John tackle complex ideas in history, biology and other subjects.
What impresses me most about John is his courage to ask tough questions—about cancer, the conflict in the Central African Republic, even how giraffes have sex—and then answer them in a way that is entertaining while at the same time super informative.
I asked John to come on part of my recent trip to Africa and found he was a terrific traveling companion. In Ethiopia, we visited health posts helping to vaccinate kids living in remote areas of the country; discussed the challenges of agriculture in Africa with a group of small farmers; and had an amazing conversation about growing up in Ethiopia with students at Addis Ababa University.
We also helped John conquer his fear of flying in a helicopter (though I’m not sure telling him how much safer it is than riding a motorcycle really convinced him).
As you can see in these videos, John’s endless curiosity was one of the highlights of our travels together. At every stop, he asked thoughtful questions about tackling poverty, getting young people involved in philanthropy, and tapping the power of storytelling to change the world.
So John, thanks for the great conversations and the company. I never thought of fighting poverty and disease as decreasing world suck and increasing awesome, but you convinced me that it’s as good a description as any other.
Mosquito Week
Why I gave my blood to defeat dengue
How a common bacterium may turn the tide against a terrible disease.

Melinda and I devote a lot of money and time to finding new and innovative ways to combat deadly diseases. But during a recent visit to Indonesia, I was asked to give something more—my blood.
Given the cause, I happily complied.
I got the request during a stop at Gadjah Mada University in Yogyakarta to check in on an amazing project to control the spread of dengue. Watch this video about my visit:
A mosquito-borne virus that causes serious illness and sometimes death, especially among children, dengue has spread dramatically in recent decades because of population growth and rapid urbanization in tropical and subtropical countries. About half of the world is now at risk of the disease. Last year, dengue cases were even discovered in Florida.
Researchers at the university are part of a global effort exploring whether a bacterium called WolbachiaWolbachia can be used to control dengue. occurs naturally in 70 percent of all insects, and it is harmless to humans. But it can block the transmission of dengue by mosquitoes. Unfortunately, the type of mosquito that carries dengue, Aedes aegyptiWolbachiaWolbachia, doesn’t naturally get , but one group of scientists discovered a way to infect them with it. Now, in partnership with other researchers around the world, they’re raising a colony of mosquitoes to be released in hopes that they will breed with wild mosquitoes and curb the spread of dengue. (The work in Indonesia is being funded by the Tahija Foundation of Indonesia.)
Working with local communities, researchers first released Wolbachia Wolbachia mosquitoes in Australia in 2011. In January, with the support of the government and residents, the Indonesian team began releasing mosquitoes in neighborhoods around Yogyakarta. During my visit, I had a chance to release dozens of the Wolbachia mosquitoes into the wild.
I also had an opportunity to speak with members of one neighborhood where the mosquitoes are now breeding. Several people told me about family members who became severely ill from dengue in recent years. One man had lost two family members to the disease. Now, they are optimistic that these mosquitoes will bring relief to the dengue burden in their city.
Many more of these amazing mosquitoes will need to be released into the wild in the months ahead before we can assess the impact of this project. That means the university’s research team will be busy breeding and raising thousands of Wolbachia mosquitoes. I have a lot of admiration for the members of the research team. Every week they take turns having their arms feasted on by several hundred very hungry female mosquitoes who need human blood to develop their eggs. There’s no risk of getting dengue from these lab-reared mosquitoes, but the bites itch just the same.
I learned that first hand when I agreed to offer a cage of mosquitoes a taste of my own blood. Within just a few minutes my arm swelled up with dozen of bites. It was a small price to pay for an amazing project that has the potential to turn the tide against a terrible disease.
Mosquito Week
“Mosquitoes are smart. We have to be smarter.”
A Tanzanian scientist on the front lines of the malaria fight.

One of the things I love most about my work in global health is getting to meet with amazing scientists who are trying to save lives. For Mosquito Week I thought I would introduce you to one of them: Dr. Prosper Chaki, whom I met in Tanzania in 2011.
Dr. Chaki runs a project in Dar es Salaam designed to kill Anopheles mosquito larvae. He spends his days wading into ponds, puddles, and marshes, spreading a biological insecticide in the areas where mosquitoes breed. His project has helped dramatically reduce malaria cases in the city. “Mosquitoes are smart,” Dr. Chaki told me. “We have to be smarter.”
He is just one of thousands of innovative researchers around the globe designing new and better ways to fight malaria. Thanks to their efforts the world is making progress against the disease.
You can learn more about how we’re getting smarter in our fight against malaria by watching this video about Dr. Chaki’s work.
Mosquito Week
What It Takes to Wipe Out Malaria
My visit to Cambodia, which is trying to eliminate the disease for good.

Many tourists know Siem Reap, Cambodia, as the base for exploring the beautiful 12th-century ruins at Angkor Wat. But when Melinda and I stopped there last week, we weren’t thinking about visiting a historic site. In fact we may have been the first visitors who ever passed through Siem Reap and skipped the temples completely.
We were on our way to see another piece of history in the making—Cambodia’s effort to eliminate malaria from within its borders. What we saw may eventually point the way toward a goal that’s shared by many of us in the global health community: eradicating malaria.
Malaria is one of the biggest killers of children on the planet, and Cambodia has made phenomenal progress fighting it over the past decade or so. Deploying an army of more than 3,000 village malaria workers who administer tests, give out medicine, and distribute bednets, they have reduced malaria from about 130,000 cases in 2000 to about 2,000 in 2012. Now the goal is to build on this progress by wiping out malaria entirely within Cambodia.
From Siem Reap, Melinda and I traveled to the remote province of Pailin in western Cambodia, near the border with Thailand, where researchers are running a pilot project to explore the best way to eliminate malaria.
They face a number of obstacles in their work. One is a kind of arms race, as drug-resistant strains of the malaria parasite keep emerging. For reasons that are not entirely clear, some of the most effective drugs against malaria have been rendered useless in Cambodia. There’s the potential for a real nightmare scenario here. If a strain of malaria that’s resistant to artemisinin were to spread to Africa—where artemisinin is the most commonly used anti-malarial drug—it would be the worst disaster ever in malaria control. But if we can eliminate malaria in Cambodia, we can not only save the lives of Cambodians, we can also prevent any new drug-resistant strains from developing and spreading to other places.
Another obstacle to eliminating malaria is that people can be infected by the parasite without showing any symptoms. Because the parasite is in their blood, they can transmit it to other people via mosquitoes, and those people can get very sick or die. The parasite is sort of like a James Bond villain who finds a secret lair from which he can carry out his deadly plot, undetected. So we need to treat everyone who’s infected, even if they don’t look or feel sick.
The project in Pailin is designed to try to get over these obstacles. The idea is to test everyone in the community to see who’s carrying the parasite and how much of it they’re carrying. Anyone who tests positive is given free treatment with the latest drugs. Here’s a video where I explain how it works:
Of course, there are downsides to this approach. People who don’t feel sick can be reluctant to get tested or take medicine. It’s also hard to keep people participating in the project, because they have to give blood every three months. So it was great to hear that Pailin’s village malaria workers, who have spent years building up trust in the community, are helping the project get over these hurdles.
Melinda and I met one of them, a man named Long Vuthy. He has been a village malaria worker since 2003 and is also the village leader. He told us he decided to join the program after watching the disease devastate his community. He proudly showed us his malaria kit—a tackle box containing tests, medications, and a log book where he records each case he encounters.
After meeting Mr. Vuthy, we walked to a local school where the screening is taking place. That morning, about 120 people had come to get their blood drawn and tested for the malaria parasite. They also answered a few questions designed to find out whether they might have been exposed to the parasite (e.g., “Do you work in the forest?”). For their trouble, they were paid a day’s wages, the equivalent of about $2.50, and got a free lunch.
As you might imagine, a project this involved would be hard to scale up using the drugs and diagnostics we have today. For example, the blood samples have to be shipped 250 miles to a lab in Bangkok that can run more-sensitive tests; that’s one reason our foundation is investing in a highly sensitive test that could be used in the field. We’re also funding research on new drugs that would cure malaria with one dose instead of the several doses now required. The fewer the doses, the more likely it is that patients will take all of them, and the more likely that the parasite will be killed off completely, which prevents drug resistance.
A lot more work needs to be done in the years to come. But I left Cambodia thinking that if we can be successful there, it will be a giant step toward the long-term goal of wiping out malaria everywhere.
Mosquito Week
The deadliest animal in the world
Sharks are wimps, compared to this beast.

What would you say is the most dangerous animal on Earth? Sharks? Snakes? Humans?
Of course the answer depends on how you define dangerous. Personally I’ve had a thing about sharks since the first time I saw Jaws. But if you’re judging by how many people are killed by an animal every year, then the answer isn’t any of the above. It’s mosquitoes.
When it comes to killing humans, no other animal even comes close. Take a look:
What makes mosquitoes so dangerous? Despite their innocuous-sounding name—Spanish for “little fly”—they carry devastating diseases. The worst is malaria, which kills more than 600,000 people every year; another 200 million cases incapacitate people for days at a time. It threatens half of the world’s population and causes billions of dollars in lost productivity annually. Other mosquito-borne diseases include dengue fever, yellow fever, and encephalitis.
There are more than 2,500 species of mosquito, and mosquitoes are found in every region of the world except Antarctica. During the peak breeding seasons, they outnumber every other animal on Earth, except termites and ants. They were responsible for tens of thousands of deaths during the construction of the Panama Canal. And they affect population patterns on a grand scale: In many malarial zones, the disease drives people inland and away from the coast, where the climate is more welcoming to mosquitoes.
Considering their impact, you might expect mosquitoes to get more attention than they do. Sharks kill fewer than a dozen people every year and in the U.S. they get a week dedicated to them on TV every year. Mosquitoes kill 50,000 times as many people, but if there’s a TV channel that features Mosquito Week, I haven’t heard about it.
That’s why we’re having Mosquito Week on the Gates Notes.
Everything I’m posting this week is dedicated to this deadly creature. You can learn about my recent trip to Indonesia to see an ingenious way to combat dengue fever by inoculating not people, but mosquitoes. (Somehow this story involved me offering up my bare arm to a cage full of hungry mosquitoes so they could feed on my blood.) You can read a harrowing account of what it’s like to have malaria and hear from an inspiring Tanzanian scientist who’s fighting it. And I’ve shared a few thoughts from Melinda’s and my recent trip to Cambodia, where I saw some fascinating work that could point the way to eradicating malaria, which would be one of the greatest accomplishments in health ever.
I hope you’ll have a look around. I can’t promise that Anopheles gambiae will be quite as exciting as hammerheads and Great Whites. But maybe you’ll come away with a new appreciation for these flying masters of mayhem.
Mosquito Week
What It Feels Like to Have Malaria
How the disease saps human potential.

Search the Web for “what it feels like to have malaria” and you will find a lot of harrowing descriptions.
Here’s an especially gripping one:
I awoke to what felt like lightning going through my legs, and then spreading through my body and in my head. Probably the worst headache, body aches, and chills you could possibly imagine. It felt like I was being stung repeatedly by an electric shock gun and could barely control my movements. The pain was so intense; I actually believed I was dying, literally crying out in pain so bad that I was taken to a 24 hour clinic that night at 3am.
Imagine feeling like that and trying to go to school, work, or take care of your family. It would be impossible.
It’s no surprise that economic growth in countries with severe malaria is significantly lower than in countries without it, even after accounting for other factors. As the economists Jeffrey Sachs and John Luke Gallup have written, “The only parts of Africa free of malaria are the northern and southern extremes, which have the richest countries on the continent.” Malaria is far from the only cause of poverty—but it is a significant one.
Whenever someone asks me why we should fight malaria, I have a simple answer: Because it kills so many people (more than 600,000 every year), and it leaves so many more people too sick to function, which holds back the world’s poorest from making the most of their lives. Malaria is gone from the United States and Europe. But where it is still a problem, few diseases do more to limit human potential.
This may all sound hopeless, but I’m actually optimistic that we can eventually eradicate malaria. I wrote about why here. I hope you’ll take a look.
Tax-Day Blues?
A reason to smile on April 15
A reason to smile on April 15.

There can’t be many days that are less popular than April 15. But I want to remind you of a fact that might ease the pain: The income taxes you’re paying will save lives in poor countries.
If your family makes the U.S. median household income of roughly $51,000, together you will buy someone in a poor country about seven months’ worth of HIV treatment. Or provide a lifesaving vaccine for 48 children. Or buy eight bednets that will protect people from mosquitoes that cause malaria.
These numbers might make you wonder if a large portion of your income taxes goes to foreign aid. After all, seven months of AIDS treatment can’t be cheap. You wouldn’t be alone in wondering this: Polls show that Americans tend to think nearly a quarter of the budget goes to aid.
It turns out that foreign aid is just 1 percent of the federal budget, or about $30 billion a year. Another way to think about it is that just 1 percent of your income taxes goes to foreign aid.
Compare that to other items in the budget. Defense for example is 17 percent, or more than $1,500 out of the median household’s income tax bill.
I believe that if more people knew what a small share of the budget goes to these programs, and how effective these programs are at saving lives, they’d want to do even more.
April 15 will never be anyone’s idea of a fun day, but I hope it helps to remember how much good American aid is doing around the world.
Maintaining Aid
Why I high-fived a colleague in Paris
Why I high-fived a colleague in Paris.

I don’t generally do a lot of high-fives. But as I climbed into the car after meeting with President Hollande in Paris this week, I held up my hand and slapped palms with one of my fellow passengers.
We were both celebrating and feeling relieved. Just a few hours before, it had seemed unlikely that the meeting would happen at all. The president had just announced a major reorganization of his Cabinet, and I didn’t think he would have time to talk with me about French foreign aid, the subject of our meeting. And even if he did have time, I thought the president might tell me that there was no way his government could maintain its aid commitments in the years ahead. Although France has an amazing track record in this area (it’s the second-largest contributor to the Global Fund, for example), the federal budget is under a lot of pressure. They are facing cuts on the order of 50 billion euros over the next three years.
So I definitely appreciated it when the president decided to keep our meeting even with everything else he had going on. And I was quite encouraged when he told me, without being asked, that he’s going to do his best to preserve France’s commitments. Of course, neither of us is under any illusion about how tough the budget situation is. But it was great to hear the president talk about the impact of France’s support and pledge to try to maintain it.
Paris was the second of three stops on this trip. I had been to Stockholm the day before and would be taking a quick trip to London the next day. In each place I wanted to encourage political leaders and voters to maintain their commitments to foreign aid, even in tough economic times. I wanted to remind people of all the lives they are saving.
This is an important year for Sweden, with elections for the national government and the European Parliament coming up later this year. I was pleased to hear from leaders in the major parties that they want the country to keep playing a leading role in global health and development, no matter how the election turns out. I had an especially productive meeting with Finance Minister Anders Borg, who oversees Sweden’s aid-related programs. He’s so interested in the work that he travels to Africa to learn and see the impact first-hand. We discussed some innovative ideas about how Sweden could take a leading role in funding infrastructure projects, like roads, in Africa. Improving its infrastructure is one of the keys to the continent’s growth in the coming decades, so I hope donors step up with creative funding ideas.
In Stockholm I also had a great time at an event hosted by one of my favorite global health experts, Hans Rosling, and three of his colleagues. Hans is unmatched in his ability to get you excited about the topic while also teaching you something. While I was there we shot a video about vaccination rates that involves me pouring orange juice out of a pitcher. (It will make sense when you see it, I promise.)
In London I got to visit Deputy Prime Minister Nick Clegg and thank him and Prime Minister David Cameron for committing to spend 0.7 percent of the country’s GDP on foreign aid. The U.K. reached that milestone last year, and they’ve said they want to maintain this level. The impact is phenomenal. For example the U.K. supports the GAVI Alliance, which provides vaccines that prevent millions of children’s deaths each year.
I also met with the CEOs of major pharmaceutical companies. We’ve gotten together every year for the past five to talk about the work they’re doing on diseases that affect the poor; I especially want to hear about the obstacles they’re running into and how we can work together to overcome them. This week we marked exciting progress on much faster tests and treatments for sleeping sickness (a.k.a. human African trypanosomiasis), which threatens millions of people in sub-Saharan Africa—during epidemics, it has been known to overtake HIV/AIDS as a leading cause of death in some communities. These advances make it possible for the first time to imagine eliminating this terrible disease. In fact I helped announce $240 million in new funding to treat neglected tropical diseases, including sleeping sickness.
I’ll close by sharing this selfie I took in Paris with a few Youth Ambassadors from the ONE Campaign. They’re part of a program that ONE started in Germany and is now taking to other countries to help keep foreign aid on the agenda. It’s always energizing to meet young people who are so enthusiastic about saving lives. Even on a trip where I heard a lot of a good news, they left me feeling especially optimistic.
Toilet Talk
The next great market opportunity: sanitation for India’s poor
To address a health crisis, India, hosted a Reinvent the Toilet fair.

If you’re inclined to take your toilet for granted, consider this. Half of all patients in hospitals in developing countries are there because of problems with water and sanitation. It’s a staggering health crisis that demands new ideas and new approaches. Last week we saw an encouraging sign that the sanitation issue is starting to get the traction it deserves: Delhi, India, hosted its first Reinvent the Toilet fair.
One problem is that flush toilets are impractical for billions of people. They require vast amounts of water and connections to expensive infrastructure, like sewer systems. Unfortunately, the current-day toilet works just well enough for rich people that no one seems to see the market for a new-and-improved toilet. That’s why we have been working with innovators from dozens of countries to reinvent the toilet so that it works for poor people.

The Next Great Market Opportunity: Sanitation for India's Poor
Last year, I went to New Delhi to talk to government leaders about this toilet initiative. They were very interested. More Indians have access to cell phones than to toilets that are clean and private. One consequence is a terrible diarrhea epidemic, which contributes to India’s huge burden of malnutrition and 200,000 deaths every year.
The Department of Biotechnology and other government agencies worked with us to put on the fair and showcase next-generation sanitation solutions. Solutions like toilets that need no water and convert fecal waste into electricity—or waste processing plants not much bigger than a shipping container that can turn thousands of gallons of fecal sludge into fertilizer.
It’s great to see India at the cutting edge on sanitation. When I joined Prannoy Roy last year for a taping of his TV show, he said people laughed at him 20 years ago for saying that one of the most important things India could do to be a better country is provide better toilets for women. Nobody’s laughing anymore. According to a recent World Bank report, inadequate sanitation costs India nearly $54 billion a year – equivalent to 6.4% of India’s GDP. Some smart people are starting to realize that on the flip side of this economic penalty is a big economic opportunity. As the World Bank report notes, improving India’s sanitation infrastructure could be a $152 billion market.
Just like any other sector, there is a value chain in sanitation. And all across this value chain—from the design of next-generation toilets that don’t require a sewer connection to the development of new markets for the collection and treatment of waste—there is amazing business potential.
India is especially well-positioned to lead in sanitation innovation. It is a proven leader in addressing difficult health problems, like eliminating polio. The country has a well-educated workforce and a demonstrated capacity for technological innovation. And it has a ready market of 630 million people looking for affordable sanitation solutions.
At the Gates Foundation, we see a lot of market failures—situations where poor people’s needs are ignored because it’s impossible to make a profit meeting them. India’s sanitation crisis is different. There is a desperate need. There are also billions of dollars to be earned. The toilet fair demonstrated that there is finally a wealth of innovative thinking about solutions. It will be fascinating to watch this market develop in the next decade.
Global Health Hero
A visit to Haiti, and the biggest hellraiser I know
Last month we caught up with Paul Farmer, a hero of global health.

Last month, Melinda and I took the kids on a vacation during their mid-winter break—and managed to get in a quick visit to Haiti, where we caught up with one of the heroes of global health, Paul Farmer.
If I had to list ten amazing people I’ve had the honor of meeting, there’s no question Paul would be right up there (Nelson Mandela would be at the top). I don’t have enough space in this post to do justice to what a special person he is, so if you want the full story, I’d suggest the book Mountains Beyond Mountains, by Tracy Kidder, which tells the whole story. Paul co-founded Partners in Health (PIH), which helps run medical clinics at 12 sites in Haiti, providing phenomenal levels of care—dealing with everything from ophthalmology to women’s health to HIV and TB. They reach more than a million people and employ thousands of Haitians. PIH also runs clinics and hospitals in several other countries, including Rwanda and Russia.
I don’t know anyone who does a better job than Paul of calling attention to the cause of global health. He’s not a scold—he really draws people in and gets them excited about the work. He chose to work not only in Haiti, but in some of most remote regions within Haiti. The poorest places in one of the poorest countries anywhere. He’s driven by a strong sense of justice. As he says, “The idea that some lives matter less is the root of all that's wrong with the world.” Short of meeting Paul in person, you can get a good sense of his passion from his book To Repair the World, a collection of speeches where his moral vision really shines through. If you really want to dig in to the details, Reimagining Global Health: An Introduction is a good place to start—it’s based on a course he co-taught at Harvard.
Melinda and I have met Paul in various places, but we hadn’t visited him in Haiti for nine years. I had read a lot about the earthquake that devastated the country in 2010 and was eager to see how things had progressed. Plus, just being around Paul is an inspiration in itself.
We started our day in Cange, a town in the Central Plateau of Haiti where PIH has a clinic. When we arrived, a small student orchestra was performing a song that I later learned was from Pirates of the Caribbean. At least judging from what we saw, life in Cange has improved since the last time Melinda and I were there. The health clinic has a lot more space now, and the local school has expanded too. While it used to take four hours over bumpy roads to get there from Port-Au-Prince, you can now make the trip in less than 90 minutes, thanks to a road that the European Union helped pay for.
I’ve met a lot of doctors working in poor communities. Sometimes they’re reluctant to get too attached to their patients, because the emotional toll would be so high. But not Paul. As we made our way through the clinic, he seemed to draw more energy from everyone he met—stopping to offer clinical advice to a nurse or a word of encouragement to a patient. I got the feeling he would have been happy to spend the day just roaming the halls and caring for people.
After Cange, we drove about 15 minutes to see a factory that makes a kind of fortified peanut butter for undernourished children. Abbott Laboratories helped fund the factory, and it is quite fancy. They have huge propane tanks to run heaters and big generators to power the machines inside. The peanuts are grown by 200 local farmers who trained at the facility. We watched as the nuts were roasted, shelled, and ground, and then mixed up with other ingredients to make the paste. A machine pours it into big 1 kg jars that will be distributed to families. There’s even a lab with technicians who test the paste for contaminants.
Next we drove into the city of Mirebalais to see the new hospital run by PIH and the Haitian government. I was blown away. The hospital opened last summer and was built using money donated after the 2010 earthquake (people who were injured in the quake still need ongoing treatment). As you can see from the video here, they spared no expense to make it a first-class facility. There’s a machine for performing CAT scans. There’s a sophisticated system for keeping medical records. The staff can send digital images to Harvard and get input from specialists there. They have modern incubators for premature infants. The hospital gets electricity from an enormous solar array (plus a diesel generator at night).
As we pulled up to the hospital, I noticed a bunch of kiosks set up out front. They weren’t part of the hospital, but they were a natural outgrowth of it. Every day several hundred people come to the hospital for care, but the staff can’t deal with them all at once. Local entrepreneurs have created this impromptu market where they sell food and other items to the waiting patients.
Inside, we met some of the patients and staff. One of our daughters is thinking about becoming a doctor, so she peppered Paul with questions as we walked around. We all visited the ward for premature infants. Later, on the flight out of Haiti, the kids told me how moving it was. They had never seen anything like that before.
In another ward, Paul introduced me to one boy who had had cholera, and another whose appendix had burst. For a lot of Haitians, those conditions would almost certainly have killed them. But thanks to the great care they got here, both boys were well on their way to being cured.
Overall we had a great visit. I saw real evidence of progress. Of course, Haiti has a long way to go: It remains quite poor. And I worry about how the projects I saw will generate enough revenue and enough generosity from donors so they can maintain such great facilities. Operations and maintenance—whether for a CAT scanner or a peanut processor—takes funding and technical expertise. I left Haiti wanting to learn more about how countries at various levels of wealth are able to build strong health care systems, especially for primary care.
But even understanding all the challenges, I felt hopeful about the opportunity for more Haitians to improve their lives. You know you’ve had a good trip if you can visit a country as poor as Haiti and leave feeling optimistic about its future.
On the Right Track
What I Learned About Polio in Nigeria
In Nigeria I saw firsthand how work is progressing on polio eradication.

I had a great visit to Nigeria last month and was able to learn firsthand about how work is going on polio eradication and immunizing kids against preventable diseases. There’s a tremendous opportunity now for Nigeria to eradicate polio and it was exciting to meet with many of the government and traditional leaders who are making this progress possible. I was joined on the trip by Aliko Dangote, a Nigerian and one of Africa’s most successful business leaders and philanthropists. Having his point of view on Nigeria and our efforts was really helpful.
On my first day in Abuja, Aliko and I went to the Polio Emergency Operations Centre, where government and donors come together to analyze the latest polio data, and plan the polio vaccination campaigns that are at the heart of this effort. They reported the fewest number of polio cases in three years, down 56% from this time last year and restricted to only two areas of the country. It was great to see Nigerians and partners work together to grab this opportunity. The rest of Africa and the world are watching. It can be done. And I believe it must be done.
Later in the day, Aliko and I met with the Speaker of the National Assembly, Ministers for Finance and Agriculture, as well as a private meeting with Nigeria’s President Goodluck Jonathan. I’m excited about our broad range of investments in health, agriculture and digital money in Nigeria. By increasing agricultural productivity – in a sustainable way – and supporting widespread access to digital money services, we can reduce hunger and poverty, and help improve the health and prospects of millions of families. Science and technology offer amazing opportunities for innovative solutions to tackle tough challenges in Nigeria for those most in need.
We joined a meeting of the Presidential Task Force on Polio Eradication, and were happy to take part in a ceremony to recognize state Executive Governors who have improved vaccine coverage rates and reduced polio cases. We paid tribute to the all-important traditional leaders who are often at the front line of changing behavior and encouraging mothers to have their kids vaccinated. The spiritual head of Nigeria’s Muslims, His Eminence, the Sultan of Sokoto, gave me a traditional robe and hat.
At the same event, President Jonathan announced he was conferring on me the Commander of the Order of the Federal Republic. Both honors were very kind, and I appreciated both the tributes as well as the commitment of so many people in Nigeria who are working to improve public health and reduce poverty.
Aliko and I had private meetings with some of the Executive Governors on the front line in the fight against polio, and the huge push to get life-saving vaccines to more kids. I was really impressed by the courage and commitment of Governor Shettima of Borno. That state has more polio than anywhere else in the country and there are big security challenges to reach every child. We also met with Governor Kwankwaso and his team from Kano, which is the most populous state in the north and has the second highest number of polio cases. Both Governors are determined to improve the public health systems in their states.
Aliko and I joined the Minister of Health, the Sultan of Sokoto, and the House and Senate Chairmen on Health to launch Nigeria’s newest Routine Immunization Strategy. It includes plans for the introduction of new vaccines, sets out a multi-year budget and describes strategies for reaching all children. This is also the first time there has been a focused look at fixing accountability at every level of the program – from the release of funds at the Minister’s level, to the delivery of vaccines by health workers in the field. This is a tremendous milestone. I was encouraged by the increasing attention to measurement and using accurate data to diagnose problems and help health workers better manage their programs.
The next day Aliko and I were in Lagos to learn more about Nigeria’s efforts to improve its vaccine supply chain. We visited the Lagos State Cold Store where the staff showed us how they are now monitoring vaccine stocks at each district level to improve the availability of life saving supplies. We also learned more about their work to streamline vaccine distribution. Prior to the program, 43% of the facilities were running out of vaccines. Under the new delivery system, this has dropped to just one percent. Transforming health systems is not easy. But it’s exciting to see this kind of innovation taking root in Nigeria. It’s making a real difference.
Aliko and I got a lot accomplished in a short amount of time, and we met with some truly committed leaders and field workers. I left Lagos more convinced than ever that Nigeria is on the right track. Next, it was on to Berlin.
Unite Against AIDS
On World AIDS Day, a Call to Action
We can all take action against AIDS, by learning, acting, and giving.

The theme for World AIDS Day this year is "Working Together for an AIDS-Free Generation." This year is especially important because the world is making huge progress against HIV, but we still don’t have all the tools we need to end the epidemic. This is a time for everyone to learn the facts about AIDS and put knowledge into action.
When you look at the facts, you see there’s a very clear, cause-effect relationship between the world’s level of investment in HIV treatment and prevention and the number of lives saved. Providing women, men and children with access to low-cost treatment literally means the difference between life and death. Access to treatment is reviving entire communities by helping people live healthy and productive lives.
But we still have much more to do. The rate of new infections is going down, but the number of people who get infected every year is still double the number who gain access to treatment. We need to stay focused on developing new prevention methods, like long-lasting pills and injectables, that can provide people with sustained protection over time.
And we have to stay focused on finding an HIV vaccine. A lot of new discoveries have given us hope that we can produce a safe and effective vaccine to protect future generations.
The organization leading the international anti-AIDS effort is The Global Fund, which currently provides HIV treatment to nearly 4 million people in Africa and is also a key partner in efforts to end mother-to-child transmission of HIV. The Global Fund has a new executive director, Mark Dybul, the former U.S. global AIDS coordinator. And it recently adopted a new approach to funding grants by investing additional money in health programs that are poised to achieve the strongest impact.
I’m convinced that the right people and organizations are assembled to push toward beating this epidemic. What’s not yet in place are the necessary financial resources. The Global Fund relies on voluntary contributions. Many governments and private organizations, including our foundation, have invested significant amounts, but the donations received so far fall short of what is needed to expand affordable treatment to those who need it.
One of the best ways that people can support the fight against AIDS is to donate to the Global Fund. You can contribute through the UN Foundation or by buying great holiday gifts through Product Red.
Take a few minutes to learn more about World AIDS day from these sites: UNAIDS for global information and AIDS.gov for information about the state of HIV in the United States. Then consider helping with a contribution to the Global Fund.
A Very Good Year
Good news you might have missed in 2013
Looking back at 2013, I wanted to share a different kind of list.

You’re probably seeing a lot of people’s year-end lists right now, going through the best movies, books, YouTube clips, grumpy cat memes, etc.
I thought I would share a different kind of list: some of the good news you might have missed. I’ve limited my list to global health and development, where Melinda and I spend a lot of time, but even so, there’s a lot to report. If you measure progress by the number of children who die of preventable causes, or by the number of people who escape extreme poverty—as I do—then 2013 was definitely a good year.
For example:
We got smarter and faster at fighting polio. You may have heard about recent polio outbreaks in Syria, Kenya, and Somalia. What you may not know is just how rapid and effective the response has been. It looks like the outbreak in the Horn of Africa was controlled in 4 months, less than half the time it took to control an outbreak there in 2005. That speed is due in part to the work done at the Global Vaccine Summit held inAbu Dhabi this year. In the past, the world has had to make tough trade-offs between responding to outbreaks, improving routine immunization, and fighting the disease in the last three countries where polio is still circulating (Afghanistan, Pakistan, and Nigeria). There was no coordinated plan or long-term funding for doing all three at once. At the summit the world got both. We adopted a comprehensive plan for pursuing all three goals, including making the world polio-free by 2018. And more than 30 donors—including a number of very generous private individuals—backed the plan with a total of $4 billion in long-term funding. That means we won’t have to make those trade-offs anymore. It’s a huge step forward.
There’s also great news from India. In early 2014, India will have gone three years without a single polio case (assuming no new ones are reported between now and then). That’s a testament to the fantastic job they’ve done immunizing every child, even in the most remote parts of the country. Now they’re focused on keeping the disease from coming back.
Next door, in Pakistan, the political leaders are clearly resolved to get polio out of the country once and for all. When I met Prime Minister Nawaz Sharif this fall, he made it clear that he sees vaccinating children as a matter of justice. Despite the ongoing violence there and in Afghanistan—including horrifying reprisals against vaccine workers—the next couple of years are a good opportunity for us to make progress on this goal.
Child mortality went down—again. One of the yearly reports I keep an eye out for is “Levels and Trends in Child Mortality.” The title doesn’t sound especially uplifting, but the 2013 report shows amazing progress—for example, half as many children died in 2012 as in 1990. That’s the biggest decline ever recorded. And hardly anyone knows about it! If you want to learn more—and I’d urge you to—the report has a good at-a-glance summary on page 3.
The poverty rate went down—again. If you want to read just one article that explains the state of the world’s poor and the future of the fight against poverty, check out “Not Always With Us,” which the EconomistEconomist ran in June. It gives a short but thorough overview of the progress so far—the poverty rate has dropped by half since 1990—and the prospects for keeping it going. As the article says, the biggest factor in reducing poverty over the past few decades has been economic growth—growth that touches not just those who are already rich, but a broad range of people. We’ll need to maintain this growth in the coming decades to keep the poverty numbers coming down. That’s one reason I argue for stepping up our investments on health: Health may not cause growth directly, but it does help lay the foundation for it. I never miss an issue of the , and this might be the best piece they ran this year.
Rich countries re-committed to saving lives. Just this month, donors met in Washington, D.C., to renew their funding commitments to the Global Fund to Fight AIDS, TB, and Malaria. I was there and I got to meet Connie Mudenda, a Zambian woman living with HIV who started getting treatment in 2004 thanks to the Global Fund. The medicine she takes costs just 40 cents a day, and it helped her get healthy, go back to work, and support her family. Connie says that a decade ago, she’d often see people who were so sick with AIDS that they couldn’t even walk. A family member would push them down the street in a wheelbarrow. Today, though, 80 percent of Zambians with HIV have access to treatment, the country’s economy is growing, and Connie says the wheelbarrows have vanished.
There’s a terrible Catch-22 in global health: You need new tools to fight diseases, but if you can’t pay to deliver them, they don’t get made; and if they don’t get made, then no one gives money to deliver them. So it’s fantastic that donors are stepping up to avoid this problem by making big commitments to the Global Fund.
A fantastic Web site got launched. If you love data, and if you’re curious about what causes the most suffering around the world, you should check out the Global Burden of Disease Web site, which was launched early this year. (The foundation helped pay for it.) Personally I am a yes on both categories, which is why I have spent a lot of time on there. It lets you make beautiful charts that help you understand the impact of disease in different countries and even see how things change over time.
On a personal note, I should say how grateful I am to everyone who made time to meet with me, from world leaders to health workers in India, Nigeria, Pakistan, and around the globe. Some of these workers take great risks to help people, facing attacks from extremists in order to vaccinate children. They are true global-health heroes.
What’s Ahead in 2014
Next year I’m excited about the continued rollout of a vaccine called pentavalent (because it prevents five diseases). Next year it will be available in South Sudan, the last of the 73 poorest countries to introduce it. India just announced that they’ll start giving it to every child in the nation in 2014. If other countries follow India’s example, pentavalent could prevent 7 million deaths by 2020. Next up are new vaccines to prevent pneumonia and rotavirus (which causes diarrhea). And we’re seeing more middle-income countries like China and India develop the ability to manufacture vaccines, which drives the cost down.
Crucial to delivering all these vaccines is GAVI, an alliance that has helped 440 million children get immunized since 2000. (Go back and read that again: 440 million.) Next year GAVI will be asking donors to renew their commitments, just as the Global Fund did this year. It will be a challenge to raise more money, but I know from experience that people want to help kids get vaccinated when they see what a phenomenal impact it has. It’s hard to resist the thrill of helping to save the life of a single child, let alone millions.
One last note about 2014: I’ll be publishing my sixth annual letter in January. This time I’m planning to take a slightly different tack from years past—Melinda and I will be tackling some of the biggest myths we encounter in our work on health and poverty. It should be a fun one to write. If you’d like to get an e-mail notice when the letter is out, you can sign up here.
MDG
Dream with a deadline: The Millennium Development Goals
In 2000, the U.N. set eight goals that changed the world. What's next?

Although it was several years ago, I still remember how Melinda and I felt when we learned about the Millennium Development Goals. We were hopeful, but we had reservations.
We were hopeful because the goals—eight specific targets for improvements in health, education, and other areas—shone a light on issues we were passionate about. We had been learning a lot about poverty, and about diseases that disproportionately affect the poor. We learned that millions of children die of preventable causes every year, and yet much of the world didn’t seem to be paying attention. So we were glad to see that three of the MDGs were specifically about global health, including reducing childhood deaths.
But as I said, we also had reservations. The MDGs were hardly the first time someone had declared that children shouldn’t die. And the U.N. had passed many resolutions calling for things that never came to pass. Why would this time be different?
Charles Kenny. Senior Fellow, Center for Global Development
Why I came to love the MDGs
It’s hard to pinpoint exactly when it happened, but over time Melinda and I moved from cautious optimists to full-throated fans. I think the MDGs are the best idea for focusing the world on fighting global poverty that I’ve ever seen. Next week in New York City, I will attend the U.N. General Assembly, where I’ll be meeting with a number of partners to talk about the progress of the MDGs and what comes next.
First, unlike so many vaguely worded international resolutions, the MDGs came with concrete numbers. You can use the goals to measure progress around the world and in specific countries. (This site lists all the targets and shows the progress toward them.) And the measures apply to things that everyone can rally around, like saving children’s lives and preventing maternal mortality. I’ve been writing about measurement a lot this year, because I’ve found that measuring progress is the only way to drive lasting success.
Second, the MDGs quickly got on the global agenda, even if they’re not that well-known here in the United States. I would visit a country like Ghana, and the leaders would be eager to discuss how they were doing on the MDGs. (Quite well, in Ghana’s case: They cut hunger by 75 percent between 1990 and 2004, for example.) I remember going to the World Economic Forum in Davos, Switzerland, and seeing for the first time a series of sessions on health and development. I doubt that would have happened without the MDGs. And Melinda and I never would have expected that in 2008, one of our daughters would come home from school with an assignment to learn about the Millennium Development Goals.
Third, the MDGs show how we can solve problems that might seem intractable. Sometimes people look at poverty or childhood deaths and say, “I feel bad about that, but there’s no way we can make progress on that in my lifetime. It’s just too depressing and complex.”
The MDGs cut through that complexity. The results prove that success is possible and real. Fewer children are dying and fewer people are living in poverty. The death rate from malaria has fallen by more than 25 percent since 2000. The proportion of people in extreme poverty has been cut by more than half, meeting MDG 1 five years early.
The River of Myths by Hans Rosling. Hans Rosling shows the amazing progress that poor countries have made in saving children’s lives and imagines what could come next
The success has been infectious. When donors see that their money is having an impact, they want to do more. Net foreign aid has gone up since 2000, and a large part of the increase has gone to global health.
How much credit do the MDGs get for this progress? There’s no way to put a precise number on it, but they probably had a bigger impact on health and education than on poverty. About three quarters of the drop in extreme poverty is due to China’s economic growth, which would have happened with or without the MDGs. But without the goals, it’s unlikely the world would have focused as much as it did on malaria, HIV/AIDS, maternal mortality, or childhood diseases.
A report card for the world
We have to acknowledge that we’re not going to meet all the goals.
Some people point to this fact and say, “Oh no, we’re failing.”
But I don’t look at it that way.
The MDGs aren’t a test that the world will either pass or fail. They’re more like a report card. Some country is getting an A in every subject. The ones that aren’t doing as well can go learn from the ones that are. Without the MDGs, we wouldn’t have any idea who was acing the test and who was struggling to get by.
In some cases, we’ll miss an MDG because the goals were unrealistically high to begin with. For example, MDG 4 is to reduce childhood deaths by two thirds. We won’t hit that number by 2015. But we have achieved the largest reduction in child deaths ever recorded. Millions of children’s lives have been saved. I dare anyone to call that a failure.
Time to double down
We can’t be satisfied with this progress. We have to double down on it. Various groups under the auspices of the U.N. are now talking about the new round of goals that will be adopted after the current ones expire in 2015. I don’t have a position on what the new goals should be, but I do think they should build on what made the current goals so successful—starting with the fact that there were only eight MDGs, which let the world zero in on the most important areas.
Next week in New York, I’ll be making the case for four other qualities that I hope the new MDGs will also reflect:
Focused on extreme poverty, including childhood deaths in the poorest countries. We can cut the number of childhood deaths by more than half—to well below 3 million—by 2030. In addition, the next round should focus on the poorest of the poor. Much of the progress in fighting poverty over the past 15 years has been among people who lived just below $1.25 a day. Those living on far less have largely been left behind. They are harder to reach, but just as deserving of the chance to make the most of their lives.
Measurable. The MDGs create a positive feedback loop by setting clear, specific targets and measuring the progress toward them. If the new goals are going to have lasting impact, they too need to have concrete targets that can be measured.
Actionable. The MDGs are focused on areas where we have the tools that will drive progress, like vaccines to stop childhood diseases and bednets to prevent malaria. The new goals should meet this same test. For example, improving governance is a worthy end, but do we have the tools to make it happen? It’s not clear.
Built on consensus. I hope people stay focused on goals that will get unanimous support. Otherwise, the U.N. could get bogged down in endless debate that could sap our momentum. No one can object to saving children and mothers.
Moving Ahead
Let’s remember what the MDGs have accomplished. They saved lives, and they helped rich and poor countries come together to make measurable progress on reducing inequity. That had never happened before. It is a wild success. It should inspire and guide our actions in the years ahead.
Tour of Progress
Video highlights of my India trip
India is making more-affordable vaccines and more-productive crops.

On my trip to India a few weeks ago, I got an update on the country’s progress with making more-affordable vaccines and more-productive varieties of crops. I also had a fun onstage Q&A with the very impressive Bollywood star Aamir Khan. Here’s a short video with a few highlights from my trip, including a look inside an agricultural research center that’s doing some exciting work on new crops.
(You can also read my blog posts about the trip here and here.)
Longer Lives, Smaller Families
Don’t Miss the Best News in Those New Population Numbers
These projections have two key points that are worth calling out.

The United Nations released some new population projections last week that are worth taking a closer look at.
The news coverage about the reports hit the high points: the UN projects that the world’s population will reach 9.6 billion by 2050, and India could overtake China as the most populous nation around 2028.
But a lot of the stories I’ve seen have missed two key points that are worth calling out.
First, life expectancy has been going up at an historic rate. You may know that the average life span went up in the 20th century—but did you know it increased faster in the past 100 years than at any other time in history? Life spans rose by nearly 50 percent, from 47 years in the 1950s to 69 years in 2010. And the U.N. projects that the average will keep going up for the rest of this century.
Of course, the average obscures a lot of variation among countries. In most rich countries today, the average life span is over 75 (in Japan it’s over 80), while in the poorest it is only 58. But even in those poor countries, the UN projects that life spans will reach 70 years by the middle of this century.
So if anyone tries to tell you how much better things were in the old days, you can ask them if they preferred it when 20 million kids a year died before age 5 (versus about 7 million today) and the average human being died before age 50.
That leads to the second point, and it’s a really important one:
As child mortality goes down, families get smaller. It’s counterintuitive, but it becomes crystal-clear when you look at the data: Just about all the countries where health is still bad also have high birth rates. And as more children in a country survive past age 5, the number of children born per woman goes down. It’s happened in China, India, Indonesia, Iran, Brazil, and South Africa, among other countries.
Why does this happen? Because when parents know their children will live long enough to support them in their old age, they decide to have fewer kids. The economist Jeff Sachs has written a lot about this point. The Swedish researcher Hans Rosling nailed it a few years ago in a brilliant and entertaining TED talk.
Of course, it’s one thing for people to want smaller families, and another for them to be able to act on this wish. That’s why it’s so important to make sure women have access to voluntary family planning, which our foundation does a lot of work on and is a big focus for Melinda.
These two facts—increasing life spans and the strong link between family size and child health—drive a lot of the work Melinda and I do. They tell us that the world is getting better; that the challenge is to make sure it gets better faster, and for everyone; and that one of the best ways to do that is by working to save children’s lives and supporting family planning. When health improves, life improves, by every measure.
Peas and Millet
Making a better pigeonpea
In Hyderabad, I saw how improvement in crop production helps poor farmers.


I have to admit: I’d never given much thought to pigeonpea and pearl millet before last week. But on my second day in India last week I got a fascinating lesson in how work with those crops is helping the livelihoods of some of the world’s poorest farmers.
After the meetings in New Delhi that I covered in my last post, we flew to Hyderabad to visit ICRISAT (short for International Crops Research Institute for the Semi-Arid Tropics), an agricultural research center supported by our foundation that focuses on crops grown in semi-arid climates, particularly certain cereals and legumes.
In the car from the airport, Sam Dryden, a senior fellow at our foundation, tutored me on legumes. They’re part of a family of plants that includes peanuts, soybeans, and peas. One defining characteristic of legumes is that their seeds, the peas and beans we eat, grow inside of pods. Beyond their importance as a high-protein food source, legumes are valued for their ability to enrich soil with nitrogen, which plants also use for food. That makes them a helpful neighbor to crops like maize and sorghum, and it means farmers can get two crops out of a field that might have typically grown just one.
The pigeonpea is a member of the legume family. Little known in the U.S., it’s an important crop in eastern and southern African, India, and other parts of Asia. The seed is used in a variety of foods such as dal, and its leaves and stems are an important feed for farm animals.
It’s also an example of what agricultural development people call an orphan crop, a crop that’s important to many of the world’s poorest people yet largely ignored by the big agriculture companies. Those companies focus on high-value crops like corn and soy that are building blocks of rich-world diets and industry. As a result, their research has boosted yields of those crops by making them more resistant to insects, disease, and drought. The orphans haven’t seen many, if any, of those kinds of improvements.
That’s where ICRISAT comes in. It focuses on coaxing higher productivity out of these neglected crops.
ICRISAT’s work with the pigeonpea is a great example. Traditionally, the varieties grown in Africa were low-yielding and susceptible to disease and pests. The plant’s small seeds also didn’t match the preferences of African farmers and consumers. The ICRISAT researchers described to me how they worked with other agriculture institutes and African government researchers to create a better pigeonpea. After decades of breeding, they developed the world’s first hybrid varieties – 23 so far -- with higher yields, faster cooking time, and a resistance to Fusarium wilt, a fungal disease.

The improvements mean that some African farmers have tripled their output to 1,200 kilograms per hectare since they started planting the improved seeds.
The results of that productivity are being felt in places like Ethiopia, Tanzania, Malawi, and Kenya. Of course, there’s a risk in raising yields: What if the increased supply drives down the price? Fortunately, farmers in those countries are now selling pigeonpea to India, which imports over 254,000 tons of the crop annually—a market so big that it can absorb the extra supply without affecting the price. Other changes—like connecting exporters directly to farmers—are also buoying prices. ICRISAT said that African farmers got about 80 cents per kilogram for the beans last year versus 20 cents per kilogram in 2005.
They also get insurance with the crop: Pigeonpea outlives maize in very dry conditions so when a drought strikes, farmers that plant both can rely on the hardier bean to survive.
The risk of drought drives a lot of research at ICRISAT since the dryland tropics it specializes in will absolutely see hotter, drier conditions in the coming decades. We owe it to the 2 billion people who live in those regions to develop drought-tolerant crops that can handle climate change. ICRISAT researchers are trying to meet that challenge through work on sorghum and pearl millet. We’ll tell that story later in a video from my visit.
GEMS
Some Exciting News About Saving Kids’ Lives
See the results of a study on the rates of child deaths from diarrhea.

A few days ago, I read some news that could help write a happy ending for a story that Melinda and I have been telling for years. The story is about a newspaper article that opened our eyes to diseases in poor countries. The article said 800,000 children died from diarrheal diseases every year. We were shocked. We thought, “That can’t be true. But if it is true, we should try to do something about it.”
Sadly, it was true. When we started our foundation in 2000, we made global health a priority.
As I learned more about the impact of diarrheal disease, I asked the foundation team that worked on them, “How many different pathogens cause diarrhea in kids? And which ones cause the most deaths?”
I was amazed by the answer. Diarrhea is caused by at least 40 different pathogens. Different ones have to be treated in different ways. But what really blew my mind was that it wasn’t at all clear which pathogens caused the most deaths.
The global-health community had never done a large-scale study on this question. The studies that had been done were limited, focusing on only very young children or looking at only a few causes of diarrhea. And that kept us from making as much progress as we wanted to. How could we know where to focus our efforts? Which pathogens should we go after first?
To answer that question, in 2007 the foundation supported a study that looked at 40 pathogens. It evaluated more than 20,000 children under the age of 5 in seven sites in sub-Saharan Africa and South Asia with high rates of deaths from diarrhea. The results just came out this month, and they’re very exciting.
The study, called GEMS (for Global Enterics Multi-center Study), found that most cases are caused by just four pathogens. Since we were dealing with 40 before, that means we’ve cut the number of potential targets by a factor of ten. And the global-health community already has, or is working on, vaccines for three of the four pathogens, including the most common one, rotavirus. That tells us we need to expand access to the current rotavirus vaccines and keep working on new ones that are effective in the developing world, which is a big focus for our foundation.
The study did contain one big surprise: At most of the sites, the second biggest cause was a pathogen called Cryptosporidium. Almost no one expected that. There’s very little research being done on treating or preventing it, so this is something the global-health community will need to explore.
There’s a lot of good news from this study. It confirms that we already have many of the tools we need to save a lot of lives, including vaccines and broader solutions like promoting access to clean water, exclusive breastfeeding, and other steps. And it points the way to new areas where we need to be working, like Cryptosporidium, to save even more children.
This study is another good example of why measurement is so important. (I’ve been writing about measurement a lot this year.) With this new data pointing the way, we can make sure every hour of effort and dollar of funding is targeted where it will do the most good.
The article about diarrheal diseases that Melinda and I read years ago inspired us to get involved in global health. It’s a sad story, but it doesn’t have to be. Progress like this makes me very optimistic that this story can have a happy ending. If you’re looking for reasons to be optimistic about saving lives, I can’t think of a better one than this.
Meeting Problems with Solutions
Getting better all the time
Halfway through the first day of my India trip, TV personality Prannoy Roy told a story I think really highlights the progress of India’s long journey to better health.

Halfway through the first day of my India trip, TV personality Prannoy Roy told a story I think really highlights the progress of India’s long journey to better health.
We were filming a question-and-answer segment in front of a studio audience for his show on New Delhi Television, one of India’s largest news networks.Prannoy was asking me and Bollywood star Aamir Khan about philanthropy, health, and India’s development when he recounted a discussion he had about 20 years ago. A former prime minister asked him and a group of other people what India could do to be a better country. Prannoy said his answer – provide better toilets for women – was met with nothing but laughter.
Things have really changed. Just before seeing Prannoy, I had spent several hours in meetings with Indian parliamentarians and ministers. Our wide-ranging conversations about health and vaccines almost always returned to how to stop the spread of diseases through better sanitation and, specifically, toilets.
I was glad: the toilet is one of my favorite topics. At each meeting I got to talk about how flush toilets (ones that use water to clear the waste away through plumbing) won’t make it anytime soon to much of the world, including rural India where infrastructure is poor and water is scarce. Instead, we need to invent a better toilet, one that doesn’t use water yet eliminates harmful microbes and gets rid of any smell. Last year our foundation sponsored a “re-invent the toilet” fair where 14 universities submitted innovative answers to that problem. None were perfect but they all were a step in the right direction.
After several meetings it was clear there was strong interest in holding a similar “re-inventing the toilet” event in India early next year. We set some follow-up meetings to start figuring out how to make it happen. We agreed that applying India’s many creative minds to the sanitation problem could speed the path to a breakthrough.
In my post, “Why I’m Going to India,” I wrote that the country is an ideal place for understanding both the problems and the solutions in areas that our foundation focuses on. In my meetings yesterday, the sanitation discussions were just one example of the great optimism I felt from government leaders and health experts for overcoming the problems. I also heard about several new solutions.
A group of polio experts updated me on how India’s focus on ridding itself of that disease is paying dividends to broader health efforts. After a lot of hard work, India has been polio free since January 2011. India will be certified polio-free if there isn’t another case by next January. I’m confident we can get there. Yesterday the experts walked me through how they are using satellite mapping to not only see where they need to provide the polio vaccine but also to expand the country’s system of routine vaccinations (the vaccines children get in their early years). With satellites and cellphones we are getting far more detailed health data on hard-to-reach places. I’m convinced those tools, pioneered with polio, will be a game changer for expanding routine vaccination.
I also sat down with some of India’s top scientists, public health experts and pediatricians. This group was celebrating amazing progress of the phase 3 trial of Rotavac, India’s first home-grown vaccine for rotavirus, the world’s main cause of diarrheal disease—which, after pneumonia, is the second leading killer of children under age five. I touched on rotavirus in yesterday’s post but it’s worth emphasizing again. The work the group did to create the vaccine, and run a very high quality trial is nothing short of phenomenal. Rotavac is a rare global collaboration among the Indian government, vaccine manufacturer Bharat Biotech, and others including PATH, the U.S. Centers for Disease Control and Prevention and the National Institutes of Health. Our foundation provided grants to support the work.The next milestone is to get the vaccine licensed by Indian authorities.
Dr. M.K. “Raj” Bhan, former secretary of India’s Department of Biotechnology and a pediatrician who shepherded the vaccine’s creation, told me that he expects the vaccine to clear India’s regulators by the end of the year, an estimate the country’s minister of health echoed later in the day. That means that India could start introducing the vaccine next year and start saving tens of thousands of kids’ lives a year.
In answering the prime minister two decades ago, Prannoy, our TV interviewer, pointed to a health problem that India still hasn’t fixed. Yet things are absolutely getting better. Since that time, India’s child mortality has dropped 45%, better than 35% for the world as a whole. With every visit to the country I see how India will drop that further as it gradually solves its health issues. An official I met at India’s Planning Commission yesterday described how India is “slow and deliberate” and ultimately successful in working through challenges. “That’s what this country is all about: finding a way,” she told me.
Today I’ll see another example of how India is finding a way when I visit a research center using old and new technologies to help boost agriculture productivity andfight malnutrition.
A Generous Turnout
Behind the scenes at the Vaccine Summit
We reached a critical milestone in the race to eradicate polio.

As I mentioned in an earlier post, last week I attended the first-ever Global Vaccine Summit in Abu Dhabi. In the months leading up to the conference, we weren’t at all sure how successful it would be. Budgets are tight. How much would governments and donors be willing to contribute?
In the video above, I talk about how things turned out.
I want to especially thank these seven private donors, who came together at the Summit to contribute $335 million to help eradicate polio.
- His Royal Highness Alwaleed Bin Talal (Alwaleed Foundation)
- Michael Bloomberg (Bloomberg Foundation)
- Ray Dalio (Dalio Family Foundation)
- Carl C. Icahn (Foundation for a Greater Opportunity)
- Carlos Slim (Fundación Carlos Slim Helú)
- Dato Tahir (Tahir Foundation)
- Albert L. Ueltschi Foundation
With these and other commitments, including $1.8 billion from the Gates Foundation, we raised $4 billion, which is enough to vaccinate more than 1 billion children against polio and other diseases over the next five years. That’s phenomenal—it’s more than 70 percent of the funding we’ll need for the plan we rolled out at the Summit to free the world of polio by 2018. Now we need to finish the job by raising that final 30 percent. When we eradicate polio—and I’m confident that we will—it will be a critical milestone in the Decade of Vaccines, a vision to reach all children with the vaccines they need by 2020.
Off to a Great Start
Global Vaccine Summit: We Changed History
The Summit was a big success.

I want to share with you my excitement over the outcomes of the Global Vaccine Summit in Abu Dhabi to celebrate the huge progress we’ve made toward ending polio and protecting all children with life-saving vaccines. The Summit was a big success.
World leaders including health and political ministers from Afghanistan, Nigeria and Pakistan, EU President Jose Manuel Barroso and former UNSG Kofi Annan appeared alongside polio survivors and vaccine heroes like Ade Adepitan, a British Paralympic medalist who contracted polio as a child in Nigeria, and Sikha Patra and Salim Shekh, two kids from India who organize polio immunizations for their community in Calcutta.
We had an amazing cross-section of participants, including community leaders like the Sultan of Sokoto from Nigeria and Rotarian Deepak Kapur from India, industry representatives, and leaders from our organizing partners UNICEF, GAVI, WHO and GPEI. Although he couldn’t attend, Archbishop Desmond Tutu, a polio survivor, also added his voice to the gathering.
We were also in Abu Dhabi to have some frank discussions on what still needs to be done to reach our ambitious goals.
And I’m proud to say that collectively, we changed history. The Global Polio Eradication Initiative rolled out a new strategy to achieve a polio-free world by 2018. Global leaders demonstrated their confidence in the six-year plan by pledging their financial and political commitments to help ensure its success.
In all, we raised a total of $4 billion dollars. That’s close to three-quarters of the plan’s projected $5.5 billion cost over six years, and enough to protect more than one billion children from polio forever.
Countries like Norway, Canada, Germany, Ireland, and the UK made generous pledges, as did His Royal Highness the Crown Prince of Abu Dhabi. The $4 billion also includes $335 million from private philanthropists such as Carlos Slim, His Royal Highness Alwaleed Bin Talal, and Mayor Michael Bloomberg. The foundation stepped in with $1.8 billion, a third of what’s needed for the polio campaign.
The Summit pledges are a huge step towards a fully funded plan, and I hope that financing won’t be the thing that stands in the way of achieving the miracle of polio eradication.
Collectively, we sent a powerful message that the world remains committed to fulfilling the vision of the Decade of Vaccines to end polio and reach all children, no matter where they live, with the vaccines they need.
Waste Management
Why we’re talking to scientists about toilets
Melinda and I encouraged scientists to innovate to help the poor.

Melinda and I spoke earlier today at the National Academy of Sciences, a non-profit group that has advised the nation on important scientific matters for 150 years. The NAS has roughly 2,200 members, all scientists at the top of their respective fields. About 200 of them have Nobel prizes.
Naturally, I took the opportunity to talk about toilets. Of course I also mentioned vaccines and other life-saving scientific advances. Melinda talked about the benefits of contraception and agriculture. But I put special emphasis on our Reinvent the Toilet Challenge, because it’s a great example of one of our biggest priorities: encouraging scientists to focus on the problems of the poor.
Scientific advances like the microprocessor and new medicines have been key in lifting millions of people around the world out of poverty. In my lifetime, extreme poverty has been cut in half. So have the number of people who don’t have safe drinking water, and the number of mothers who die during childbirth.
But we can do even better. There are many life-saving discoveries that don’t reach the developing world. Or they aren’t tailored to meet the needs of the poor to begin with. The toilet for example has been essentially the same technology for 200 years, and it requires infrastructure like sewage systems that are out of reach for much of the world. That leads to open defecation and other problems—and 1.5 million children who die each year from contaminated food and water. So Melinda and I made the case for finding more ways to make sure the poor are among the first, rather than the last, to benefit from scientific progress.
Why the National Academy of Sciences? Because it’s a group that represents one of the greatest resources we have in fighting poverty and disease: brainpower. Material scientists can make big advances on the next-generation toilet. Geneticists can develop new seeds that help farmers grow more nutritious food and raise their incomes. Energy researchers can create cheaper, cleaner forms of energy to meet the growing demand for it in the developing world.
Here are some specific ways we’re trying to use the power of science to benefit the poor:
Reinventing the Toilet
Many of us in the rich world take toilets for granted. But today 40 percent of the world’s population doesn’t have access to them. Instead they resort to open defecation, which contaminates water and food supplies, killing 1.5 million children a year. Unfortunately, today’s toilets require complex sewer infrastructure that won’t work in many of these settings. So we need to design affordable toilets that work in these communities.
Last year eight universities participated in a Reinvent the Toilet Challenge. We held a fair to celebrate the winner, and I got to award prizes to the top three winners. It probably says something about me that I really had fun handing out prizes for toilet designs.
SCUBA Rice
In her speech, Melinda talked about the importance of providing farmers with new seeds. One example of this is the effort to develop new varieties of rice that can thrive in areas of Asia and Africa, where rice yields are historically much lower than other parts of the world because of flooding, drought and poor soils. Partners from around the world are working to create rice that can “hold its breath” underwater.
Grand Challenges
In 1900, the German mathematician David Hilbert sparked a century of innovation in mathematics by identifying the 23 problems in that field that most needed solving. That’s the model for the Grand Challenges in Global Health. A panel of scientists has identified 16 challenges that, if solved, could lead to breakthrough advances for the developing world. They include everything from making vaccines that don’t have to be refrigerated to preventing mosquitos from transmitting malaria.
Midwife Calling
Ghana: Mobile technology for global health
Mobile phones keep midwives and patients connected.

In Ghana, the Grameen Foundation is using mobile applications to improve the quality of maternal health and childcare. With the MOTECH Mobile Midwife program, pregnant women can register and receive voice messages that provide reliable advice for a health pregnancy. Smartphones are also used to record health services delivered.
Texting Immunity
Mozambique: Mobile Technology for Global Health
Text messaging has increased immunization rates in Mozambique.

In Mozambique, Margarida Mathshinhe and VillageReach use text messaging to improve routine immunization. VillageReach deployed the Dedicated Logistics System (DLS) to increase the scale and efficiency of vaccine delivery to children living in rural areas.
First, Celebrate
Not Your Typical Vaccine Conference
This week I'm going to Abu Dhabi to attend the Global Vaccine Summit to celebrate the tremendous progress the world has made in ending polio and immunizing children.


This week I’m going to Abu Dhabi to attend the Global Vaccine Summit to celebrate the tremendous progress the world has made in ending polio and immunizing children.
This isn’t going to be typical conference. We aren’t going to have breakout sessions or canvas bags crammed with printed reports to take home. We’ll be there to do just two things: first, celebrate the progress we’ve made in the Decade of Vaccines to reach all kids, everywhere, with the vaccines they need; and second, to share best practices and have some frank discussions on what still needs to be done. As part of that, the Global Polio Eradication Initiative will roll out a new strategy to end polio once and for all. Global leaders will discuss their confidence in the plan and pledge political and financial commitments to help ensure its success.
Why Abu Dhabi? His Highness General Sheikh Mohamed bin Zayed bin Sultan Al Nahyan, Crown Prince of Abu Dhabi, is joining UN Secretary-General Ban Ki-moon and me to host the Summit, the first of its kind. The Crown Prince, an important partner of the foundation across several issues, represents to me the inspirational leadership we are seeing from the Middle Eastern and Islamic communities to improve child health worldwide.
In my talk, I’m going to share some of the numbers that impress me, such as the measurement systems that have allowed Ghana to build a strong immunization system. And I’ll share numbers that make me angry. For example, a child born in a low-income country is 18 times more likely to die before reaching the age of five compared to a child in a high-income country—largely due to preventable causes. That inequity is simply unacceptable and completely fixable.
I’m excited to meet some pretty amazing heroes while I’m there, too. World leaders like Jose Manuel Barroso and Kofi Annan will appear alongside Ade Adepitan, a British Paralympic medalist who contracted polio as a child in Nigeria, and Sikha Patra and Salim Shekh, two kids from India who organize polio immunizations for their community in Calcutta. I get to meet the two winners of my annual Gates Vaccine Innovation Award, too. Archie Panjabi will be our emcee. She appears on the American series The Good Wife and is using her celebrity to be a strong advocate for ending polio.
Thousands of people—scientists, investors, health experts, community leaders—share involved in the process of immunizing a child. We need to have the right vaccines, developed and manufactured at affordable prices, delivered to the hardest-to-reach children. It is crucial to build up strong routine immunization systems to protect our gains against polio and provide a platform for primary care. When the world comes together, we can set ambitious goals, we can measure our progress, and we can achieve even more. I’m counting on the Global Vaccine Summit to do just that.
No "One Size Fits All"
Putting HIV Patients at the Center
The lessons I drew from my visit to a clinic in South Africa.


Experts have long recognized that there is no “one-size-fits-all” approach to HIV services. The features of the global HIV epidemic vary by country, often by community and patient, and it’s important to understand these distinctions so that we can design programs to meet people’s needs and strengthen their access to treatment and prevention.
A few months ago, I had the opportunity to meet Craig Househam, who heads the Department of Health in the Western Cape, one of South Africa’s nine provinces. We talked about how his department is delivering health care to the thousands of people living with HIV in the townships and rural areas surrounding the city of Cape Town. I was really impressed with the approach that Professor Househam and his team have created in the Western Cape, and I want to share some of the lessons that I think can be drawn from it.
One thing that the system does well is to tailor the support provided to each HIV patient by offering different tiers of engagement with the health system.
In many countries, all HIV patients are expected to have the same level of engagement with the health system, regardless of their needs. That generally means monthly medical appointments with a doctor or high-level nurse at a central hospital. For many people living far from facilities, these trips often take an entire day due to lengthy travel and significant wait times. For the majority of patients who are generally healthy and responding well to their medications, this level of engagement with the healthcare system may be burdensome and actually discourage patients from remaining in care. For others with more complicated cases, this standardized level of care may be insufficient.
In the system in the Western Cape, healthy patients who are adhering to their anti-retroviral (ARV) treatment can pick up their medicine every two months from local service organizations rather than from a central hospital or clinic. Qualified pharmacists sort and package the medications, and then they are delivered to patients by mid-level healthcare workers rather than doctors or nurses. This lets people access quality services in their own neighborhood, reducing the burden on them and on the health system overall. To ensure that people are staying healthy and not developing resistance to their treatment, the Western Cape schedules everyone for an annual clinical exam with a highly qualified nurse. If there are problems, patients are immediately referred to a doctor for further examination.
I was also impressed by how the Western Cape collects the data required to understand which level of engagement is appropriate for the individual patient. They are phasing out their paper-based records and adopting an electronic health record that creates individual e-files for patients and links their lab results, hospital records, and other information under one file that can be accessed wherever an individual seeks care.
Why am I so excited about this approach?
First, this system takes into account the specific needs of the individual receiving care. By providing patients only the level of care they need, it leaves them more time to devote to their jobs, their families, and their communities.
Second, it enhances the impact of scarce healthcare resources—financial, human, and technical. By reducing the cost and effort while still keeping thousands of people healthy, it frees up resources that can be directed toward more specialized care for those who need it—or toward expanding access to treatment for those who don’t have it.
Third, the Western Cape’s approach uses smart IT solutions to meet patients’ clinical needs and providers’ logistical needs. It is preparing the way for an even more efficient, patient-focused health records system that can facilitate a better managed HIV treatment system at a lower cost to the public. This is especially important in countries like South Africa, where many patients might be on the move; electronic records can follow a patient much more easily than paper ledgers.
Approaches like these remain critical in our efforts to turn the tide on HIV. We have made huge progress against HIV in the past decade, thanks in no small part to programs like PEPFAR and the Global Fund for AIDS, Tuberculosis, and Malaria. The cost of ARV medicines has fallen by more than 99 percent, and more than eight million people now have access to lifesaving treatment. But we still face a situation where only half of all people who could benefit from HIV treatment are actually receiving it. And that means we have a moral obligation to be smarter about how we organize treatment programs so that people in treatment are able to live longer and so that fewer people die for lack of access to treatment.
Tracking Immunization
Seeing Ghana’s Health Care System in Action
I saw a healthcare system tracking and using data to great effect.


I got to spend two days in Ghana this week. It was my first visit there, and the time was really productive and inspiring. I got to watch an effective health system in action – from the decision makers at the national level to nurses who live and work in the villages.

I had heard that Ghana’s health system thrived on tracking information but I didn’t realize until I got there that it has an entire culture of data. Every immunization is carefully documented in the mother’s green booklet that tracks the health care of each child, as well as recorded in large registry books. That data moves up the chain to the sub-district and district levels. This kind of rigor may sound obvious, but in many places I’ve traveled, recordkeeping is so erratic that health workers don’t know how many babies live in their area of service, much less whether they’ve had all of their shots.
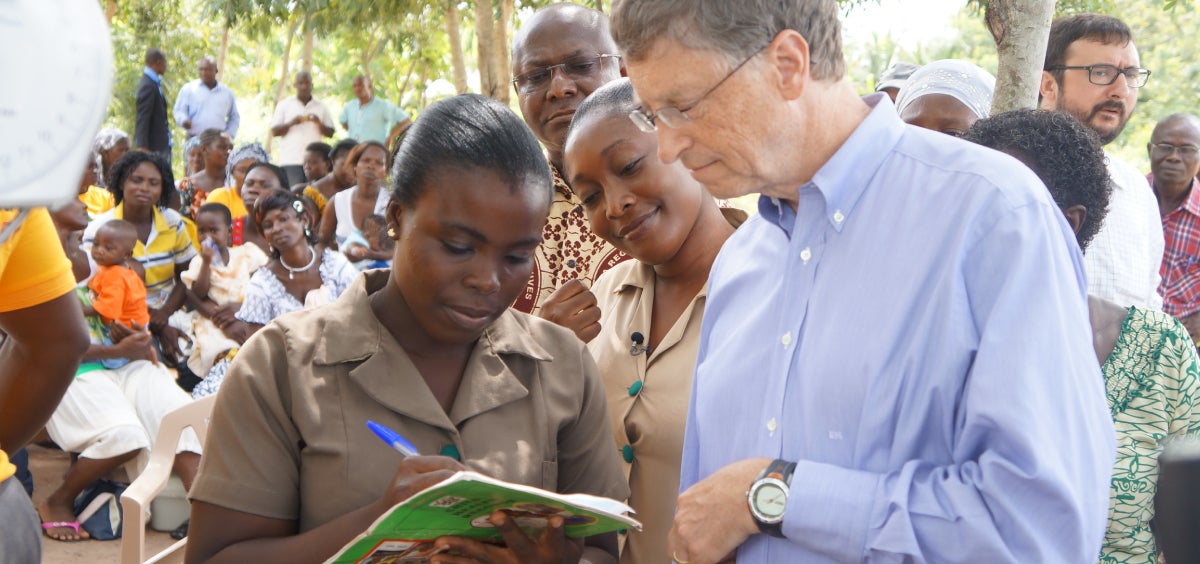
I met Patricia Antwi, district director of health services in Awutu Senya, about an hour’s drive north of Accra. Every month she gathers all of the sub-district heads to validate and pressure test their data with each other. Then every quarter all of the district leaders in her region meet and do the same. They track their work and adjust their planning and decision making based on such data as patient visits, products delivered and used, and immunization coverage rates. They openly debate what they have measured to help each other improve. They admit when it doesn’t go as well as it should.

Many of us are looking at potential digital strategies for record-keeping, but paper is pretty good.
The energy and commitment of the well-trained nurses was obvious. Alice Grant Yamoah runs the community health compound in the village of Ahentia. She lives in the heart of the community with three colleagues. A couple of days a week they go out in to the villages to treat or immunize children when their mothers don’t bring them in. Alice showed me how to give six-week-old Fredrick his rotavirus vaccine. Luckily for Fredrick these are drops that are fairly easy to administer. Still, both Fredrick and his mother were patient with someone doing it who clearly was less experienced than Alice and her colleagues.

There is a lot to learn from Ghana’s successes – but the most important in my mind is that countries need to have a really strong primary health care system that includes immunization as well as maternal and child health, malaria treatment and prevention, and other things that protect children and their families. It was a strong reminder to me that health is the magic lever. If you make progress there, it will help with all other things.
I’m a huge believer in the Millennium Development Goals, and I was also struck in Ghana over how important they are in helping drive focus and progress in the right places and in the right ways.
After visiting the clinics, I had the opportunity to meet with President John Dramani Mahama, who came into office in January. I was impressed by his strong focus on the MDGs. President Mahama and his ministers have a clear sense for where there has been great progress and where they still need to drive improvement.
The MDGs have really helped Ghana’s leaders focus their efforts, develop effective plans and measure their progress. Mahama was very clear about the good strides they have made in hunger and poverty as well as child mortality and education. He was equally candid about where they must redouble efforts to hit their targets in the areas of maternal health and sanitation. They still have a ways to go, but what’s exciting is that they have a strong direction and a solid plan to accelerate progress.
Going for GMOs
Farmers deserve options
Farmers have started hearing about GMO seeds, and they all want them.

This article by Sam Dryden, Director of Agricultural Development, Bill & Melinda Gates Foundation, was first printed on March 6, 2013, on the Impatient Optimists blog.
It is an exciting time to be working in agricultural science: we are seeing developments in crop research that are transforming farmers’ lives: tools that allow farmers to adapt and survive environmental challenges, and innovations that mean farmers can grow and eat more food so they are healthier and more productive.
Throughout my career developments in science have come hand in hand with criticisms and sometimes rejections of new research or scientific breakthroughs. While critical dialogue is important, the debate is only constructive when based on evidence instead of dogma.
Unfortunately, in one area of agricultural science, GMOs, many of the arguments have often steered towards dogma. So, it was refreshing when at the beginning of the year, a once outspoken anti-GMO activist, Mark Lynas, apologized for the myths he had helped create about biotechnology. He apologized for the scare tactics he and his peers had used to fill tabloid headlines and the trespassing and destroying of crop research he had led. He admitted—in a compelling speech to the Oxford Farming Union—that his previous views were “anti-science”. Once he had devoured the peer-reviewed articles and scientific data, he acknowledged the inconsistency between his position on climate change and his rhetoric around GMOs.
Most important of all, he apologized for contributing to depriving poor farmers of valuable, potentially lifesaving technology used successfully by most of the rich world.
It is this point that I feel most passionately about. What is so often missed in the debate about GMOs is choice: the choice for a poor farmer to consider planting a maize crop which could cope with droughts that are becoming ever more frequent; the choice to grow rice that provides the nutrition her child needs to prevent blindness; or put simply, a choice that we in the west take for granted.
Whether the tool being developed is produced by the latest technology or a more traditional approach, giving farmers access to solutions that deliver more productive or more nutritious crops, should be a decision based on scientific debate and research.
As in medicine, the development of new products should undergo rigorous safety reviews, guided by national regulatory bodies. Instead of arguing about the role of biotechnology in agriculture (interestingly, genetic engineering has produced insulin for diabetics without any alarm or calls for a complete ban), we should concentrate on ensuring that products—whether they are new seeds or new vaccines—are safe and effective.
Once proven (and so far, GMOs have been proven safe and effective), the use of these tools must be a choice for farmers to make. And farmers are choosing GMOs in their millions: GMO crops are the fastest growing technology (in the US, in Brazil, in India, Argentina) – because when farmers have access to more productive, less resource intensive crops, they seize the opportunity.
Since Bt Cotton (insect resistant) was introduced to Indian farmers in 2002, this GM cotton has grown to now account for approximately 90% of all cotton grown. During this past cropping season in India, roughly 6 million small holder farmers planted over 8 million hectors of insect resistant cotton.
The environmental impact, in the US alone, has been huge—cotton farmers have been able to cut back from 10 to 12 sprays per season to one. That’s less spraying of chemicals, less toxic agents impacting on the wildlife, marine life and on the children walking through fields. The same is possible throughout the developing world.
It is not just GM technology that is delivering positive results, innovations in conventional breeding are also benefitting small holder farmers. Our partners at the International Rice Research Institute in Bihar, India developed Stress Tolerant Rice for Africa and South Asia (STRASA). This new rice can survive up to 20 days underwater so when rains flood their fields, farmers are now getting twice the yield compared to the old rice variety. The impact on farmers’ lives is enormous—in a flood year, they have seen their incomes double.
STRASA has reached 3 million rice farmers in South Asia. But that’s just the beginning. Farmers have started hearing about these seeds, and they all want them. In the next six years, we expect 20 million farmers to plant these new varieties.
By adopting new technologies (whether it is genetic modification, conventional breeding or any other approach) farmers are making a loud statement about the importance of choice to them. However, their voices are rarely heard in this debate.
Hopefully soon it won’t be old hats like myself or Vandana Shiva arguing anymore, but the young scientists and farmers themselves who are seeing the benefits of all the tools in the box.
It is time to share their stories with the rest of the world. I urge you all to step forward and make your voices heard.
CIMMYT
Mexico will lead innovation in agricultural development for the world
Mexico is at the forefront of advances in agricultural development to help poor countries become food self-sufficient.

Building on its success a half-century ago pioneering new varieties of wheat and maize that saved a billion people from starvation, Mexico is again at the forefront of advances in agricultural development to help poor countries become food self-sufficient.
Combining the latest breakthroughs in agricultural science and farming practices with digital technology, Mexico’s innovative efforts will enable even the poorest farmers to grow and sell more crops.
Against the dramatic realities of climate change, a growing global population, rising food prices, and a shrinking agricultural land base, Mexico’s leadership in agricultural innovation is critically important—especially to the countries of Sub-Saharan Africa where hundreds of millions of people face severe hunger and poverty.
At the center of these efforts is Centro Internacional de Mejoramiento de Maíz y Trigo (CIMMYT), where Mexican and international researchers have worked for decades to develop higher-yielding, more resilient seeds for maize and wheat, and to introduce better agricultural practices that help farmers be more productive. One of CIMMYT’s greatest strength is its partnership approach. In addition to bringing together the world’s leading scientists and agricultural experts, CIMMYT has also involved farmer associations, the private sector, governments, international organizations, and NGOs in developing effective solutions to meet the needs of poor farmers worldwide.
This week, CIMMYT will be celebrating the completion of new agricultural research and training facilities made possible through the financial support of Fundación Carlos Slim. These state-of-the-art labs and greenhouses will ensure CIMMYT’s continued leadership developing high-yielding maize and wheat varieties equipped to tolerate the stresses of climate change. Expanded training facilities will enhance CIMMYT’s ability to develop and deliver resource-conserving farming practices and advance digital technologies that enable poor farming families to increase their productivity and income.
Helping poor farming families increase production in a sustainable way, and sell more crops, is the most effective way to reduce hunger and poverty over the long term. This has been proven in Mexico, India, Pakistan, Brazil, China, and many other countries over the last half century.
The unique partnership between CIMMYT, the government, and our foundations ensures that Mexico will continue to lead in agricultural development—first in Mexico and then the rest of the world.
The new infrastructure funded through Fundación Carlos Slim will enable CIMMYT to carry out cutting-edge agricultural science using the latest digital innovations, and to accelerate the use of mobile technology to provide farmers everywhere with vital information about weather, prices, and new techniques to improve their productivity. The Mexican government’s MasAgro initiative is helping farmers adopt more sustainable and profitable farming practices to increase food production. As these agricultural advances achieve scale in Mexico, the Gates Foundation will ensure that they reach maize and wheat farmers in Africa and South Asia, along with the resources needed to improve productivity.
Fifty years ago, Mexico’s leadership in agricultural innovation helped lift hundreds of millions of people in Latin America and Asia from hunger and poverty. More recently the UN’s Millennium Development Goals have reduced the number of people living in extreme poverty by half, since 1990.
The world is counting on Mexico to continue leading the way in agricultural research and sustainable farming practices to ensure global food security. Meanwhile, the global community must do its part by aligning around a new set of goals—including an agricultural productivity target—and achieving measurable outcomes that improve the lives of the world’s poorest people.
Gene Banks for Crops
Mexico, Carlos Slim, and me
Mexico and philanthropists like Carlos Slim are helping lead the global fight against hunger and poverty through agricultural development.

This week I’m excited to be in Mexico for a series of events with Carlos Slim, probably Mexico’s best-known business leader, whom I’ve enjoyed getting to know for his business insights—but also because of some of the innovative approaches he’s taking to philanthropy.

We’ve been invited by the International Maize and Wheat Improvement Center (known by its acronym in Spanish, CIMMYT) to help launch new facilities at its headquarters near Mexico City. With a staff of 1,100 in Mexico and 13 regional offices around the world, CIMMYT is helping reduce hunger and raise living standards in many poor countries through programs focused on increasing maize and wheat productivity. Our foundation has invested in CIMMYT, and Carlos Slim has been a big supporter.
Carlos is a very interesting guy. His father immigrated to Mexico from Lebanon. Carlos started several businesses when he was quite young and was already very successful by his mid-20s. His interests in construction, real estate and mining eventually branched out into many other businesses, including Mexico’s largest telecommunications company. He reminds me a little of Warren Buffett in his ability to find undervalued investment opportunities. I’ve enjoyed the time I’ve spent with him, getting to hear his thoughts on business trends and the future of Latin America.
Among many other great projects, the Slim Foundation has funded the new CIMMYT facilities that we’re helping open this week. Carlos’ foundation and ours have collaborated before in helping launch the Salud Mesoamérica 2015 initiative to support health projects in Chiapas, Mexico and across Central America.
This week we’ll get a chance to tour the new CIMMYT facilities including the gene bank, which holds the genetic diversity of 130,000 wheat and 28,000 maize varieties worldwide. This information is being uploaded onto databases that will be available to plant breeders everywhere. We’ll also get into the field with farmers who’ve been helped by the MasAgro project, sponsored by the Mexican government to help strengthen food security through R&D, capacity building and technology transfer.
One reason why I always enjoy going to Mexico is because of the country’s incredible progress, which has been really encouraging for me to get to see as I’ve spent time there over the years first for Microsoft and lately for our foundation. Despite the many challenges Mexico still faces, Mexico’s extreme poverty rate (those living on less than $1.25 per day) went from 13.6 percent in 1996 to 4.03 percent in 2010 (as per latest World Bank figures). A major driver in reducing poverty has been agricultural development, especially innovations that have helped improve crop yields for smallholder farmers, whose lives have improved a lot as a result.
Part of what makes this week’s visit particularly exciting for me is that the expansion of CIMMYT represents a very important and positive global trend: newly industrialized countries such as Mexico, China, India and Brazil are becoming leaders in efforts to help less developed countries. Mexico is in a great position to work closely with poor countries both because of its progress and because of its quite advanced technical capabilities in agricultural development. CIMMYT is a prime example of that.
Poor countries, donors and rapidly growing countries are increasingly working together in partnerships that I believe are a model for how to deploy the world’s combined resources. These sorts of partnerships, combined with rigorous goal-setting and measurement, can produce enormous benefits for the poorest around the world.
“Developing Countries”?
The River of Myths by Hans Rosling
Hans Rosling shows how countries are making progress in saving lives.

Hans Rosling shows how measurement reveals incredible progress in saving the lives of children in what were once labeled "developing countries." If the few countries that still have high child mortality rates can follow the path of Ethiopia, preventable child deaths may be history by 2030. We must continue to closely measure this progress.
Video created in partnership between The Gates Notes and Gapminder. #BillsLetter. License: Creative Commons 3.0.
Closing in on 1%
Turning the Corner on Polio in 2012
The Global Polio Eradication Initiative is making important changes.

Working to support the effort to rid the world of polio has taken me to some exotic places. But earlier this month, it took me to Washington, DC (I suppose you could argue this is also quite an unusual spot) to talk with policy makers about the historic opportunity we have to end polio forever.
My conversations with lawmakers gave me a chance to discuss some of the doubts people have expressed about whether we can really do this. But it also provided the opportunity to bring lawmakers up-to-speed on the results of important changes in the Global Polio Eradication Initiative’s (GPEI) approach—including cool new technology being used and the increased engagement on the part of governments in the countries where polio transmission continues.
In my opinion, the changes and progress in 2012 have made for the most convincing case yet that ending polio is possible—and is one of the most concrete accomplishments possible for global health.
For more than 10 years, we have been 99 percent of the way toward ridding the world of polio. Since then, every few years the global community would vow that year would be the year when polio transmission would stop.
However, 2012 is notably different from the earlier stagnation in progress. And while the global program hasn’t stopped transmission of the wild polio virus everywhere as some had predicted, it did close a big gap in that last one percent when India became polio-free early in the year after a long and hard battle to protect more than 172 million children under the age of five from polio. This was incredible tough terrain in which to run thousands, if not tens of thousands of vaccination campaigns. So, the lessons learned from India’s success are serving as a great guide for what’s needed in the remaining three countries where polio transmission persists—Nigeria, Pakistan and Afghanistan.
There’s no doubt that these countries aren’t easy places to get rid of the disease. There are a number of factors that need to be in place including improved campaign quality, meeting the program’s global funding needs, and anticipating political challenges.
I heard from U.S. lawmakers that the news regularly coming out of Afghanistan and Pakistan has led to reasonable concerns about the role insecurity plays in being able to reach children with vaccines. But in the last 11 months, incredible efforts are being made in these two countries by government officials, religious and community leaders and non-government organizations to negotiate access to children in hard-to-reach places.
And those efforts are paying off.
The polio program has been partnering with a number of NGOs to conduct negotiations to secure access to children, leading to breakthroughs in the past few months. In Afghanistan, the average number of inaccessible children in thirteen of the highest risk districts of the country has been reduced by more than half, from nine percent in June 2012 to 3.4 percent this November. And in the Terah Valley in Pakistan, where children hadn’t received vaccines in three years, approximately 30,000 children were reached with the polio and other critical vaccines during a vaccination campaign earlier this fall.
On the other front, in Nigeria, while cases have actually gone up this year, there is a full-scale effort to revamp the program, with many changes based on what vaccinators in India implemented to great success. Included in these changes are decreases in the size of vaccination teams and the addition of female vaccinators, tracking of nomadic populations, rigorous microplanning and scaling up of additional staff to help with all of these activities.
Another major innovation that is leading to early reports of impressive progress is the work on GIS mapping and GPS tracking to improve polio campaign planning and performance. (It’s a really ingenious use of the technology that you can learn more about here.) GPEI’s focus on using the polio program to increase routine immunization is ensuring that the polio program has an even broader long-term impact on the population.
The Independent Monitoring Board of the GPEI also notes the positive changes in a report released last week and their conclusion that the GPEI “has never been in a stronger position” reflects what I’m seeing too. Their assessment about what comes next for the history books is telling: “The time is momentous for public health history. A final concerted effort could indeed mean writing the story of polio’s last stand.”
I couldn’t agree more.
Join Us
World Polio Day: A Day to Learn, Act, Donate
Thanks to everyone working to end polio. Let's keep at it.

Today is World Polio Day, a day to celebrate the remarkable progress we’ve made in the fight against polio and to focus on the urgency of the work we still have to do. But equally important, it’s also a day to say “thank you” to the millions of people around the world who have generously given their time and money to this critical effort.
Ending polio is my top priority in my work at the foundation and I’m grateful for the opportunity to be part of this amazing public health campaign. Right now, the world has the opportunity to change history by ending polio forever.
In 1988, the year the global campaign against polio began, more than 350,000 children in 125 countries were paralyzed by the disease. Today, just three countries exist where polio transmission has never been stopped. And the number of new polio cases this year is down to 171 (compared to 467 cases this time last year). This number represents the fewest number of new cases in the fewest districts in the fewest countries in the world.
This is great progress.
And it kicked off this year with news that India—the second-most populous country—became polio-free in January and has been for more than 18 months. If we can rid India of polio, I’m optimistic we can do it anywhere. But we need to seize this opportunity and partners and donors need to act now.
For people who live in countries or regions that got rid of polio years or decades ago – like the U.S. and Europe – the disease might seem kind of abstract. But as long as there is a single case of polio anywhere in the world, no country is safe from the risk of reinfection. We have seen reinfection occur a number of times in recent years in countries that were previously polio-free. In a world of increased mobility, we all stand at risk until the job is done.
To ensure success, we need to fully fund polio campaigns and routine immunizations. We need continued leadership and accountability. And in regions where there are wars and conflicts, we need to ensure the security of vaccination teams so they can get to children - even in the most difficult areas.
I’m confident we can finish the job. We have an effective global polio program and real progress is being made.
We have a once-in-a-generation opportunity—now—to end polio forever and to leave in its place stronger health systems that can deliver life-saving vaccines to protect all children from vaccine-preventable diseases. You can be part of ending polio forever. It costs less than $1 to vaccinate a child against polio. Will you join this global effort? Here’s where you can learn more, act, or donate.
Someday we can retire World Polio Day. Let’s make that day come soon.
A Good Team
Partnering with Bono on foreign aid
For the past decade, we've teamed up to speak in support of aid.

This week, Bono and I met with European leaders to encourage them to renew their commitments to fund development assistance programs that help the world’s poorest. Bono is incredibly dedicated and it was great to partner with him on telling the aid story.
Giving in Tough Times
France committed to foreign aid
I'm thankful that France renewed its development commitment.

I was in Paris this week with Bono, talking about the importance and effectiveness of foreign aid with senior French officials, including France’s new President, Francois Hollande. I’m excited that France remains committed to development, even in these tough budgetary times.
“Last Mile” to Polio
Digital Mapping Technology Helps Polio Vaccinators Zero In
Health workers are using digital mapping to target polio in Nigeria.

One of the challenges getting from 99% to 100% on global polio eradication is making sure that all children are getting the multiple doses of the polio vaccine necessary to build up immunity.
To stop polio from circulating, you need to ensure that most children under the age of five receive several doses of the vaccine to build up their immunity. This is very difficult when there are hundreds of remote villages and hamlets that vaccinators don’t know about, nomadic tribes, and people in a castes or religious sects that don’t mix with the rest of the population.
Recently, public health officials began using GIS technology in Nigeria—one of the three remaining polio-endemic countries—to improve the quality of maps that tell vaccinators where to go. They are also using GPS technology to monitor the movement of vaccination teams. This kind of surveillance reduces the chances a team will miss an area that still harbors the disease.
The global health community has done an amazing job on polio, reducing the number of paralysis cases from 350,000 in 1988 to less than 200 so far this year. In 1988, more than 125 countries were endemic. Today, only three remain.
Yet, people sometimes ask me why we haven’t finished the job. It’s an understandable question since most countries got rid of polio a long time ago. One of the biggest reasons is that polio is a highly-contagious disease that travels quickly and easily. Another is the need to give each child multiple doses of the vaccine.
The use of digital mapping technology underlines the minute level of detail, planning, and organization required to completely eradicate polio. I’m optimistic that it will really help vaccinators cover the “last mile” in the delivery of polio vaccines.
Meanwhile, we can’t afford to ignore the other important pieces necessary to eradicate polio—sustaining political will and funding so vaccinators can reach children in every village, and ensuring accountability so the disease has nowhere else to go.
A Targeted Effort
GIS Mapping & GPS Tracking for Polio in Nigeria
A digital mapping system is being used in Nigeria to help health workers target specific areas for immunization efforts in the fight or eradicate polio.

In order to deliver vaccines, immunization teams go door-to-door throughout the country, including settlements in remote, rural regions.
Before going into the field, these teams use a process called “microplanning” to determine where they need to go in order to deliver the polio vaccine.
Before Geographic Information Systems (GIS) maps were made available through the mapping project, hand-drawn maps popularly known as “cartoon maps” were used to show the distribution of settlements. These maps were drawn from memory and not based on real geographical data.
GIS combines satellites, mobile device and mapping software capabilities to capture, analyze and present data as legible and informative maps.
The imagery of states is downloaded and organized for local government area (LGA) and ward map creation.
These maps make it possible to read distance and proximity with realistic placement of mapping features, to ensure that all settlements and hamlets are visited by vaccination teams, and the correct number and type of teams are deployed.
Phones are loaded with tracking software and the final settlement list before the vaccination teams are sent out in the field.
These vaccination teams are using tracking devices in the field. The phones collect geo-location readings through GPS.
The data from the phones is then processed in the GIS lab.
Detailed analytics report tracking results for each settlement.
These results make it easy to identify which settlements were missed and need to be revisited.
In Europe with Bono
Europe with Bono, defending aid
Shoring up support for international development assistance programs.

I spent Wednesday in Paris, talking about the importance and effectiveness of foreign aid. My partner in many of those meetings was Bono, who has used his voice so effectively to advocate for development aid and the needs of the poorest people on earth.
By any estimation, my few days in Europe were off to a good start.
We spent the better part of the day meeting with senior French officials, including France’s new president, Francois Hollande, his finance minister, Pierre Moscovici, the Minister of Foreign Affairs, Laurent Fabius, and their new Development Minister, Pascal Canfin.
France plays a critical role in encouraging the European Union to keep its commitments to overseas development assistance programs, particularly in the face of Europe’s economic difficulties. Its own commitment to foreign aid is a tremendous example to other donor countries. That was the context for our meetings.
President Hollande was clear that he remains committed to aid, and that he is an advocate for both the effectiveness of foreign aid when it is carefully done, and the responsibility developed countries have in working with the developing world. France has a remarkable history of support for Africa and for its assistance efforts around the world, with organizations like Médecins sans Frontières. The President also spoke about how aid can benefit both the recipient and donor countries.
France’s finance minister Pierre Moscovici made this point last month when he noted that Europe’s growth over the next 20 years will depend heavily on Africa’s growth and development. Ensuring that all Africans have a chance for a better future is not only the right thing to do, but also the smart thing to do from an economic standpoint.
We had a good exchange about getting the most out of every Euro of aid. I’m a big advocate for the incredible impact that investments in vaccines can achieve, and was very happy to hear the President specifically call out France’s commitment to staying involved with the Global Fund, which provides funding for programs to fight AIDS, TB, and malaria. France should be particularly proud in their leadership with the Global Fund. Their help is making a real difference in millions of lives around the world.
Support from leaders like President Hollande is critical to preserving those life-saving investments in aid and explaining why staying true to the EU goal of devoting .7% of national budgets to foreign aid is the right course.
Bono was very persuasive about the impact foreign aid is having, as well as the devastating consequences withdrawing it could have on poor countries, particularly in Africa.

I was really pleased with our meetings. They took place in spectacular surroundings (the Élysée Palace is a stunning example of French style and decoration). But the focus was on the poor, on both sides of the table. And that made for a very good first day in Europe.
Low Cost, High Yields
The MenAfriVac Vaccine: an Amazing Success Story in Global Health
What the launch of a new meningitis vaccine means for Africa.

Since Melinda and I first got involved in philanthropy, we’ve learned a lot about how to make the foundation’s investments more strategic and impactful.
We focus on problems that affect the most people with the most urgent needs, and on filling gaps that others can’t. We look for opportunities to use science and technology to create breakthroughs. And we work collaboratively with others to help create scalable, sustainable solutions.
Even after you’ve done all the analysis, though, you can never say with absolute certainty how things are going to go. But as we approach the second anniversary of the launch of a vaccine that is finally taming meningitis across Sub-Saharan Africa, I’ve been thinking that it’s a great example of when all of the pieces fall into place.
For more than 100 years, devastating waves of meningitis swept every few years through the 26 countries that have come to be known as the meningitis belt. Each time, the epidemics left death, disability, and financial disaster behind. Meningitis is caused by the inflamation of the protective membranes covering the brain and spinal cord.
It would strike the young most often and could kill within hours. Without antibiotics, 50 percent of those infected would die. Even with antibiotics, one in 10 people wouldn’t survive two days. Among remaining survivors, one in every four was left with a permanent impairment—ranging from mental retardation, seizures, paralysis to hearing loss or an infection requiring the amputation of a limb.
After the largest meningitis epidemic wave ever recorded swept across Africa in 1996 and 1997—infecting a quarter of a million people and killing 25,000—African health ministers were desperate for an alternative to the existing polysaccharide vaccine, which provided only short-term relief after outbreaks occurred and could not reduce the risk of future epidemics.
In 2001, our foundation funded a 10-year partnership between the World Health Organization and Seattle-based PATH to develop an affordable, new vaccine that experts hoped would last longer and do a better job of interrupting transmission of the disease. Over the next decade, a remarkable collaboration grew to include many private sector and public sector partners.
In December 2010, the new MenAfriVac vaccine was introduced in three countries: Burkina Faso, Mali, and Niger. Mothers queued up early with their children, fearful that health workers would run out of the vaccine. They need not have worried. In four weeks, a remarkable 20 million people were vaccinated.
The results are as good as we hoped for. Innovative science and technology led to development of a vaccine at less than one-tenth the cost of a typical new vaccine. Strategic partnerships were also key to delivering an affordable, sustainable vaccine and getting it quickly to people most in need.
In Burkina Faso, a country which reported 40,000 meningitis cases in 2006 and 2007, 12 million people were vaccinated. Since 2010, there have been no new cases of Meningitis A reported among vaccinated populations.
Over the next three months, another 50 million people in seven countries will receive the MenAfriVac vaccine, bringing to nearly 100 million the number of people who have received it in just two years.
There is still a lot of work left to do. Hundreds of millions more people in Sub-Saharan Africa still need to be vaccinated. But for those spared the suffering of future meningitis epidemics—and for those of us working to eliminate disease and reduce poverty—the MenAfriVac vaccine is a reminder of why aid matters and the impact we can achieve working together.
Photos from My Trip
Snapshots of UN Week
Photos from my week in NY at the UN session on eradicating polio.

While in New York, Sandro Rosell and I recorded a short video together talking about the foundation’s partnership with FC Barcelona to work toward saving children’s lives around the world.

Sandro Rosell (L), the President of FC Barcelona and the FC Barcelona Foundation and Ramon Pont (R), the Vice President and Director of FC Barcelona have been tremendous partners in using their club and its worldwide fan base to raise awareness of polio with their “More than a Goal” campaign.

Dr. Ahmad Mohamed Ali, President of the Islamic Development Bank, and I signed a Memorandum of Understanding between the foundation and the IsDB. Their financial support will make a big difference. But in addition, the support and commitment of so prominent an Islamic institution will be of great help to our efforts in places like Afghanistan and Pakistan.

I enjoyed dinner with senior leadership from the Islamic Development Bank and learned a lot while in New York.

I started Day Two in New York with an early meeting with President Karzai of Afghanistan. His country is one of the last three where polio remains at large. He’s truly on board for doing everything he can to work on polio. Afghanistan presents daunting challenges – but it’s encouraging to see his support and leadership.

The main reason for my trip to New York was to attend a meeting hosted by Ban Ki-moon, the Secretary-General of the United Nations. At the meeting, heads of state from Afghanistan, Nigeria and Pakistan stood alongside donor government officials and new donors from the public and private sector to outline what we need to do to stamp out polio. It was a remarkable display of solidarity, energy and commitment. It was an honor to be there.

A Busy Day in NY
At the UN: Talking health and development
As the United Nations General Assembly convenes in New York this week, I’ve been asked to come and speak about the need for nations around the world to recommit to eradicating polio. Here are some notes from my first day at the UN.

UN Week is a crazy time in New York. Getting around can be tough with increased security, various protesters, and heads of state and other important visitors coming and going. But as I wrote yesterday, it’s also an incredible opportunity to see people, and to discuss issues of real importance to the world.
I got a chance to spend some time with UN Secretary General Ban Ki-moon this morning. He’s about the busiest guy in New York this week, so it was super nice of him to make the time. We got to talk about polio, and the important meeting he’s hosting tomorrow, which is the main reason I’m here. Having his voice continue to make the case for why we need to end this disease in the few places it remains is so important. As Secretary General, he’s called out five of the world’s major "killers" he wants to see eliminated during his second five-year term. Polio is on that list, along with malaria, pediatric HIV infections, maternal and neonatal tetanus, and measles.
In the morning I had the chance to meet the Prime Minister of Ethiopia, Hailemariam Desalegn, who was sworn into office just last week. I was really happy to get to meet him because Melinda and I both had a great working relationship with his predecessor, Meles Zenawi, who died in August of this year. It was a great loss for Ethiopia, and for Africa and the world. But I was impressed with the new Prime Minister, not only for his thoughtfulness and knowledge about the issues we work on as a foundation in Ethiopia, but also for his commitment to continuing the policies of Prime Minister Zenawi, which have made real progress in helping the people of Ethiopia. Some of the foundation’s most exciting projects are happening in Ethiopia, particularly our partnership with the government in improving agricultural output for small farmers. I was in Ethiopia earlier this year, and I told the Prime Minister I looked forward to getting back there sometime in the future.
One Year Polio-Free
Angola’s Re-Match Against Polio Underscores the Urgency of Global Eradication
Angola marks a full year without a new case of polio, evidence that with sustained focus we could end polio forever.

There have been many amazing success stories in the global campaign to eradicate polio. This past month adds another—Angola marked a full year without a new case of polio. Angola’s accomplishment is the latest evidence that we are extremely close to ending polio forever. Earlier this year, the World Health Organization (WHO) announced that India had gone a year without a new case of polio—a remarkable accomplishment considering its size and population. A sustained global public health effort over the last 24 years has led to more than a 99 percent reduction in polio cases and only 650 new cases in 2011.
Polio is a formidable foe and Angola is one of the world’s poorest nations with numerous health challenges to tackle, which makes Angola’s achievement especially noteworthy. After eliminating its own poliovirus over a decade ago, Angola persistently fought to stop transmission of polio virus imported on several occasions from outside the country. The last importation of the polio virus took several years and over 30 polio vaccination campaigns to stop the transmission.
Angola’s experience with polio is a stark reminder that countries that have eliminated polio within their borders are not safe from a new polio outbreak until the entire world is free of this vaccine-preventable disease. An impoverished country of 18 million in southwestern Africa, Angola originally defeated polio in 2001 despite decades of civil war, showing that polio can be eliminated under challenging circumstances. Angola remained free of the disease until 2005, when polio returned due to cross-border transmission. Porous borders and water and food contamination—key ways polio spreads—are especially big challenges in countries like Angola. But new outbreaks can occur in any country, including China and Tajikistan last year, and will continue to be a threat everywhere if the world does not ensure that we eradicate polio.
Angola’s leaders and citizens deserve a lot of credit for their determination to eliminate polio not just once, but twice. This is no easy or inexpensive feat, especially for poor countries like Angola, which must use limited resources for many other pressing health priorities to re-tackle polio. Angola, which now shoulders 90 percent of the operational costs of these campaigns, succeeded because of a deep commitment among government officials at all levels and the involvement of community and religious leaders, NGOs, and volunteers. Officials deployed huge vaccination campaigns involving thousands of health workers and volunteers going door-to-door, positioned on main streets, and canvassing markets. In Cazenga – one of the poorest municipalities – volunteers were each assigned to stay in contact with 10 families to ensure that they received regular checkups and vaccinations.
Like all 125 countries that have gotten rid of polio since 1988, Angola’s leaders and citizens also deserve the global resolve needed to ensure that no country ever has to go back and re-do the hard, expensive work that’s already been done to protect their children from polio. This will ensure that these countries can focus their resources on other pressing health priorities.The only way we can achieve this monumental goal is for all countries to take responsibility for making the world polio free. This means:
- We need to increase political will in existing and new donor countries to fill the Global Polio Eradication Initiative’s existing funding gap of almost $1 billion through 2013, and to commit to funding the GPEI for the long term until the job is done.
- Endemic countries—Afghanistan, Nigeria and Pakistan—where polio transmission has never been stopped must continue their strong political commitment to do everything they can to protect their children and the world’s children from polio.
- Countries such as Angola and India need to remain vigilant, continue dispensing the polio vaccine and improve routine immunization to ensure their children stay protected from vaccine-preventable diseases.
- Polio eradication partners such as the WHO and UNICEF must work on improving vaccination campaigns and protect every child with the polio vaccine.
We must not let go of the idea that we can ensure that all the world’s children will be safe from polio and on their way to protecting all children from vaccine-preventable diseases. I know I don’t.
WC: Winners' Circle
And the winners of the reinvent the toilet challenge awards are…?
Today I attended the Reinvent the Toilet Fair — a fascinating learning experience and an important step in providing safe sanitation for everyone in the world.

A year ago, the foundation launched an initiative to tackle the problem of sanitation in the developing world. We called it the Reinvent the Toilet Challenge. In this photo gallery you can learn more about each of the grantees and their sanitation solutions.
This week in Seattle, the foundation is holding a Reinvent the Toilet Fair. Today I awarded prizes to three universities who responded to our challenge a year ago to come up with solutions for capturing and processing human waste and transforming it into useful resources. The winners included: first place to California Institute of Technology in the United States for designing a solar-powered toilet that generates hydrogen and electricity, second place to Loughborough University in the United Kingdom for a toilet that produces biological charcoal, minerals, and clean water, and third place to University of Toronto in Canada for a toilet that sanitizes feces and urine and recovers resources and clean water. A special recognition was awarded to Eawag (Swiss Federal Institute of Aquatic Science and Technology) and EOOS for their outstanding design of a toilet user-interface.
A solar-powered toilet that generates hydrogen and electricity
California Institute of Technology, USA
A self-contained, solar-powered toilet and wastewater treatment system. A solar panel will produce enough power for an electrochemical reactor that is designed to break down water and human waste into hydrogen gas. The gas can then be stored for use in hydrogen fuel cells to provide a backup energy source for nighttime operation or use under low-sunlight conditions.
A sanitation system that converts human waste into biological charcoal
Participating organizations: Stanford University and the Climate Foundation, USA
A self-contained system that pyrolyzes (decomposes at high temperatures without oxygen) human waste into biological charcoal (biochar). After the fair, the system will be shipped to Nairobi to process two tons of human waste daily, at a facility located in the slums.
A toilet that converts human waste to fuel gas
Delft University of Technology, The Netherlands
A toilet system that applies microwave technology to transform human waste into electricity. The waste will be gasified using a microwave-induced plasma. This process will yield synthesis gas (syngas), a mixture of carbon monoxide and hydrogen. The syngas will then be fed to a solid oxide fuel-cell to generate electricity.
Diversion for safe sanitation
Participating organizations: Eawag: Swiss Federal Institute of Aquatic Science and Technology; EOOS, Switzerland
A functional model of a urine-diverting toilet that recovers water for flushing. The urine and feces will be safely transported to a decentralized processing center. The water used for cleaning will be recycled by a gravity-driven biological membrane.
A toilet that produces biological charcoal, minerals, and clean water
Loughborough University, United Kingdom
A toilet that transforms feces into a biological charcoal (biochar) through hydrothermal carbonization (decomposition at high temperatures without oxygen and in water) of fecal sludge. The proposed system will be powered from heat generated by combusting the produced biochar and will be designed to recover water and salts from feces and urine.
A urine-diverting combustion toilet
National University of Singapore, Singapore
A toilet that uses biological charcoal (biochar) to dry and combust feces. The heat generated will be used to extract water from urine by boiling it under pressure. The system can be fitted with activated carbon and exchange resin to recover highly purified water.
A community bathroom block that recovers clean water, nutrients, and energy
University of Kwazulu-Natal, South Africa
A toilet system that can safely dispose of pollutants and recover materials such as water and carbon dioxide from urine in community bathroom blocks. The system will separate the urine from the feces and extrude the feces into thin strands for faster drying and stabilization.
A toilet that sanitizes feces and urine to recover resources and energy
University of Toronto, Canada
A technology for treating solid waste streams through mechanical dehydration and smoldering (low-temperature, flameless combustion) that will sanitize feces within 24 hours. Urine will be passed through a sand filter and disinfected with ultra-violet light.
Not Flush with Cash
Simple, affordable sanitation innovation in Durban
I met with sanitation experts in Durban who have developed a safer and inexpensive alternative to the pit toilets used by many poorer families around the world.

In 2009, during a foundation trip to South Africa, I met with Neal Macleod, head of Durban Water and Sanitation. Neal is a health expert working to improve sanitation so people no longer have to use pit toilets such as the one in the photo.

The typical developing world toilet is just a pit. You dig a hole in the ground, you put up a shack around it, and in some cases you put some kind of seat in there. There may or may not be water or toilet paper. It’s pretty unattractive, particularly the smell.
Neal showed me an improved toilet model called a Ventilated Improved Pit latrine or V.I.P. The Ventilated Improved Pit latrine is set up so that air flows down through the toilet, down into the pit and up through a pipe which dramatically reduces the smell problem. And by putting the right mesh wiring on the top of the pipe, flies can’t get in.
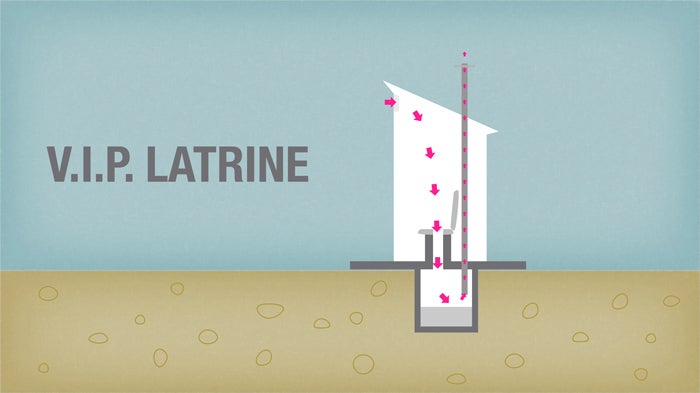
One challenge is that you’ve got to empty the pit. In preparation for emptying a pit latrine, large plastic containers are lined up behind the toilet.

The workers have to wear gloves and protective masks to empty the latrines.

Workers pump out waste from a pit latrine. They would remove the liquid waste by using a hand pump.

Workers empty the waste from a pit latrine into large plastic containers. Each pit would yield 25-60 of these huge buckets full of waste.

A Meeting in Zambia
Chief Mumena: Leading by Example on HIV
The fight against AIDS in Africa is filled with true heroes. Chief Mumena is certainly one of them.


The fight against AIDS in Africa is filled with true heroes. To my mind, Chief Jonathan Eshiloni Mumena is certainly one of them.
When I visited Zambia in March, I had the chance to meet with him. He is a senior chief of the Kaonde people, who live along Zambia’s border with the Democratic Republic of Congo. Chief Mumena is one of his country's most respected traditional leaders, and he has been using his voice to encourage Kaonde men to embrace voluntary medical male circumcision as a strategy to prevent HIV transmission.
The discovery that male circumcision can reduce a man’s risk of acquiring or transmitting HIV by up to 60 percent is an exciting breakthrough in HIV prevention, but the message about male circumcision's life-saving potential still hasn't reached enough people.
Traditional leaders can play an important role in expanding demand for male circumcision, and Chief Mumena is showing the way. A few years ago, his teenaged son came to him and said, “I want to go for MC” (shorthand for male circumcision). Chief Mumena had never heard of “MC,” and he asked his son a lot of questions because the Kaonde do not historically practice circumcision.
But when his son showed him a brochure and told him about the tremendous HIV prevention potential of male circumcision, the chief became a convert to the cause. He started to encourage Kaonde men to be circumcised. And as a way to lead by example, Chief Mumena had the procedure in 2011. He was 47 years old at the time.
Hundreds of Kaonde men have responded to his call to action by undergoing the short, nearly painless procedure at local clinics managed by the Society for Family Health.
Chief Mumena is attending this week’s International AIDS Conference in Washington, DC, to share his story and raise visibility for male circumcision.
Treatment is Working
Why I’m Committed to Turning the Tide on AIDS
A decade ago, almost no one in Africa was receiving drugs to treat HIV. AIDS was a death sentence. Now more than 8 million people in developing countries, the majority of them in Africa, have access to life-saving treatment.

Florence Daka is a healthy mother of four who lives in Lusaka, Zambia. She sees her children off to school every morning and works a full day cleaning offices.
That may not sound extraordinary, but it is. It’s extraordinary because Florence is alive and well and living with HIV, thanks to the effective treatment that she takes. What’s more, the medicines that Florence received during her last pregnancy helped her avoid transmitting HIV to her youngest son, Stephen, who is now a healthy two-year-old.
When I met Florence during a visit to Zambia earlier this year, I was struck by her story and how she and Stephen are living proof of the tremendous progress that we’ve made in the fight against AIDS.
A decade ago, almost no one in Africa was receiving drugs to treat HIV. AIDS was a death sentence. Now more than 8 million people in developing countries, the majority of them in Africa, have access to life-saving treatment. The cost of HIV drugs in Africa has plummeted by more than 99%, and most pregnant African women who are infected with HIV now have access to treatment to prevent mother-to-child transmission of the virus.
It’s important to celebrate this tremendous progress—progress that seemed unimaginable just a decade ago – and to stay committed to the fight against HIV. That’s why I joined government leaders, philanthropists, faith leaders, entrepreneurs and entertainers at the Kennedy Center’s Eisenhower Theatre last night to recognize what the world has achieved in turning the tide on AIDS.
This week, the International AIDS Conference will be held in the United States for the first time in more than 20 years. And last night’s Kennedy Center event – with 1,000 global health advocates in attendance—offered a great stage to share success stories and talk about the importance of sustained HIV funding.
I talked about the strong leadership that the President’s Emergency Plan for AIDS Relief (PEPFAR); the Global Fund to Fight AIDS, Tuberculosis and Malaria; and developing country governments have taken to expand access to treatment and prevention.
I also thanked public and private sector leaders in the U.S. for maintaining America’s long-standing commitment to HIV research and development (R&D). Our country still provides 70 percent of all funding for HIV R&D, including efforts to develop more effective and longer-lasting prevention methods and an HIV vaccine. Americans can be justifiably proud of the tremendous moral leadership that the U.S. has taken in producing breakthrough innovations in the fight against HIV.
But America isn’t in this effort alone. I’ve been honored to meet people around the world who are committed to funding and leading critical R&D activities. And I have told them that the Bill & Melinda Gates Foundation is committed to working with partners everywhere to accelerate the discovery and development of new tools to treat and prevent HIV.
Tomorrow, I will be part of a panel at the International AIDS Conference that will discuss what’s needed to sustain progress against HIV in tough economic times. I look forward to sharing my ideas in a follow-up post.
A Test Worth Taking
Florence Daka, an HIV-Infected Mother of Four
In Zambia, I met Florence, who was successfully treated for HIV.

On my trip to Zambia earlier this year, I visited the Coptic Mission Hospital in Lusaka and had a chance to meet with Florence Daka, a mother of four who is alive today because of the effectiveness of HIV drugs.
It was important to hear Florence’s story, because she helped me understand why the decision to get tested and take HIV drugs isn’t always so easy. In Florence’s case the drugs also prevented transmission of HIV to her newborn son—an example of what can be achieved if we keep our focus on HIV treatments, in addition to fundamental research. In Zambia, the spread of HIV from mother-to-child is one of the most frequent ways AIDS has spread—where more than 15% of the adult population is living with the disease but many do not know it.
A Tough Challenge
In Pakistan, Victory Against Polio is in the Hands of Local Officials
Pakistani leaders are working hard to support polio activities.

I met recently with a group of Pakistani national and provincial leaders waging war against polio in a handful of areas where the dreaded disease still exists.
Over the last 25 years, 122 countries where polio was once endemic have eliminated the disease. Just three countries remain: Pakistan, Afghanistan, and Nigeria. Reducing polio infections by more than 99 percent over the last quarter-century could not have been achieved without a sustained commitment from all countries to mount this successful global public health effort. But the hard work of reaching thousands of vulnerable children is largely a challenge that falls to local officials.
In Pakistan, eradicating polio is an especially unique challenge—although I’m optimistic, Pakistan will continue to make progress. A recent report by the Independent Monitoring Board affirms this optimism.
Last year, Pakistan had more polio cases than any other country. But since the beginning of this year, overall, polio cases in Pakistan have dropped by 67%, from 69 cases in 27 districts at this time last year, to 23 cases in 13 districts since the beginning of 2012.
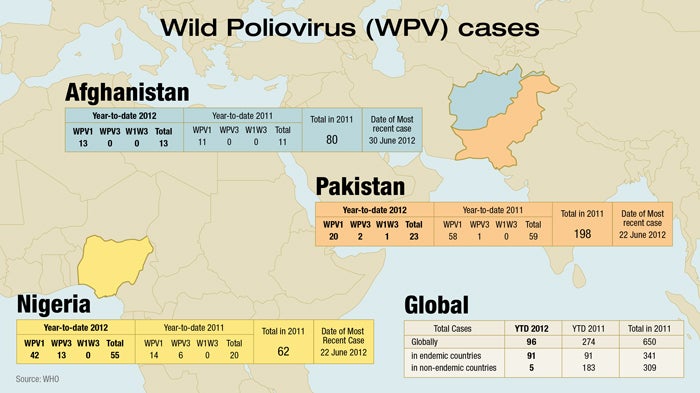
It recently devolved its national health ministry, which means provincial and local officials have to work extra hard to coordinate polio and immunization activities. There are areas such as the semi-autonomous tribal region in northwest Pakistan where conflict and insecurity prevent vaccination activities. Much has recently been written about new challenges that have arisen, including an alleged ban on immunizations by some local leaders in North and South Waziristan, Federally Administered Tribal Areas (FATA). While this further complicates running immunization campaigns in an already-challenging environment, efforts are being undertaken to address the situation. It also is important to note that this affects not even 1% of the country’s target population. However, there are still some areas where the management of local polio campaigns needs to improve. Pakistan is effectively tackling these challenges with new approaches and adopting lessons learned from India.
In the U.S. and other developed countries, we take the administration of vaccines for granted. Young children get immunized when they visit the doctor. But in Pakistan, heroic health workers often have to surmount obstacles, and even risk their lives to reach children who are unprotected. Vaccine teams are enlisting the support of religious leaders to help counter misperceptions about immunizations and suspicions that they are part of a plot. They also are adopting proven methods to reach children in migrant communities where vaccinator teams that speak the local dialect have been recruited to reach local populations and give them more confidence in their efforts. And where it’s encountered political instability and insurgency, the polio program has tried to coordinate with the Pakistani military to get access for vaccinator teams and to try to ensure their safety.
As of last month, there were 16 cases of polio reported in Pakistan.
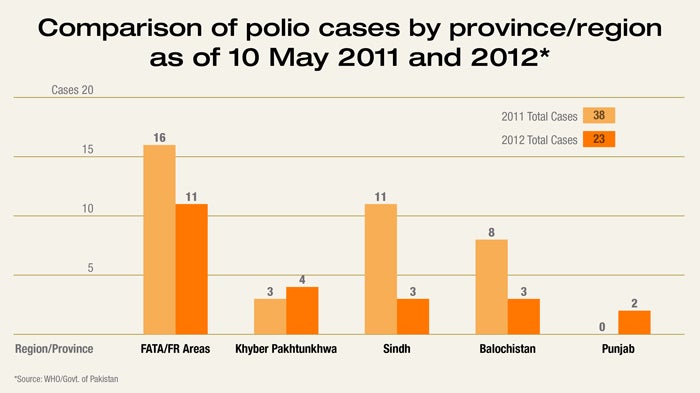
That doesn’t sound like a large number, and the progress that it demonstrates is worth acknowledging.
But polio is a cunning disease. Ninety-nine percent of the people who carry the virus don’t show any visible effects, so it’s hard to know who has it and where it’s traveling until a reported case shows up. In a country with a population of 175 million people, you can imagine how difficult this is.
But India has proven that it can be done in a country with a population of 1.1 billion. Earlier this year, it was removed from the list of polio endemic countries after going a full year without a new case of wild poliovirus. India’s success proves that polio can be defeated in the most challenging circumstances.
It was clear in my meeting with the Pakistani provincial leaders and several national officials who joined them that there’s a strong resolve to finish the job. They were very open about where efforts have fallen short. And the fact that the Pakistanis were willing to travel to India to meet with Indian health officials after their meeting with me really underscored their commitment.
India and Pakistan don’t always see eye-to-eye on things, so seeing the Pakistanis and the Indians sharing what is working and some of their common problems in solving polio was very encouraging. Their meeting was also a chance for India to help their neighbor, and a reminder that they need to stay vigilant in their own country.
Failing to completely eradicate polio would create a very real risk for the rest of the world - a resurgence that could affect tens of thousands of children worldwide getting infected. On the other hand, eradicating polio will result in benefits of up to $50 billion by 2035 in the world’s poorest countries. Our investment in polio eradication is also laying the foundation for delivery of other cost-effective health services—including vaccines for other preventable diseases.
Despite current challenges, my meeting with the Pakistanis and action taken on polio and vaccines by the World Health Assembly reinforce my confidence that we truly are on the verge of ending polio. India has proven that a strong commitment by political and community leaders, well-managed and high-quality vaccination programs tailor-made to local circumstances, and adequate financial resources can get the job done.
When it comes to polio, the Pakistanis and the Indians want the same thing we all do—a world in which no child ever gets this preventable disease again. But the responsibility to end this disease doesn’t just lie with the countries where polio transmission continues, we all have a responsibility to ensure a polio-free world.
One Success Story
HIV/AIDS & Avahan
The Avahan center is helping to reduce the spread of AIDS.

One of the reasons for my recent trip to India was to congratulate the team at Avahan on their fantastic work and transition to management by the government of India—this is an incredible achievement. The Indian government will be scaling the program and supporting it over the long term.
When I was in Bangalore recently, I visited an Avahan supported drop-in center for sex workers that is one of the success stories in India’s effort to reduce the spread of HIV. The center is run by a local community organization that provides counseling, medical help, HIV prevention training, and a microfinance bank to about 19,000 sex workers. This center is one of many programs which are part of the larger Avahan HIV prevention project. The program is targeted at millions of the people most at-risk for contracting and spreading the virus. The foundation helped get Avahan off the ground and has supported it for the last 10 years—its transition to government management is a great example of what collaboration with governments can achieve.
Meeting the People
The Urban Health Initiative in India
The Urban Health Initiative helps women in slums get contraception.

I always look forward to visiting India for the opportunity to meet people who are benefiting from projects we’re supporting in key health areas, like family planning, polio eradication, and HIV/AIDS.
On my recent trip, I spoke with several women in one of Lucknow’s urban slums who told me how grateful they are to have a choice of contraceptives. That hasn’t always been the case and there are still many poor women who don’t know about or have access to contraceptives. Efforts like the foundation-supported Urban Health Initiative are designed to change that by educating more women about contraceptive choices and practices like spacing births further apart.
This is a top health priority for the foundation because it directly affects the health (and often the survival) of poor women and their babies. And it offers them something that all mothers desire and deserve—the opportunity to provide their children with a high-quality education and the best chance of success growing up.
Exporting Hope
The Serum Institute of India
I toured the Serum Institute and met founder Dr. Cyrus Poonawalla.

Serum Institute is an impressive company that was founded by Dr. Cyrus Poonawalla and his brother in 1966 to manufacture low-cost vaccines for Indian use. Today their company makes more vaccines than any other manufacturer and delivers them to 140 countries around the world. And the great thing is their products are very high quality so they’ve really been able to fill a huge need for affordable vaccines. It was an honor to meet with Dr. Poonawalla during my visit to India. Serum’s contribution to global health has just been amazing.
20 Years of Growth
India’s progress
In India I saw how aid and spending on health can make a difference.

India’s progress over the past 20 years has been quite phenomenal. It deserves recognition especially now, as rich countries consider whether to continue investing in global development assistance despite all the economic problems they face at home.
India still faces many challenges. More than 400 million Indians live in extreme poverty. The country is home to half of all the world’s malnourished and underweight children and one fourth of the world’s tuberculosis.
But over the past 20 years, India has really emerged as a dynamic, influential country. It’s been one of the world’s fastest growing major economies, and it’s playing an increasingly important role in world affairs, including as a member of the G20 and the BRICS group of newly industrialized nations.
The current situation in India is quite hopeful. The country has a lot of talented people. The universities are improving. Government spending is going up because of the nation’s economic strength. Some reforms are needed, and that’s progressing, gradually. India represents all the challenges you face when you have lots of people living in poverty. And so India can contribute to how we solve problems globally.
A lot of progress has come from the nation’s culture of innovation, which has produced some really original and creative solutions. Yet, aid also has played an important role. Our foundation has invested more than $1 billion USD in programs to fight disease and poverty in India. I’m pleased with the results, and we will invest more in the future.
During my recent visit, I had a chance to see the latest progress on things that matter a lot to us: on eradicating polio and curtailing the spread of infectious diseases like HIV/AIDS and tuberculosis, for example. And I saw how India is emerging as a model and increasingly a catalyst for improvement in other developing countries. For example, India has become a world leader in the development of high-quality, low-cost vaccines and other bio-pharmaceuticals, which are playing a huge role in improving health not only in south Asia but also in Africa and elsewhere.
Ending Polio
It’s now been more than a year since the last new case of polio was reported in India. In February, India was officially removed from the list of polio-endemic countries.
This is especially great when you look at it in context. Three years ago, India had more polio cases than anywhere else in the world. Its polio problem seemed like the toughest to tackle. Compared with the countries where polio persists, India is bigger by far, with the most kids, and still has regions where sanitation is poor. Within the country there’s lots of movement, which tends to spread infection.
Yet, India really stepped up to the challenge on polio. The government funded its own eradication program. They really educated mothers about why vaccination is good for kids. Twice a year, 2 million volunteers prepare 800,000 vaccination booths around the country—at schools, hospitals, and community centers. They immunize more than 172 million children one by one. Working with partners like Rotary International, WHO, and UNICEF, they have built an impressive infrastructure for delivering health services to some of the most underprivileged children in the world. And they have been very persistent in following up to find kids, even the kids of migrant workers, to get vaccination levels up above 90 percent. And so the disease stopped.
India is very proud of this achievement, and rightly so. It’s a direct result of political will, dedicated resources, and rigorous management and accountability. The commitment of government leaders has been critically important.
And that commitment is helping with other health problems. By extending vaccination into the poorest and most inaccessible places, the drive against polio has helped establish better public-health delivery systems that can improve the well-being of millions of children and families.
India’s experience carries lessons for developing and newly industrialized countries around the world. It proves that success can be achieved – against polio and other diseases, as well – even in the most challenging circumstances.
Curbing HIV/AIDS & Tuberculosis
Another great example of India’s progress is in its work to halt the spread of HIV/AIDS. Our foundation has been helping with this for a long time. With a number of Indian partners, we started the Avahan program. It’s fighting HIV/AIDS in communities and at the street level, helping local groups deploy peer-to-peer counselors, distribute condoms and provide HIV testing, treatment and care.
Important leadership has been provided by the national government, which has increased funding for HIV/AIDS and established a national strategic plan that includes community-led HIV prevention. The National AIDS Control Organization has done great work. NACO and Avahan have contributed to a 50-percent reduction in the incidence of HIV/AIDS over the past six years. That’s saved India something like $100 million USD in health costs averted because of fewer AIDS cases.
Now, NACO is facilitating a smooth transition of Avahan to management by the state governments. This transition is very important and encouraging because it indicates India’s resolve to sustain the fight against HIV/AIDS for the long haul, which is what it will take to really beat this thing. This is a great example of what collaboration between funders and governments can achieve.
Lessons learned from HIV/AIDS work have helped with other critical health efforts, like the Ananya partnership, which is really scaling up programs to improve maternal and child health. India is also a model for other countries on how to scale up HIV prevention efforts.
The country faces many other health challenges. For example, India has the largest tuberculosis epidemic in the world, with nearly one thousand deaths from TB each day. But there’s a solid basic TB control program and a real commitment to getting TB under control. The government has an ambitious strategic plan to provide universal access to good diagnosis and treatment to all TB patients. This plan can prevent the emergence of multidrug resistant TB thru prompt diagnosis and appropriate treatment.
India has begun to execute this strategy by making TB a nationally notifiable disease, which means cases must be reported to authorities. This will help ensure they get the care they need regardless of whether they are being treated by government or private doctors.
India is also using its leadership in information technology, which could be a big help to government and private health providers in monitoring the spread of the disease, improving the efficiency of the TB control program and in treating patients.
Leading on Low-cost Vaccines
Just a few decades ago in India, many basic vaccines were hard to get. They were almost all imported from overseas. But today, Indian manufacturers play a critical role in driving down prices for vaccines and making them available to not only Indians but also millions of poor people worldwide.
One of the leaders in this transformation is the Serum Institute, in Pune. I visited with Serum’s chairman Cyrus Poonawalla and other executives. Their work is absolutely vital to our foundation’s work around the world, because Serum is extremely good at making high-quality vaccines for many different diseases – and doing it at low cost so that poor countries can afford them.
Serum has gradually evolved from making relatively simple vaccines for things like tetanus to making more advanced ones. In response to a request from African leaders for a better weapon against meningitis epidemics, Serum developed a vaccine for meningitis A, the first vaccine created specifically for poor countries. Serum is developing important new vaccines against rotavirus, which causes diarrhea and vomiting that kills hundreds of thousands of children in poor countries every year.
Serum's the world's highest-volume provider of vaccines – does it at very high quality, very low price. It’s a great example of the potential for innovation in developing and newly industrializing countries – innovation that can benefit poor people everywhere.
Achieving Progress through Collaboration
Prime Minister Manmohan Singh recently committed to raising government investments in health to 2.5 percent of GDP by 2017, which will really help extend health services to more people and will pay big economic dividends in the long term.
During my recent India trip, I was very glad to see the evolution and strengthening of our partnerships with government. I spoke with many government leaders including the dynamic chief ministers of two states, Bihar and Uttar Pradesh, which are among the poorest in the country. I was very impressed with the forward strides they’re making. The chief minister of Uttar Pradesh, Akhilesh Yadav, is under 40, the state’s youngest chief minister ever.
In Bihar, chief minister Nitish Kumar has helped drive remarkable improvements in farm productivity and is taking steps toward big improvements in health. Bihar’s maternal mortality rate is among the highest in India. But good things are happening. Last year our foundation launched a five-year, $80-million USD grant made in partnership with the state government and leading Indian and international non-government organizations. Bihar is becoming one of the nation’s biggest success stories.
As in Bihar, one important reason we invest in India is that we’ve found the government can be a very effective partner. Our government partners there are especially good at scaling up the very best ideas and sustaining them over the long term, as they’ve done with polio and now with HIV/AIDS.
This pattern has been repeated across the country over the past several decades. And as a result, aid has steadily become a smaller and smaller portion of the national economy. This is the good that can happen when aid donors and governments work hand in hand.
The People I Met
My trip to India
When I visit India, I speak with many people to learn about the country.

India is a fascinating country and I always learn so much from the people I meet. Sometimes it’s a challenge to reconcile the extremes. On the one hand, there are a lot of talented people and some amazing things going on there. But there’s also a huge amount of abject poverty in places like the Ujariaon slum in the state of Uttar Pradesh. People live in makeshift homes and face a lot of health problems. Yet, when I got a chance to talk with them, they’re like people everywhere. The people living in the slums want their kids to get educated and they are optimistic that things are going to get better. It was touching to hear their stories.
Reasons to Visit
Why India?
In this visit, I was interested to learn about India's progress in health.

I’ll soon be posting a full video about my recent trip to India. But first, a preview video and some thoughts about why I went. I go to India at least once a year to see the progress of the work our foundation is doing there. India is a fascinating, dynamic country, and I always learn so much from the people I meet.
We’ve been working in India for a long time, investing more than $1 billion in programs to fight disease and poverty. Originally we were focused mostly on preventing the spread of HIV/AIDS. That effort has become a great model for how to really scale up HIV/AIDS prevention, and it’s now transitioning to government sponsorship. This year’s trip was a chance for me to thank and congratulate everyone involved in the transition and in India’s progress against HIV/AIDS.
The trip also was a chance to celebrate the fact that India has now gone more than a year without recording a new case of polio. I also wanted to learn more about India’s progress as a developer and manufacturer of vaccines and other medicines that can help improve public health throughout the developing world.
Those are just some of the reasons why I went to India. The video on this page explains more, and I’ll share a lot more in the video that will be posted later this week.
Wash Your Hands
Can a simple, safe childbirth checklist save lives in developing countries?
I had the privilege recently of meeting Atul Gawande, a brilliant physician who’s using an amazingly simple concept—checklists for medical practitioners—to save lives and reduce health care costs. With support from our foundation, Gawande is investigating whether a safe childbirth checklist can increase the survival rate of mothers and newborns during childbirth in India and other developing countries.


It’s a well-known fact that hand washing and sterile instruments prevent the transmission of germs during medical procedures. Yet, many doctors and nurses frequently don’t follow these basic protocols.
It’s an especially big problem in developing countries—where many hospitals and clinics lack a basic standard of care.

Dr. Atul Gawande, a high-regarded U.S. surgeon and researcher, may have found the solution: a 1-page checklist that helps health workers avoid the major causes of maternal, newborn, and intrapartum (stillborn) deaths. Although it seems like a simple and obvious approach, no one has ever created a safe childbirth checklist. And until Gawande showed a few years ago that a simple checklist could save lives and avoid complications during surgery, there was no common checklist for that either. His work on developing and implementing checklists has had a dramatic impact on health care in the U.S. and around the world. Could we extend that insight to the developing world for childbirth?
I was a bit skeptical when I first heard about the power of a simple checklist. It sounded almost too good to be true. But Gawande’s research team tested the checklist idea with 8,000 patients undergoing surgery in eight cities around the world. On average, the checklist resulted in a 47% reduction in deaths and a 35% reduction in other complications.

At a time when most things about healthcare are getting more complex and costly, Gawande’s checklist is simplifying healthcare and saving money and lives. And the great thing is that it’s proving to be scalable without adding additional expense—a rare achievement in healthcare. So far, 4,000 hospitals worldwide are using the checklist approach to reduce errors during surgery.
In India, the safe childbirth checklist that Gawande’s research team developed in consultation with the World Health Organization is showing promising results. At the start of a pilot study at one childbirth center, health workers used only about one-third of the practices on the checklist—things like washing their hands before a vaginal exam, using a sterile blade to cut the umbilical cord, and introducing breastfeeding within an hour of birth. After the checklist was introduced—and with the coaching and guidance of the hospital administrator—compliance with best practices checklist shot up to 86%.

Our foundation is now funding a more extensive trial to see if the checklist can be scaled effectively to increase maternal and newborn survival in 120 hospitals in the Indian state of Uttar Pradesh. We focused on Uttar Pradesh because it is one of the poorest states in India. The mortality rate there for women giving birth is more than twice the rate elsewhere in India and over 30 times greater than in the U.S. So the potential impact in terms of saving lives is huge. And if the results are as positive as we hope, the childbirth checklist could be introduced in other developing countries.

One of the things that excites me about the checklist approach is that it focuses on improving health care by empowering the people working in local hospitals and clinics. And it doesn’t cost a lot of money. Getting the checklist right is critical, and not as easy as you might think. But once that’s done, Gawande’s approach is to train a handful of doctors or administrators and encourages them to coach their colleagues. We know that this kind of peer-to-peer coaching works well in other professions, such as teaching.
I first came across Gawande when I read one of his articles in The New Yorker, where he’s a staff writer (in addition to being a practicing surgeon, associate professor at Harvard, researcher, and book author). Gawande writes about his profession—and about his own experiences as a doctor—with an honesty and authenticity that is both refreshing and eye-opening.
I had the opportunity to meet him recently and he’s an impressive guy—one of a handful of people who’s really thinking creatively about how to improve the quality of health care and get costs under control. I’m optimistic there are other simple solutions that can similarly increase the quality of health care and lower costs at the same time. And if we can show their effectiveness in health care, we may discover they can be applied in other fields—such as education—where we also need to improve quality and make the most of limited resources.
Reaching High-Risk Groups
Avahan: Winning Against HIV/AIDS in India
One reason I was very excited to be visiting India recently was to get a chance to check on our foundation’s efforts to support the work of the government of India to halt the spread of HIV/AIDS. India is making good progress and learning lessons that could be helpful in other countries.

In 2003, we worked with Indian partners to launch a project called Avahan, which means “call to action” in Sanskrit, an ancient language of India. The project is a partnership with many Indian NGOs, state and local governments and the national government, which has increased funding for HIV/AIDS and established a national strategic plan that includes community-led HIV prevention.
Avahan’s efforts have been focused on reaching high-risk groups in six states of southern India, where the virus is most prevalent, and elsewhere along the nation’s major trucking routes, long-haul truckers being among those at high risk. Others we’re trying to reach include sex workers, their clients and partners, men who have sex with male partners, and injection drug users.
About 2.7 million people in India are infected with HIV, but that number is far below the dire forecasts that some experts predicted for India a decade ago. Avahan and India’s other efforts have contributed to a 50-percent reduction in HIV/AIDS incidence in the past six years, saving $100 million USD in averted health costs and, more importantly, saving many lives. One estimate puts the number of infections averted in the six states at more than 100,000.
Avahan is engaged in communities and at the street level, helping local groups deploy peer-to-peer counselors, distribute condoms and provide HIV testing, treatment and care. A big part of the effort is aimed at reducing the stigma that often prevents people from seeking HIV prevention and treatment services.
India has taken ownership of its national response to HIV/AIDS and is transitioning the Avahan program to state governments, facilitated by India’s National AIDS Control Programme. During my recent trip to India I was pleased to congratulate in person a number of the leaders who has been involved in transitioning Avahan and sustaining India’s HIV/AIDS prevention efforts.
In Bangalore, I got to spend time at a community center that’s part of Avahan. The center, known as Swathi’s Women's Group, was set up by sex workers to help prevent the spread of AIDS in their community. It’s been quite successful at that, and now it does lots more, like running a micro-finance bank and helping members defend their rights. It’s a great self-help success story.
The India program stands out as one of the best examples of effective national scale up of HIV prevention efforts, but those efforts will need sustained funding and government leadership. We’re hoping that what we learn in India will encourage and guide increased prevention efforts in other parts of the world.
In Bangalore
India: day three
My third day in India started with a visit to a community center that’s doing great work helping reduce HIV and providing support to sex workers. The day concluded with a meeting with a number of business leaders and philanthropists to talk about giving.

I started my last day in India at a Bangalore community center called Swathi’s House—a drop-in center for sex workers that’s part of a foundation-supported HIV prevention project called Avahan. The community members gave me a traditional Indian welcome, called an aarti. It was a day to celebrate, because the program is being handed off to the government for long-term support. But the real driver of success are the members themselves.
The center is run by a remarkable community-based organization called Swathi Mahila Sangha, which has approximately 8,500 members out of a population of about 19,000 sex workers in Bangalore. They provide counseling, medical help, HIV prevention training and a micro-finance bank. All of this is done with a cadre of peer educators and outreach workers. It’s a great model for self-help and empowerment.
I was touched by the community’s honesty and resolve—and their entrepreneurial spirit. Roughly half of the members now have savings accounts and their micro-finance bank has $800,000 USD in assets, with a recovery rate of nearly 100%. (I think most U.S. banks would be envious.) Thanks, in part, to their efforts, rates of HIV and sexually-transmitted diseases are down and the woman I talked with spoke of no longer feeling alone and helpless. They were proud of being able to keep their money, instead of remaining victims to “the thugs and the goons.”
Even though they are still a marginalized group, the sex workers are succeeding in advocating for their own rights and are enthusiastic about getting even more sex workers signed up and involved. There’s also been tremendous progress at the government level tackling the problem of HIV infection head-on, and Avahan and community centers like Swathi House are great examples.
I spent the last part of my trip at a gathering of a number of business leaders and philanthropists. I was the guest of two remarkable individuals. Azim Premji is the founder of Wipro and one of Asia’s biggest philanthropists. Ratan Tata is one of the country’s foremost business leaders and a member of the Tata family well known throughout Indian industry and philanthropy. They were nice enough to invite me to make a few remarks at the beginning, but mostly it was an opportunity to listen and learn about their perspectives on philanthropy in India.
While the circumstances for giving are unique in India, it was amazing just how much their discussion sounded like the conversations I’ve had with wealthy business people and philanthropists in the U.S. and elsewhere. A few common themes emerged. People agreed it was often easier to make the money than to give it away in a thoughtful way. There was a huge feeling of personal satisfaction in their philanthropic work, and a deep sense of societal obligation to give back. With so many problems to address, deciding where to engage and how to do it weighs heavily on their minds.
The group decided they wanted to get together again to learn from one another and talk through issues of common interest. That was fantastic. India is in a new phase of its long history of charitable giving, and I am certain many of these families are going to lead the way by doing remarkable things.
It’s been a very productive and moving three days. I’m grateful I had the chance to meet with so many amazing people in a short time. I’ll post some thoughts on the trip as a whole as well as some video the week of June 11. There’s a lot to reflect on.
Life in Lucknow
Day one in India, May 2012
I’m in India this week, and my first stop is in the state of Uttar Pradesh (U.P.). In U.P.’s capital, Lucknow, I’m meeting with people from just about the two most opposite ends of the social spectrum.

I’m seeing U.P.’s new Chief Minister, who would be the head of state of the world’s fifth largest country if U.P, with its 200 million inhabitants, was its own nation. But I started out the day in the Ujariaon slums.

I just finished Behind the Beautiful Forevers, Katherine Boo’s book on the slums of Mumbai, and so was thinking about this part of the trip before I got here. I’ve been to poor areas many times, but I don’t think anything can completely prepare you for a place like Ujariaon.

About 2,000 people live here in an area of about a square kilometer. What little work there is around here is almost all done by garbage pickers, who leave every morning quite early to roam around the city to find things that they could possibly sell or use. As you see in these photos, there are mountains of soda bottles and cardboard. And in the middle of the garbage, families are making whatever makeshift shelters they can.

During the day, there are lots of young kids around who aren’t old enough to be of much use picking garbage. They were awfully curious about who all these visitors were.

I sat down with some community health outreach workers and some women who are raising their families in the Ujarianon slums to hear about the Urban Health Initiative. The UHI is working in 11 cities to expand access to family planning services. Reaching women who live in circumstances like this is extremely difficult. But the outreach workers are dedicated to helping local women understand what options they have and getting them access to contraceptives if they wish them.

It was touching to listen to the women talk about their hopes for their families, and to hear them explain why having fewer children could mean a better life for their kids. The circumstances are horrendous, but their determined hope for their children is beautiful.
The challenges of helping communities like this could be overwhelming. That is why I was so encouraged to meet Chief Minister Akhilesh Yadav and many of his staff and ministers. He is young – only 38 years old -- and something of a rising star in Indian politics.
I came away with a very real sense that he and his colleagues in U.P. are truly committed to a number of critically important initiatives, particularly around health care for the poor, vaccines and development. There are new efforts around universal vaccination, which will have a huge impact on U.P. They’re also addressing critical needs in water, sanitation and hygiene. My visit to the slum earlier in the day, where good water is rare and open defecation is the rule, was a stark reminder that even in the cities, there is much work to be done.
We had a very productive exchange with Chief Minister Yadav as we talked about the projects we’re working on in U.P. His energy and optimism for changing life for the better in U.P. was encouraging. While the Chief Minister and the mothers I spoke to earlier in the day live in very different conditions, they share a deep desire to make things better in U.P. – for their families, and for the state as a whole. I don’t know that you can understand things like this very well without going to see, and I felt lucky to be in India on day one.
Tomorrow, it’s Delhi and the chance to talk about polio with some important guests.
Vaccines and Mangoes
India: day two
My second full-day in India started with a meeting with a high-level delegation from Pakistan of people working on eradicating polio in their country. It was tremendously kind of them to come to Delhi to see me. We had a lot to discuss.

The delegation was led by Shannaz Wazir Ali, who is Prime Minister Syed Yousaf Raza Gillani’s Special Assistant for polio eradication. I’d met her early last year in Dubai, to talk about ridding Pakistan of this terrible disease, and so it was good to catch up on progress made in the intervening months.Accompanying her were a group of public health officials and, most importantly, leaders from many of the provincial governments who are on the ground working toward this tough but important goal.
That this meeting happened in India is significant for several reasons. But the fact that India has been without a case of polio for over a year now is a terrific achievement. Besides meeting with me, the group will also spend time with Indian public health officials, sharing best practices and learning from one another. The conditions in Pakistan are really difficult, but you could not hope to find a more committed group of people than the delegation I met with. Many of the public health workers fighting to end polio in Pakistan risk their lives doing so. These are true heroes who face incredible obstacles -- misperceptions about the vaccines, remote and migrant communities, the need to go into villages that are dangerous because of violence and political instability.
But if India could beat polio (at least so far) in places like Uttar Pradesh and Bihar, I know Pakistan can do the same for its people. There are 16 cases reported in Pakistan so far this year. While that’s not a big number, it represents a huge vaccination challenge. I don’t wish to underplay the challenge, but seeing the Pakistani delegation’s resolve and desire to make polio eradication a national priority encouraged me.
Later in the day I visited the Serum Institute of India. This is an amazing company, and its facilities would be considered state of the art anywhere in the world. Serum produces low-cost, high-quality vaccines used in 140 countries around the world. It started out in 1966 to manufacture low-cost vaccines for Indian use. But over the years, Serum’s low-cost vaccines have literally transformed the world of health. By lowering the cost, you expand the reach of these miracle drugs. So I was really honored to be welcomed by Dr. Cyrus Poonawalla, who started Serum with his brother, and whose commitment to low-cost access has made a huge difference to millions of people around the world. This year, Serum will ship a billion doses of vaccines worldwide.
I was able to meet with a number of Serum’s top scientists and got to look at their impressive manufacturing line. I was particularly happy to see their work on the Pentavalent vaccines. This is a 5-in-1 vaccine given to children to protect them from life-threatening haemophilus influenza type B, diphtheria, pertussis, tetanus and hepatitis B. Serum’s work has dramatically lowered the cost of these vaccines (and a great many others) and is a true contribution by India to the well-being of the world.
A couple of commenters have asked about the weather, and I’ll admit – as a guy from Seattle – that the temperatures have been a challenge (44 Celsius – 112 Fahrenheit today). The upside is that it’s the height of the mango season right now, and I’ve been lucky enough to get them at just about every meal. They’re spectacular.
I finish up in Bangalore on Friday where I’ll once again be spending time with two distant ends of the spectrum. In the morning, a meeting with sex workers involved in an HIV prevention program called Avahan and I’ll end the day listening to some of India’s wealthiest families about their thoughts on philanthropy.
Real Courage
Zambia: On the front lines waging war against HIV and Malaria
The hints of progress I saw at an HIV clinic in Zambia.

The AIDS epidemic in Zambia is a sobering reminder of the big health challenges many African countries face. However, we are beginning to see encouraging signs of progress.
The government of Zambia and non-profit health clinics like the Coptic Mission Hospital that I visited in Lusaka are doing great work treating HIV patients. I wish more people could have an opportunity to meet people like Florence Daka, a mother of four who is alive today in Zambia because of the effectiveness of HIV drugs. Florence’s story is even more compelling because the drugs she takes also prevented transmission of HIV to her newborn son. The spread of HIV from mother-to-child is one of the most frequent ways AIDS has spread in Zambia—where more than 15% of the adult population is living with the disease but many do not know it.
Even more encouraging, I talked with men who are courageously setting aside cultural views and getting circumcised because they understand it significantly reduces their risk of getting or transmitting AIDS. The goal with AIDS is to have a vaccine that will prevent anyone from getting the disease. But we're more than a decade away from having that. So one of the best tools we have right now, other than behavior change, is male circumcision.
One of the important things we’ve learned about the spread of AIDS is that it occurs less often in communities where men have been circumcised for cultural or religious reasons. But the big question was whether you could convince a large percentage of adult men who weren’t circumcised as infants to come in for the procedure. An important breakthrough was the invention of a small device called a Shang Ring. It is considered safer than the standard surgical procedure, costs less, and is acceptable to men. This is great news because it enables health officials to scale up the procedure.
Many countries in Africa are launching national programs to encourage circumcision. In Zambia, the government has set a target of circumcising 80 percent of the male population—nearly 2 million men. Kenya, South Africa, Botswana, and Tanzania are also starting to show leadership in this area.
I was also heartened to see the progress in Zambia against malaria, which like AIDS is a devastating disease that disproportionately affects the poor. Fifty years ago, the only way to slow malaria was to spray DDT—a highly toxic chemical—on walls. But in recent years, countries like Zambia have launched an intensive effort to distribute mosquito bed nets, medicines, diagnostics and insecticides that have dramatically reduced the number of young children dying from the disease.
Zambia was one of the first countries to pilot widespread distribution of bed nets and the foundation has been a funder of that effort. Zambia’s program is so well run and effective that the government hopes to eliminate malaria in five regions by 2015 and completely eliminate it throughout the country by 2030. That kind of goal would have been unimaginable even a decade ago.
Combined with the successes I saw in Ethiopia providing basic health services for women and children and boosting agricultural productivity for small farmers, there are a many reasons to be optimistic that many people in Africa are on the road to self-sufficiency. One of the jobs of our foundation is to make sure other donor countries and governments understand the important progress being made—progress that is really changing the quality of life for millions of people in Africa.
Modeling Progress
Ethiopia: exciting innovations in agriculture and health
In Ethiopia, I saw advancements in farming and health services.

Ethiopia is one of the poorest countries in the world and has faced enormous challenges feeding its people and providing critical health services to mothers and their children. Yet, I returned from a recent visit excited about advances the country is making in agriculture and health.
If these innovations—which are a top priority for our foundation—succeed, they can be replicated in other African countries that also face big challenges in health and agriculture.
One factor in Ethiopia’s progress is Prime Minister Meles Zenawi and his leadership team, who have played a key role in reinventing the country’s agricultural and health systems. Making changes to either would be a big challenge in any country, so it’s even more impressive in Ethiopia, which has the second largest population of any country in Africa but a limited economic infrastructure.
Around 85 percent of the country’s population survives by growing crops on small plots of less than five acres. But frequent droughts and soils that have been depleted of nutrients often led to low crop yields and considerable food insecurity. More than half of the country’s population of 83 million is malnourished and more than 5 million households receive food aid each year.
Our foundation has been working with the Ministry of Agriculture, the county’s new Agricultural Transformation Agency, and other partners to help farmers plant higher-yielding, drought-tolerant seeds, improve soil health and fertility, and get higher prices for their crops by selling to global markets.
At the Melkassa Research Station, one of 13 government-run agricultural outposts, Dr. Markus Walsh, Sr. showed me a new, state-of-the-art technology called NIR spectroscopy that’s part of a digital revolution in agriculture. This portable device, which quickly and cheaply analyzes soil conditions, is a fantastic breakthrough that will help farmers everywhere. But it’s especially valuable in countries like Ethiopia, where farmers haven’t been able to afford laboratory tests but need to know how to amend soils to grow better crops. The spectroscopy is part of an even bigger agricultural digital information system that will provide a comprehensive and detailed map of soil properties across the country.
I also met with a number of farmers to talk about new varieties of sorghum (a grain) and beans they are growing. Beans are very important because they provide protein and people need a combination of protein and grain to have a reasonable diet.
Helping small farmers sell their crops in world markets is another important part of the work we’re supporting in Ethiopia. It’s currently a big challenge because poor farmers may not be growing the right crops for world markets and they often lack the roads, trucks, and other infrastructure necessary to enable exports. And getting foreign investors to help build this “value chain” can be difficult. But I visited one agricultural processing facility called ACOS, that is processing and shipping a variety of beans to European markets. It is jointly owned by an Italian company and Ethiopian investors and is a great example of private investment in developing countries.
What Ethiopia is doing in health is really a model system because it reaches everyone in the country. I visited the Germana Gale Health Post, where I talked to several of the more than 30,000 health extension workers who have been trained in recent years to deliver basic health education, prevention, and treatment. Most of the health workers are women, and those I met were energetic and well-trained.
These kinds of primary health services—giving vaccines, educating women about family health, and promoting hygiene and environmental sanitation—is the foundation for building good health systems in poor countries. Ethiopia’s health system also includes district health centers like the Dalocha Health Center I visited. There, they do a little bit of surgery and have more expertise and a wider variety of drugs. There are also primary hospitals that focus on higher level treatment and some emergency surgery, and general hospitals that deal with serious emergencies and high-risk and specialized care.
Ethiopia still faces some big problems. But the people I met and what I saw re-energized me and increased my optimism that the big investments we and other donors are making in health and agriculture will pay off for the people of Ethiopia and can serve as model activities in other African countries. Improving agricultural productivity and the quality of life through better health services is the key to unleashing the potential of Ethiopia and other poor countries and getting them on the road to self-sufficiency.
Science, Soil, and Seeds
Agriculture in Ethiopia
Most of the world’s poorest people are farmers, and so helping them improve their lives involves expertise in soil science, seed hybridization, and agricultural marketing. All of which are being used to end hunger and raise living standards in Ethiopia, as I observed during my recent visit.

Africa’s farmers get their food and income from farming small plots of land. They grow a variety of crops, which are often threatened by diseases, pests and drought.
One of the biggest challenges farmers face is unproductive soil. For Ethiopia, the Africa Soil Information Service is generating a digital soil map to diagnose local conditions and make targeted recommendations for improved crop production.
Soil samples are collected and analyzed using near-infrared spectroscopy, which is both portable and less expensive than traditional wet chemistry analysis. Samples are analyzed against a library of 500,000 entries.
The Ethiopian Institute of Agriculture Research has 13 stations that support technology development for sorghum, maize, common beans, and horticulture crops (onion, tomato, fruits). Bill visited the Melkassa Research Station in Nazaret, Ethiopia.
One of Ethiopia’s main crops is sorghum. It grows well in harsh conditions and is self-pollinating. There are many varieties, used for food and brewing.
Sorghum breeder Alemu Tirfessa shows Bill the diverse breeds, and describes hybrid seed production. The new hybrid seeds are more resistant to disease and drought.
The many varieties of beans grown in Ethiopia are grouped by market classes. Beans are a very important crop because they provide protein, which helps create a balanced diet when paired with grain.
Bill spoke with representatives from the Lume Adama Farmers’ Cooperative, which helps farmers set pricing, get credit, and gain access to improved seed. One farmer said that thanks to increased chickpea production, she’s doubled the number of oxen she owns and has earned enough money to send her four children to school.
In the Bowls of Millions
Ethiopia & sorghum
During my recent visit to Ethiopia, I learned about the nation’s ambitious efforts to fight poverty by increasing farm productivity. Those efforts are focused in part on a cereal crop that is almost unknown in the developed world, but that is a major lifeline for much of Africa and Asia.

Sorghum is the world’s fifth most important cereal in terms of the land used to grow it and the volume produced.
Sorghum is an especially important crop and diet staple in poor countries.
Other grains are unsuitable in areas that get little rainfall, that are subject to drought or where irrigation is not possible. That’s where sorghum is a lifesaver.
Sorghum is widely grown both for food and as a feed grain.
On my recent trip to Ethiopia, I learned about efforts to help poor farmers improve their crop yields. I got to attend a sorghum demonstration at the Melkassa Agricultural Research Station.
In Africa’s poorest regions, people still grind sorghum and other cereals by hand, much as their ancestors did.
Here a girl shakes a tray of sorghum to prepare it for use in making Injera, a sort of pancake. Consumed in many ways, sorghum and millets are a major source of calories and protein for millions of people in Africa and Asia.
Malting and brewing sorghum produce lager and stout, often referred to as clear beer, as opposed to traditional African opaque beer. Clear beer has been brewed commercially in Africa since the late 1980s.
Keeping the Pests Out
A simple advance in crop storage aids poor farmers in Africa
Reducing spoilage from weevils helps farmers store and sell more crops.

On a recent trip to Africa, I saw the incredible impact that simple innovations can have on the world’s poor. For years, farmers trying to eke out a living growing cowpeas—a protein-rich staple—would lose as much as half their crop to weevils. As I showed students during a recent talk at Stanford, a simple, inexpensive triple-layer bag invented by researchers at Purdue University enables farmers to protect their entire crop. This allows farmers to charge more for their crops and has increased their incomes by as much as 30 percent.
The People I Met
Photos from my trip to Ethiopia and Zambia
On my recent trip to Ethiopia and Zambia, I met with health workers, families, and farmers, and learned about the progress they are making in meeting healthcare and agricultural challenges.

On my recent trip to Ethiopia and Zambia, I met with health workers, families, and farmers, and learned about the progress they are making in meeting healthcare and agricultural challenges.
I visited the Germana Gale Health Post Site in Silte, Ethiopia, to meet with health extension workers and learn about the critical health issues they see, such as maternal and neonatal health risks, malaria, and pneumonia.
This health post offers several services, and also provides training to residents and community leaders to help spread information and educate the community at large about health issues and available treatments.
The health worker at this post is very active and experienced, providing family health services, and distributing supplies such as bed nets for malaria prevention.
This year, she has seen more than 200 children, most ages 2 weeks and older. On a tour of the delivery room, she explained that she is usually called to homes by family members for births.
She provides family planning services and counseling to new mothers, focusing on the importance of breastfeeding for the babies' health.
A large number of "family folders", individual family medical records, are kept at the health post. There are also many wall charts showing dates and numbers of services.
Each wall chart indicates annual and quarterly targets for each service (immunization, deliveries, preventive treatments).
I asked how closely they were meeting their targets, and learned how they captured the data.
The storage for vaccines includes a broken kerosene refrigerator and a cold box. The refrigerator broke after two years and has not been fixed.
Vaccine is delivered in a small cold box from the health center on the days they provide services.
An immunization clinic was being held on the porch of a side building, where a group of women were receiving tetanus vaccines and children were receiving Penta, polio, measles and PCV.
While most services are given at the health center, the health worker has two outreaches per month, the furthest being a three-hour walk away.
The clinic had a coffee ceremony for me, roasting the beans on the spot.
Coffee was served with popcorn.
I visited a household with a two week-old baby. The home was fairly large, with a fenced-off area for animals. The family has two other children – a 3 year-old and a 6 year-old.
The baby and the older children were all born at home with the help of the health worker, who taught their mother to begin breastfeeding immediately to help boost the baby's immune system with colostrum.
I visited the Melkassa Research Station in Nazaret, Ethiopia, one of 13 stations in the Ethiopian Institute of Agriculture Research that supports technology development for sorghum, maize, common bean and horticulture crops (onion, tomato, fruits).
Farmers are facing challenges in seed production with the current irrigation capacity. To address this, experimental hybrids are being formed under the Drought Tolerant Maize for Africa project.
In the last eight years, the agriculture sector in Ethiopia has been growing at the rate of 10 percent per year. The country also has a comprehensive food security program for drought-prone areas.
Currently, most farmers rely on seed they have saved themselves, which is subject to drought and losses caused by birds. Seed companies can produce hybrid seed, providing the best option increasing production of sorghum.
Workers sort and clean seed at a seed-processing facility.
At the legume seed storage facility, I saw the different market classes of beans (white pea, red kidney, small red, sugar, large kidney beans) as well as chickpea (desi and kabuli), and mungbean.
I visited the cold storage, which plays a critical role in preserving seed viability for legumes. They lose viability faster than cereals because of their high protein content.
Male circumcision can significantly reduce HIV transmission. At the Shang Ring Male Circumcision clinic, they are conducting a trial program where circumcision can be performed at a cost as low as $2 per device.
The Coptic Mission Hospital and Clinic in Lusaka, Zambia, has been a high-quality provider of HIV services.
I met Florence Daka, a cleaner at the hospital, who tested positive for HIV in 2008 and was successfully treated with an antiretroviral (ARV) drug. In 2010, Florence was able to conceive, and safely deliver an HIV-negative child, Stephen.
Some Pictures
Photos from my recent trip to Ethiopia and Zambia
On my recent trip to Africa, I met with many people and heard their interesting, inspiring stories about how aid works. This gallery has stories and photos from the trip.

On my recent trip to Africa, I met with many people and heard their interesting, inspiring stories about how aid works. This gallery is a preview of some of the stories and photos I'll share during a Livestream on April 4th.
In Silte, Ethiopia, we visited one of the nation’s many new “health posts” set up to improve public health, village by village. The staff members here are saving lives with their incredible work.

Bed nets are still one of our best tools against malaria. While in Zambia, we met with local health care officials to talk about their battle against the disease.

Africa is making significant progress toward the Millennium Development Goals of improving maternal and child health.

AIDS/HIV has taken a huge toll in Africa, but more people are getting the life-saving treatments they need, while education and outreach efforts are curbing the rate of new infections.
African farmers of cowpeas (also known as black-eyes peas) are benefitting from an inexpensive solution to weevil infestations that used to ravage their crops after harvest. Scientists from Purdue University developed airtight bags to protect cowpeas.

Now, farmers can store cowpeas for sale when prices are strong. That’s expected to raise farmers’ annual incomes by an average of $150 in West and Central Africa, where most live on about $2 per day.

A Good Effort
A report card on helping the world’s poor
I believe the global community deserves a solid B for progress meeting the UN’s Millennium Development Goals.

People sometimes say that the United Nations doesn’t do enough to solve the big problems of the world. I’ve never really agreed with that point of view, but if anyone is looking for evidence of the UN’s impact, a good place to start is the Millennium Development Goals (MDGs).
The MDGs are an ambitious set of goals for reducing poverty and child mortality rates, and fighting diseases that sap the socioeconomic potential of poor countries. They were agreed to in 2000 by all 193 UN member countries and 23 international organizations. Creating that kind of consensus is—by itself—a significant achievement.
The great thing about the MDGs is that they provide clear targets and indicators of progress in key areas, including ending poverty and hunger, ensuring universal education, gender equality, improving child and maternal health, combatting HIV/AIDS, environmental sustainability, and strengthening global development.
Although a number of countries won’t be able to achieve all of the goals by the target date of 2015, the MDGs have been helpful in getting everyone to really think about their part, the progress they’re making, and what they can learn from others. The goals have focused political attention in developing countries, encouraged UN groups to work together, and inspired wealthy and fast-growing donor countries to coordinate their efforts.
In February, the World Bank announced that the MDG goal of cutting extreme poverty by half had been achieved five years early. A week later, UNICEF and the World Health Organization announced that the goal of halving the number of people without access to safer drinking water was also reached five years early. These are noteworthy achievements though much work remains to be done. Other goals, such as reducing maternal mortality by three-quarters, simply won't be achievable by 2015, although the progress has been really good.
Already, people are talking about what the goals should be for 2030. That’s a great thing because there’s still a lot more work to do, especially in reducing diseases and maternal and childhood deaths. But I believe the global community deserves a solid B for its efforts so far and where there is progress, we should celebrate.
One of the things I’ve learned in my work at Microsoft and the foundation is that setting clear goals and honestly evaluating progress is critical when trying to tackle big challenges. The MDGs provide a report card on the progress the world is making to take care of those most in need.
Goal 1: Eradicate Extreme Poverty and Hunger
Goal 2: Achieve Universal Primary Education
Goal 3: Promote Gender Equality and Empower Women
Goal 4: Reduce Child Mortality
Goal 5: Improve Maternal Health
Goal 6: Combat HIV/AIDS, Malaria and Other Diseases
Goal 7: Ensure Environmental Sustainability
Goal 8: Develop a Global Partnership for Development
Beans
On my way to Africa
On my trip to Africa, I'm thinking about malaria, public health systems, farm productivity, and beans. Yes, beans.

This week I’m in Africa, a place I go a couple of times a year to see our foundation’s work in the field. The reason I go on these trips is to see for myself what’s happening and I come away with success stories, notes on things that we need to get smarter about, and a better understanding overall. This time I’m visiting Ethiopia and Zambia, which should be very interesting.
Eliminating malaria in Zambia
I’ll be looking at malaria intervention in Zambia, because that’s where we supported the first major efforts to distribute bed nets and get people to use them. After we began this work, the U.S. started the President's Malaria Initiative, which essentially expanded what we were doing in Zambia and replicated the program in other countries.
Malaria deaths are way down from their peak in Zambia. Bed nets have been very effective. But we’re still looking for answers to some questions about them. How much do they help long term? How quickly do they wear out? Despite them, do malaria deaths eventually rebound, as we’ve seen somewhat in Zambia (particularly in the north)? Why the increase - is it because people didn’t use the nets, because they’re torn, because mosquitoes adapted, or simply because mosquito numbers vary from year to year?
Nobody ever thought bed nets alone would drive malaria to zero. They’re a really good tool, but you'll need a couple other tools that you use in a deep way to ever get to eliminating malaria in a particular location or community. Everything we’re learning is equipping us to achieve our long-term goal, which is to eliminate malaria locally in a whole lot of communities, building to eventually emptying the malaria map.
New kind of government partnership in Ethiopia
We’ve been working in Ethiopia for more than a decade. In that time we’ve made over 125 grants to partner organizations that are doing health and development projects there. Our engagement deepened a few years ago when Prime Minister Melas Zenawi came to us and said he really wanted to improve agricultural productivity. Agriculture contributes about half of Ethiopia’s GDP and employs roughly 80 percent of the workforce.
But the Prime Minister said he wanted to try something different from the normal way donors come in and support particular projects. He wanted to step back and look at everything involved in farm yields – seed companies, farmer education, fertilizer costs, everything – and then figure out an overall plan. And then ask donors to support things that fit with the plan. So, about a year and a half ago, Ethiopia formed the Agricultural Transformation Agency.
This is exciting, because areas in the Horn of Africa are often on the edge of famine. The situation in Ethiopia is nowhere near as bad as in Somalia, but the eastern part of Ethiopia has had recurring food problems. Improving the amount of food farmers can raise would make a big difference in the lives of those families living there.
Now that ATA has new policies in place, donor money is going to support projects in line with an overall plan. A lot of the focus is on increasing the productivity of small farmers. Part of the plan involves using new types of seeds. I’ll get to see how that’s going.
Community health outreach
I’ll also get to see the results from Ethiopia really bulking up its community health outreach. About 20,000 young women have been trained and placed in newly built health posts, as they’re called. I’ll be interested to see how that’s going and what the challenges are. One surprise is that pregnant women aren’t coming into the health posts to deliver their babies, at least not as much as expected. What would it take to change that, since the health of the mother and the baby are so dramatically improved by delivering in a clinic? I’m also interested in getting a clearer idea of Ethiopia’s vaccination rates. There are conflicting data on that.
Legumes – beans, basically
I'm also visiting an agricultural research station in Ethiopia where they’re doing very interesting work with legumes – beans, basically. The project is developing new varieties and helping farmers learn how to process them for sale to urban markets, which small farmers weren’t getting to before.
Beans are interesting because they’re a staple for really poor people almost everywhere. The most basic or world diets consist of some kind of bean and some kind of grain: beans and rice, beans and wheat, beans and millet. That combination gives you the complete proteins you need to live. So, nearly everywhere, subsistence farmers grow beans. They’re not only a staple, but also a fertilizer for farmers’ other crops, because beans return nitrogen back into the soil, which most every other crop takes out. Coming up with even better varieties could help farmers and improve nutrition in many places.
As always, throughout this trip I’ll be meeting with local representatives of donor groups and leaders of aid projects. We get together and they talk openly about what’s working and what’s not. That’s always very helpful, hearing from people in the field.
When I come back from Africa I plan to share some of the stories and photos of what I’ve seen in the field so that others can have a glimpse of what’s going on in the poorer part of the world. And by providing that glimpse, I hope it draws people in to want to know about and care about these issues.
Innovation on Small Plots
Working together for small farmers
I urged leaders of the international agriculture community that they need to do better for small farmers.

If you care about poor people, you need to care about agriculture.
Most extremely poor people in the developing world get their food and income from farming small plots of land. Many others live in big cities and need access to inexpensive food to be healthy and productive. So helping small farmers grow more food sustainably is the best way to fight hunger and poverty over the long term.
History is on our side. In the past several decades, agricultural yields in many places have doubled, and hunger and poverty have been cut in half. Now it is time to continue and accelerate that progress.
This week, I am speaking to the leaders of the international agriculture community at a meeting at the International Fund for Agricultural Development. The audience will be made up of the key people working in developing countries, aid agencies in developed countries, and international groups like the World Food Program and the Food and Agriculture Organization—and my message is that they need to do better for small farmers.
I am urging them to get together to set a common productivity target and create a system of public scorecards to hold themselves accountable. If they take these steps, I believe it is possible to meet the world’s most aggressive goals for reducing hunger and poverty.
One of the most important priorities is connecting the poorest farmers in the world to breakthroughs in agricultural science and technology. Right now, a digital revolution is changing the way farming is done, but poor small farmers aren’t benefitting from it.
For example, we now have satellites that can identify instantly and precisely how much wheat there is in a field. However, many developing countries are still sending people out with a pad, pencil, and tape measure to estimate yields. As a result, we take more time and expense to get less accurate and incomplete data. Better data, collected in a timely way, means decision makers have better information to make policies that can help farmers. That is one examples of how a digital revolution can make a difference.
Innovation is the concept on which Melinda and I created the foundation. For years, we saw the impact that innovation in the computer industry had on the richest people in the world. But at the same time, the poorest half was hardly benefitting from innovation at all. We hope our foundation can work with partners to help change that.
The stakes could not be higher. The world’s ability to help small farmers be more sustainably productive will determine whether or not they remain in poverty or whether the hard work results in self-sufficiency for hundreds of millions of people.
Swatting Mosquitoes
Using Disease to Fight Disease
A novel approach to controlling mosquito populations

Most people probably wouldn’t want to visit a mosquito research lab on their family vacation, but Melinda and I were in Australia recently and were excited to see some amazing work in molecular biology that could lead to a breakthrough in controlling mosquito-borne diseases such as dengue fever.
Mosquitoes are a plague in much of the developing world, not just because they are a nuisance, but because they are transmission agents for some truly terrible diseases. The scientists we met with in Cairns have discovered a way to infect mosquitoes that are normally capable of carrying diseases like dengue and yellow fever with a bacterium called Wolbachia. Wolbachia is naturally present in many types of insects, but not in these mosquitoes. Although it is harmless to humans and most other animals, when placed in these mosquitoes Wolbachia shortens their lifespan by about 50 percent and inhibits the development of dengue virus and several other pathogens.
If mosquitoes with the Wolbachia strain can be successfully introduced into wild mosquito populations, it could greatly reduce the transmission of infectious diseases to humans because most mosquitoes would die off before the viruses that cause human disease could replicate in their body. Another plus for Wolbachia is that it alters the mosquitoes’ reproductive biology, so that when female mosquitoes that do not carry Wolbachia mate with male mosquitoes that do carry Wolbachia nearly all of their embryos die off. Since Wolbachia is passed through the mother mosquito to her offspring, this means that Wolbachia can spread very rapidly through a mosquito population.
Some of these discoveries were a surprise to scientists. If they can be proven in field trials, Wolbachia could create a cheap, natural, and self-sustaining method of control that dramatically reduces dengue fever and other major infectious diseases such as yellow fever and malaria.
The research, led by Professor Scott O’Neill of Monash University, has been funded since 2005 by the Foundation for the National Institutes of Health (FNIH) under the Grand Challenges in Global Health initiative, which encourages innovation to solve persistent health problems in the developing world. Diseases spread by mosquitoes are definitely at the top of that list.
O’Neill’s work is mainly focused on preventing mosquitoes from transmitting the virus that causes dengue fever, an infectious tropical disease that causes 22,000 deaths—mostly among children—and results in 500,000 cases of severe illness each year. Scientists are optimistic that this approach could also work with other insect-transmitted diseases such as malaria, which kills nearly 1 million people annually, mostly children under 5 years of age.
Historically, the battle against disease-carrying mosquitoes has relied on repellants, insecticides, bed nets and eliminating stagnant water breeding sites. More recently, scientists have been working on vaccines that would prevent people from getting infected with mosquito-borne diseases.
To do his current research, O’Neill has had to convince people in Cairns that releasing mosquitoes in their neighborhoods is a good thing. Melinda and I participated in one release of about 20 jars of mosquitoes—probably 1,000 mosquitoes in all. I was bitten by several dozen, but was safe from getting dengue fever because the mosquitoes being released were lab-reared and not infected with dengue. I have a lot of respect for the volunteers who go into mosquito cages and allow themselves to be bit in the name of science. The average number of bites they get is over 50!
It was fascinating to see the project first-hand. There’s a real possibility that this approach will get deployed broadly and could really help reduce a lot of disease transmission. But as exciting as it was for Melinda and me, our kids said they definitely didn’t mind not going along.
A Bunch of Reasons
Building better bananas
I'm sometimes asked why the foundation has made agricultural development a priority along with global health. Actually, the two are intertwined. One example comes from Australia and Uganda, where researchers are using advanced technology to try to improve the banana.

Our foundation’s work around the world gives me opportunities to meet really smart, visionary people who are doing pioneering work in fields that I might not get a chance to learn much about otherwise. For example, in December Melinda and I went to Cairns, Australia, where James Dale and his team from Queensland University of Technology are doing advanced research on bananas. As odd as that might sound, this research could make a big contribution to public health in a lot of Africa and Asia.
Before our visit, I didn’t know much about bananas. Dale, an agricultural scientist, is one of the world’s leading experts. He has been profiled in The New Yorker, in a fascinating article about the history of bananas as an export crop. As the article explains, a blight has spread among plantations in Asia and Australia in recent years, badly damaging production of the one type of banana that is grown for export, the Cavendish. This disease, a fungus, hasn’t spread to Latin America yet, but if it does, bananas could get a lot scarcer and more expensive in North America and elsewhere. Dale is working to develop new versions of the Cavendish that resist the fungus. He does this by inserting genetic material from other organisms into banana plants.
This work is separate from the research that our foundation supports, although some of the same techniques and scientific principles are involved, including transgenic experiments. Making banana plants less susceptible to diseases is a secondary goal for us. Our primary goal is to help Dale develop new types of banana that are more nutritious—specifically, much richer in Vitamin A and Iron that the body can absorb.
This is important because the diets of millions of people in Africa are deficient in both of these vital nutrients. While rare in the developed world, Vitamin A deficiency in developing countries causes hundreds of thousands of children to go blind each year. It also reduces the body’s ability to fight infection, which raises the fatality rates in poor countries from infectious diseases like measles. Iron deficiency is so serious and widespread that in Uganda, for example, more than 40 percent of young children have stunted growth and 73 percent are anemic.
Meanwhile, bananas are a primary staple of people’s diet in Uganda and many other African nations. (Our foundation also has supported research to enhance the micronutrient content of cassava, rice and sorghum, all staples for millions of the world’s poorest people.) An average Ugandan consumes about five times his or her weight in bananas each year. Fortunately, Ugandans have more varieties of banana to choose from than we usually do in the developed world. Some varieties are eaten raw, while others are cooked as part of a dish with other ingredients. The kind that are cooked are sometimes called plantains, but they’re all bananas. For dessert there’s the sweet Sukali Ndizi, which children especially love.
Unfortunately, the banana varieties grown in Uganda are low in essential micronutrients, particularly Vitamin A and Iron. To increase these levels, Dale and his team in Australia are collaborating closely with Ugandan scientists at that country’s National Agricultural Research Organization. The NARO team, led by Dr. Wilberforce Tushemereirwe, has made important contributions—developing research protocols, conducting field trials, and planning distribution of new, more nutritious banana varieties to Ugandan farmers. The NARO team’s involvement is a great example of young African scientists playing a major role as full partners in using state-of-the-art science for development of new products important to agriculture and health in their own country.
Our foundation has supported this work since 2005, initially as part of our Grand Challenges in Global Health initiative, which fosters early-stage research aimed at breakthroughs on the world’s most pressing health problems. If you had asked me at the time, I would have said the project was one of the more wild things we funded. Some of the original Grand Challenges projects, even some of the ones I thought were the most likely to succeed, have come to an end, but that’s scientific discovery.
Other funders have not been focused on the kind of work that Dale and NARO are doing, so our funding has been important, and the work is progressing well. New banana varieties have been developed that have as much as five times more Vitamin A than before. You have to get the levels just right, though, because too much makes the banana look orange, which consumers might not like. Boosting iron levels seems to be a tougher challenge.
It all takes a long time, though, for a few reasons. Not much was known before about how to work with banana cultures at the molecular level, so a lot of basic science had to be done first. Then, it takes two or three years to take a new banana culture from inception to the point where it produces fruit and you can see if it’s more nutritious. And there have been some unfortunate setbacks. In early 2011, Cyclone Yasi roared through Cairns and destroyed the fruit crop from field trials there. Luckily, the cyclone did not uproot the plants, but the trials were delayed at least nine months until a new crop of bananas could grow.
Once some clearly superior banana varieties are developed and proven, it will take time to do the research to show the health benefits, for regulators to approve them, and for farmers to begin planting them.
It’s great that we started back in 2005.
Fighting Crop Disease
Cassava: can science save a diet staple?
In Tanzania last year, I visited with farmers whose survival – like that of millions of other Africans – depends on the cassava, a diet staple threatened by disease. I also visited with African scientists on the forefront of efforts to protect the cassava and other vitally important crops.

In Tanzania last year, I visited with farmers whose survival—like that of millions of other Africans—depends on the cassava, a diet staple threatened by disease. I also visited with African scientists on the forefront of efforts to protect the cassava and other vitally important crops.
Cassava is a staple crop that provides a basic diet for more than 500 million people worldwide.

Cassava is a starchy root that must be processed before eating because it contains small traces of cyanide. It is often grated, dried, and roasted to make garri, a flour; the leaves are eaten as vegetables in a stew.

When dried to a powder, cassava is known as tapioca.

These cassava plants are infected with mosaic disease, making the cassava root much smaller and less nutritious.

Christina supports her family by farming cassava. In the past two years, Christina’s crop has been invaded by two cassava diseases. Because of these diseases, she is depleting her savings to buy cassava to feed her three children. For Christina and other small farmers getting food is the most pressing daily concern.(Mapinga Village, Tanzania)

When I was in Tanzania last year, I met Dr. Joseph Ndunguru, a plant scientist leading a project to fight the mosaic and brown streak diseases that attack cassava crops. Dr. Ndunguru is part of a new generation of African scientists building up the capacity to do innovative science in Africa.

One Year Polio-Free
India Marks a Milestone for Child Health
This Friday will mark a full year since the last case of wild poliovirus was detected in India. This is a huge milestone in the history of global health. But the fight against polio is not over.

Four years ago, I visited India and saw again what polio does to children. I was in a slum in East Delhi, when I met a 9-month-old girl named Hashmin—paralyzed by polio—cradled in her mother's arms. She will never be able to do many of the normal things kids do because she has polio. Watching her was the strongest of reminders of the imperative of ending this terrible scourge once and for all.
The following year, in 2009, India had more polio cases than any other country in the world. But much has changed since then, and this Friday will mark a full year since the last case of wild poliovirus was detected in India. This is a huge milestone in the history of global health.
With a huge and growing population, hard-to-reach migrant communities, and sanitation and health conditions that limit the effectiveness of polio vaccines, this remarkable achievement in India marks clear progress in the fight against polio.
India really stepped up to the challenge on polio. The government of India funded its own eradication program. Twice a year, 2 million volunteers prepare 800,000 vaccination booths around the country—at schools, hospitals, and community centers. They immunize more than 172 million children one by one. Working with partners like Rotary International, WHO, and UNICEF, they have built an impressive infrastructure for delivering health services to some of the most underprivileged children in the world.
India’s story is proof that major health problems can be solved in the toughest places in the world. But the fight against polio is not over and we are at a critical moment in time.
In 2011, there were still a handful of countries with polio outbreaks. We must sustain funding to ensure a comprehensive immunization effort in India and other countries—until there are no more cases. If we don’t, the virus can spread back into countries where it has been eliminated, as it did last year in Russia and China.
Eradicating polio is a top personal priority and of the greatest importance at the foundation. Last year, I visited India again to see how the country was able to make such phenomenal progress. I also visited Nigeria and Chad to understand the challenges that lie ahead. I’m optimistic that we can vanquish polio forever if other countries choose to learn from India’s success. Together, we can accomplish something amazing.
Keep Giving
A plan to assist the world’s poor
Advances in agriculture, education, health, and sanitation have led to a dramatic decline in child deaths over the last 50 years. But the global economic crisis is putting at risk the development aid so critical to continuing this progress. As Congress considers foreign aid in the coming weeks, I encourage policymakers to consider the remarkable impact of American aid, its benefits to the U.S., and the contributions of a growing number of donor countries.

Fifty years ago, almost 20 million children under the age of 5 died every year. In 2010, the figure was down to 7.6 million. This 60 percent decline in childhood deaths — reflecting advances in agriculture, education, health and sanitation — is compelling evidence of the increasing justice in our world.
But the global economic crisis is putting the long-term trend of progress at risk, as Congress’s debates about the foreign aid budget underscore.
I am giving a report Thursday to the heads of the Group of 20 governments, including President Obama, suggesting creative ways for the world to continue investing in development despite fiscal constraints. I hope three key ideas become part of congressional deliberations over the coming weeks.
First, programs funded by U.S. generosity have been a core component of this 50-year project of raising living standards around the world.
Aid is targeted to fill specific gaps in development. The most important of these gaps is innovation. When the private sector doesn’t have incentive, and poor governments don’t have the money, smart aid pays for breakthrough solutions. The green revolution that fed a billion people in the 1950s and ’60s never would have happened without advanced agricultural science funded by U.S. aid. In just the past 10 years, millions of children have been saved from diseases such as measles and whooping cough by vaccines that Americans paid for through their contribution to an organization called the GAVI Alliance. Immunization is a great example of how aid can be effective. Thirty-six cents worth of measles vaccine protects a child for a lifetime.
Second, development isn’t just good for people in poor countries; it’s good for all of us. It used to be that the world was, roughly speaking, one-third rich and two-thirds poor. Now, the number of dynamic, healthy, highly educated countries is much higher, which is a recipe for prosperity. Imagine the world economy without Brazil, China, India, Indonesia, South Korea, Mexico or Turkey.
If countries that are currently poor can feed, educate and employ their people, then over time they will contribute to the world economy. On the supply side, they’ll increase the production of key commodities such as food, keeping prices lower. On the demand side, as their citizens are more productive, they’ll become important markets for trade.
But if people don’t get access to basic necessities, continued suffering will lead to economic stagnation and instability. It is, for example, not only unconscionable but also a strategic mistake to allow famine to devastate the livelihoods of millions of people in the Horn of Africa.
Third, the United States is not doing development alone. We spend about 1 percent of our total budget on aid, as do dozens of donor countries.
And with only a few exceptions, the amount poor countries spend on their own development is much greater than the amount donors invest. Ethiopia, for example, has in the past five years built 15,000 rural health posts to provide improved services for its citizens.
There is also a group of rapidly growing countries — including Brazil, China and India — that combine recent experience with development and significant technical capacity, giving them the insight and the skill to have special impact. For instance, China is sequencing 10,000 varieties of rice to help small farmers cope with climate change. These efforts can make a big difference. For example, a new submergence-tolerant rice variety being used in flood-prone areas of Bangladesh and India can more than double farmers’ yields. We predict that 20 million farmers will be planting this variety in the next six years.
The private sector hasn’t always invested as much in development as it should because the market incentives haven’t always been clear, but there are ways to encourage involvement. In my report to the G-20, I’ll make half a dozen recommendations for mobilizing tens of billions of dollars annually from private sources. The African diaspora is sitting on $50 billion in savings that could fund development in their home countries if it were captured through diaspora bonds.
If the transaction costs on remittances worldwide were cut from an average of 10 percent to an average of 5 percent, it would unlock $15 billion a year in poor countries. In addition, there are trillions of dollars in sovereign wealth funds, and a portion could be reserved for key infrastructure projects in poor countries.
Sometimes Americans get the impression that we’re shouldering the whole burden of development and that, ultimately, our aid doesn’t make a big difference. I see it very differently. We’re providing strategic investments that link up with many other investments to systematically make a better, more prosperous and safer world. If we do it right, we can keep shrinking the number of countries where aid is needed to zero.
This was originally published on November 1, 2011 in the Washington Post.
Advancing the MDGs
Foreign aid advances millennium development goals
In this photo gallery, meet some of the people who are helping their countries move closer to meeting the U.N. Millennium Development Goals.

From a Kunwasi village in Ghana to a Maksoodpur village in India, development aid is saving children’s lives, improving health conditions, reducing poverty and hunger, and increasing economic growth and stability. In this photo gallery, meet some of the people who are helping their countries move closer to meeting the U.N. Millennium Development Goals.
Ethiopia
Lomitaa, a health extension worker in Ethiopia, makes a home visit in Mojo village. To reduce suffering from preventable and treatable diseases, the government trained more than 32,000 women as health extension workers, to teach rural families about disease prevention and healthy living. It also created “health outposts” to provide basic medical services and preventive care in rural areas. Since the program’s launch in 2006, there has been a 35 percent increase in immunizations for diphtheria, tetanus and pertussis, and a 50 percent reduction in malaria. Health extension workers often walk miles to reach families in the most remote areas.
Nicaragua
Nicaraguan horsemen Julio Mesa Zelodon and his son Santos delicately balance a fragile cargo of rotavirus vaccines, which must be transported in an insulated box to preserve the drug’s effectiveness. Rotavirus is a preventable and treatable diarrheal disease that causes 500,000 deaths each year among infants and young children. Since the vaccine’s introduction in 2006, Nicaragua has seen a 77 percent decrease in severe rotavirus cases. The vaccine is often transported by horse, donkey or boat to reach the country’s most remote areas.
Ethiopia
Since Ethiopia emerged from 16 years of civil war in 1991, the country has made significant progress in poverty reduction, food security, health, nutrition, and education. Education reforms aimed at increasing access, especially for girls and the rural poor, increased student enrollment by 500 percent. School fees were abolished and funding was provided for adult literacy programs, school construction, and to train and hire teachers.
Ghana
Staple crops like cassava and yams as well as cash crops like tomatoes and peppers are on sale at a street side market in Kumasi, Ghana. Through agricultural reforms, farmers are better able to cultivate staples and grow cash crops for additional income, reducing the country’s hunger rate by 75 percent and cutting poverty nearly in half.
Ghana
Andres Yemetey from the Ghana Infant Nutrition Action Network discusses the benefits and proper techniques of breastfeeding with Estherlyne Larkai as she feeds her daughter at the Osu Maternity Home in Accra.
In the past, many women in Ghana supplemented breast-feeding with water, sugar water, or herbal concoctions that caused diarrhea and other problems. As the result of government education efforts, many women now feed their babies only breast milk, and men are encouraged to provide support to make that possible.
Cote d'Ivoire
Kevin Kouassi, 36, who is HIV-positive, works at the NDA Health Center in Dimbokro, Cote d'Ivoire. His job is to encourage testing, counsel those who come to the clinic, and educate them about prevention and treatment. Today free testing for HIV/AIDS is readily available in Cote d'Ivoire and can be done in as little as 15 minutes, ensuring that patients will stay to receive their results. Here, he counsels 24-year-old Aya who is six months pregnant with her second child and has come to the clinic for testing.
Viet Nam
In the last two decades, Viet Nam has become a major exporter of rice and coffee, and its manufacturing sector has boomed. The government has tapped the country’s economic growth to improve health, education, and water and sanitation services. Incomes have risen and the poverty and infant mortality rates have fallen dramatically.
Egypt
Until recently, most births in Egypt were at home and unattended by skilled personnel. Through education and outreach efforts, couples like Saad and Madiha have learned about the value of prenatal visits, medically assisted childbirth, post-partum care, and family planning. Targeted villages have seen dramatic improvements in maternal and child health, including a 27 percent drop in underweight babies.
Bangladesh
A Bangladeshi mother, Shahinoor, gives her child, Santo, oral rehydration solution. Commonly made of ingredients that poor households can afford, such as salt and unrefined brown sugar, oral rehydration therapy has saved the lives of millions of children from death due to diarrhea. Its widespread use, in combination with immunization campaigns for childhood diseases, has significantly reduced child mortality and malnourishment in Bangladesh and worldwide.
India
In 1975, the Indian government started the Anganwadi program, one of the largest child health and development efforts in the world. Here, Anganwadi worker Pushpa Kumari vaccinates a child against polio in a house-to-house campaign in Maksoodpur village. Between 1999 and 2007, India’s under-five mortality rate fell from 117 to 72 per 1,000 children.
Malaria Forum
Charting a course to end malaria
With continuing innovation, we can eradicate malaria.

In the past 10 years, the number of people who die from malaria has declined 20 percent.
For the past three days, the global malaria community has been meeting in Seattle, talking about what it’s going to take to get rid of the other 80 percent. The eradication of malaria is an ambitious goal and a long-term goal—but a goal Melinda and I are 100 percent committed to.
People used to say eradication was impossible, but we remain optimistic because human beings have a spectacular ability to innovate.
The tool that’s most associated with the recent progress against malaria is the long-lasting bed net. Bed nets are a fantastic innovation. But we can do even better. We can invent new ways to control the mosquitoes that carry the malaria parasite.
One of the problems with nets is that they can be uncomfortable to sleep under, so people sometimes chose not to. Researchers are testing spatial repellents that drive mosquitoes away right now. A family could hang a small coil from the ceiling and be protected, without having to accept a terrible night’s sleep.
One innovation the malaria community has been pursuing for decades is a vaccine. We have never had a vaccine for a parasitic disease, and the scientific complexity is dizzying. But at this week’s meetings I was pleased to announce interim results from the final-phase of a trial for a vaccine candidate called RTS,S. Among five to 17-month-old children, the vaccine prevented clinical malaria (which was defined as the presence of fever and parasites in a child who was ill and brought to a health facility for care), in 56 percent of trial participants over a period of one year. We still need to analyze the complete data when it’s available, but this vaccine could be licensed and protecting children by 2015.
We’ll keep on innovating and improving on this vaccine, but these results are a huge milestone in the history of our fight against malaria.
The malaria parasite has been killing children and sapping the strength of whole populations for tens of thousands of years. It is impossible to calculate the harm malaria has done to the world. But we have the ability to make generation after generation of better tools, and we can chart a course to end malaria.
More Work to Do
Why we must outsmart mosquitoes
The decisions we make now will determine what happens to malaria in the future.

On October 18, at the foundation’s second annual Malaria Forum, I spoke about the progress being made in the war against the dreaded parasitic disease. But more needs to be done to control and eradicate it, including a higher level of preventive drug treatment for pregnant women, additional research on chemical repellants, and further investigation of vaccines and drugs to treat those who are infected.
Prepared Remarks by Bill Gates
Thank you, Melinda.
Melinda told you about some of the people we met in Tanzania recently. I was impressed by a man named Prosper Chaki, who runs a larviciding project in Dar es Salaam. He spends his days wading into the standing water where anopheles mosquitoes breed, so he can poison them. It’s not so surprising that he’s gotten malaria 20 times.
“Mosquitoes are smart,” Mr. Chaki said. Then he told us, “We have to be smarter.”
I believe we will be smarter. One reason is that you have come from all over the world to this forum—to challenge each other, to disagree with each other, and to learn from each other. When you leave tomorrow, our team at the foundation will move forward with the benefit of the most rigorous thinking in the world. We are grateful to you for that, and I hope each of you will take inspiration back with you as you continue your personal fight against malaria.
The other reason I believe we will be smarter is that human beings have a spectacular ability to innovate. Innovation is one of the most powerful forces in the world. It can make the impossible, possible.
Melinda talked about the innovations that have changed the course of malaria and saved a million lives in the past 10 years.
But innovations are only as good as our commitment to delivering them. We have to get better at using the innovative tools we have.
Intermittent preventive treatment with drugs during pregnancy and infancy are two proven methods of protecting those most at risk from malaria, but they’re not saving as many lives as they should be. For example, most countries in sub-Saharan Africa provide IPTp in less than 20 percent of pregnancies. That is not good enough.
We have to demonstrate the same level of commitment as new tools come online. I am very optimistic that Seasonal Malaria Chemoprevention will be available starting early next year, when the WHO’s approval process is complete. We must be aggressive in launching pilot studies to understand how this intervention should fit into control strategies, so we save as many lives as possible, as quickly as possible.
We also have to be thinking simultaneously about the next generation of tools. If we think big, bring more partners into the fold, and take smart risks, we will invent novel tools—powerful ways of fighting malaria that don’t exist now. This is the kind of innovation that will enable us to plan for the eventual eradication of malaria.
Eradication is an ambitious goal—and a long-term goal. It is also a goal to which we remain 100 percent committed.
We are committed to it for moral reasons. My children will not die from malaria, thank God. Since that is true, no child should die. It should never be too expensive or too inconvenient to give the poorest a chance to survive when the richest already have it. Equity is not yet a reality, but it is what we believe in and what we are striving for.
We are also committed to eradication for strategic reasons. The only alternative to charting a course to the end of malaria is an eternity of trying to stay just one step ahead of the parasite and the mosquito. If we have to fight in perpetuity, the cost in lives will be enormous. The opportunity cost of never being able to divert our attention to other challenges will be incalculable.
I know some people in the malaria community worry that focusing on the uncertain goal of eradication could distract us from control measures that are working today. I understand the desire to stay focused on saving lives. But I don’t see eradication and control as two separate approaches to the fight against malaria. Instead, they are two compatible parts of a single approach. To achieve elimination and eradication, we need to start with control, drive it up to high levels, and sustain it. But if we don’t target elimination and eradication, control will lapse, and malaria will continue taking lives.
It will take leadership and innovation and money to extend the recent success. It will also take leadership and innovation and money to plan for malaria’s eventual eradication. The conclusion is daunting, but inescapable: We will need enough leadership and innovation and money to do both. We do not have the luxury of choosing one or the other.
I am an optimist. I believe we are capable of setting our sights on an ambitious goal with a generation-long time horizon and multiple, shifting milestones along the way. But eradication will never happen as long as it remains a general aspiration. We must turn it into a specific plan, and our job now is to lead the constant search for new and better tools that will help us execute our plan, step by step.
The best tool we have now is bed nets. Nets are a fantastic innovation, but they’re not perfect and they won’t be sufficient. They are expensive, they are unpleasant to sleep under, and they don’t protect against outdoor- and daytime-biting mosquitoes. There is a clear need for cheaper, easier to use, and more powerful vector control methods.
I am enthusiastic about spatial repellants, chemicals that can keep mosquitoes away from treated areas. Repellants could be a big improvement over nets, because the people benefitting from them wouldn’t have to make the choice to sleep under them every single night. The likelihood of human error or human resistance would shrink by a lot. And spatial repellants would be effective against all types of mosquitoes, no matter when or where they bite.
Recent trials in China showed that mosquito coils containing a chemical repellent decreased people’s odds of contracting malaria by about 80 percent—and coils plus nets were much more effective than coils or nets alone. Right now, additional trials are taking place in Indonesia to confirm the impact of coils on transmission and to measure their impact on the mosquito population. We expect data from this critical proof of principle study in the middle of next year.
Researchers are also busy identifying potential active ingredients for spatial repellants. Larry Zwiebel of Vanderbilt University just isolated a compound that is 1,000 times more powerful than DEET. Other researchers are looking at other formulations, and results from these studies will be available in two or three years.
ACTs are the second tool that has changed the course of malaria control over the past several years. Obviously, they represent a vast improvement over the old drugs that weren’t effective, but, like nets, they are not ideal. Artemisinin is expensive, the course of treatment lasts several days, and resistance is already developing.
The Medicines for Malaria Venture currently has a drug candidate in phase II trials, OZ 439, that has the potential to be a single-dose cure. This could solve many of the problems with ACTs. It should be cheaper, since the total amount of drug needed for treatment will be lower. Adherence will be much higher, since people will have adhered completely as soon as they swallow the pill. This will decrease the risk of treatment failure and slow the development of resistance.
OZ 439 could be licensed as early as 2016, depending on the suitability of the quinolines currently being tested as partner drugs. In addition to finishing the trials, MMV is working to find a partner from the pharmaceutical sector to help it make and market OZ 439 when the time comes.
One of the most important innovations for the future of the fight against malaria will be a tool we don’t yet have: a vaccine. A vaccine is a wonderful thing. It’s the simplest, most cost-effective way to save lives. The smallpox vaccine, plus the innovative approach of ring vaccination, led to the eradication of smallpox. The polio vaccines have pushed the world to the threshold of eradicating polio. Vaccines have slashed the number of deaths caused by diphtheria, measles, tetanus, and a host of other diseases.
But the search for a malaria vaccine has been a long and frustrating process. There has never been a vaccine for a parasitic disease. The scientific complexity is dizzying.
Today, however, we are closer than ever before to tackling that complexity. Four years ago, I announced interim results from phase II trials of the RTS,S vaccine. Today, I am pleased to announce the interim results from the phase III trials. Among five to seventeen month old children, the vaccine prevented clinical malaria in 55.8 percent of trial participants over a period of one year. RTS,S prevented severe malaria in 47.3 percent of trial participants aged five to seventeen months. It prevented severe malaria in 34.8 percent of the entire study population, including infants.
These are only interim results. We need to study the data over a longer period of time to understand whether the effect of the vaccine diminishes. We also need to evaluate the impact of a booster dose. Leaders must have all this information before they can make decisions about how to use the vaccine if and when it’s approved.
Nevertheless, these results signal a huge milestone, and I want to congratulate the many partners that have been working on this project for decades. First, this is proof that it is possible to create a vaccine that is effective against malaria. For a long time, we didn’t know. Now, we know. Second, if RTS,S continues to show effectiveness of around 50 percent—above and beyond bed nets—it has the potential to protect millions of children and save thousands of lives.
And RTS,S is a first-generation vaccine. It is an early outcome of a long process of innovation that will ultimately yield more effective vaccines. Researchers are currently recruiting participants for the phase I trials of a second-generation RTS,S vaccine.
There are many vaccines that work according to completely different mechanisms in various stages of development. I am particularly excited by the potential of transmission blocking vaccines, vaccines that prevent mosquitoes from picking the infection up from human hosts. In the drive toward elimination and eradication, these vaccines will be invaluable.
But the fact is there are still many basic science questions about malaria that we need to answer to make the search for vaccines less challenging. We know there are mechanisms by which people become immune to malaria. We can even produce that immunity artificially, but we don’t understand it. If we get a better sense of what underlies immunity in those cases, we will have a much better chance of filling the vaccine pipeline with good products.
As we develop these new tools, we also have to develop a more sophisticated understanding of how to deploy them. When you have several ways to fight more than one species of parasite, carried by many species of vector, you can’t afford to guess about strategy. What is the smartest way to combine our interventions so they have the maximum effect? We need to be able to answer these questions with evidence.
I believe modeling can help generate that evidence. I want to walk you through some charts from one malaria model to give you a sense of the kinds of answers they can provide.
When our friend and mentor Warren Buffett made his gift to our foundation five years ago, he was clear about the purpose philanthropy should serve. One of his famous quotes about finance is, “I don’t look to jump over 7 foot bars. I look around for 1 foot bars that I can step over.” Philanthropy is the other way around, he tells us. We should be looking around for the 7 foot bars; that’s why we exist.
Malaria eradication is a high bar. To reach it, it will take a constant, concerted effort to innovate. But we can do it. We can drive down the number of cases, lower and lower. We can keep introducing new and better tools, until we interrupt transmission like we’ve done in dozens of countries already. And, eventually, with relentless focus, we can eradicate malaria. We’ve already shrunk the malaria map considerably. We can make it disappear.
It won’t happen in four years, or in eight years. But the decisions we make now will determine what happens to malaria in the future.
The parasite has been killing children and sapping the strength of whole populations for tens of thousands of years. It is impossible to calculate the harm malaria has done to us. Now, we can chart a course to end it.
Thank you.
In Africa
Visiting Tanzania: A Battleground in the Fight Against Malaria
On my most recent trip to Tanzania, Melinda and I spent time looking into how the foundation’s partnerships to reduce malaria are progressing.

On a recent trip to Tanzania with Melinda, we spent time focused on the foundation's efforts to reduce malaria. We were particularly interested in learning about the progress of research into a malaria vaccine.
Bagamoyo District Hospital
These children were waiting to see a doctor at the Bagamoyo District Hospital in Tanzania. They are among several thousand children participating in field trials of the vaccine, known as RTS,S. Just this week, interim results from the clinical trials were reported, and they prove that it’s possible to create a vaccine that’s effective against malaria. It was exciting to visit this clinic because it is so well run, they're offering lots of good health services, and people are coming from far away to participate in the vaccine trial.

Meeting with Health Officials
We met with health officials from the Bagamoyo District Hospital and the Ifakara Health Institute. There were a lot of visiting scientists from the Swiss Tropical and Public Health Institute, which has a close relationship with the IHI. We saw scientists who are working on ways of repelling mosquitoes so people don’t just have to rely on bed nets, which are only partly successful protection against malaria. It's great that the foundation’s support is helping with the vaccine, and that it is also helping train young scientists and building up a research infrastructure, which will have a lot of long-term benefits.

Ifakara Health Institute
Scientists at the Ifakara Health Institute were great at educating us about their work, including techniques for capturing mosquitos to help prevent malaria, what species of mosquito they were focused on, how they get the vaccine out into the field, and how they saw if the vaccine worked.

Meeting with Hospital Staff
We also met with staff at the local hospital to discuss progress treating and preventing malaria.

Mapinga Village Dispensary
We visited the Mapinga Village Dispensary, which is an example of how healthcare is delivered in Africa. These dispensaries are the first place people go for care in or near their villages. We saw how the dispensaries keep their vaccines, and we talked to people like Neema Malachi Najwale, the nurse in charge of the Mapinga Dispensary, about how they get mothers to come in for the vaccines. We also talked about how they can now use cell phones to send regular status reports on their inventory.

Meeting with Parents
We talked with some of the parents of children participating in the vaccine trials. Although Tanzania is quite poor and hasn't developed a very extensive infrastructure of roads and electricity, in the health area they've done pretty well. They have good vaccine coverage and are on track to meet a lot of the Millennium Development Goals. It’s a great example of the progress taking place in Africa.

Defeating Malaria
At the Mapinga Village Dispensary, we talked with the head nurse about a number of diseases they have to deal with besides malaria. But by far the biggest killer of children and adults in that area of Tanzania is malaria. So the enthusiasm among health officials for the new malaria work there is very high. I’m an optimist when it comes to defeating malaria. There is good progress with the vaccine, drugs to prevent and treat malaria, and other preventive measures. Eradicating malaria won’t happen overnight, but it’s a moral and economic imperative for Africa, and for the entire world.

A Childhood Terror
The history of polio in the U.S.
David Oshinsky remembers growing up in an America terrified by polio—a plague that put every child at risk until a vaccine was finally developed in the mid-1950s.

David Oshinsky, the author of Polio: An American Story reflects on the history of polio and the final push needed for eradication.
First Pledges
GAVI raises $4.3 billion at first pledging conference
Today we get to celebrate a significant milestone for global health equity.

The GAVI Alliance, an organization that helps make sure children in poor countries get the same vaccines that children in rich countries do, just met its fundraising target for the next four years. They did it despite the fact that donors everywhere are coping with budget crises.
This news comes on the heels of an announcement by several multinational and developing country vaccine manufacturers that they will be lowering the prices of some key vaccines. Together, these developments mean that we can save more than 4 million additional lives by 2015.
Vaccines are one of the best long-term investments to prevent disease and give children a healthy start in life. But for a long time, the healthiest children in the least danger were getting vaccines, and the children who needed vaccines the most weren’t getting them. In many cases, it took decades before vaccines made for developed-country markets were available in poor countries. Take the example of rotavirus, the leading causes of diarrheal disease. Only children in poor countries die from rotavirus, yet the vaccines for the disease was made available first in rich countries!
That’s why increasing access to vaccines for the world’s poorest countries is one of the top priorities of the Gates Foundation, and that’s why today we pledged an additional $1 billion to support the lifesaving work of the GAVI Alliance over the next five years. We were joined by many other donors who understand that buying vaccines saves lives, and who know it is an investment worth making, no matter how tight their budgets.
How We Fight Epidemics
Tackling TB Through Innovation
I explored innovation in testing and treating tuberculosis, as I spent World TB Day in India.

Many people think tuberculosis is a disease of the past, but this ancient epidemic remains a huge global problem. Each year there are 9 million new TB cases and 1.7 million deaths.
Yet there is a tremendous opportunity to turn this situation around. Most new TB cases are in major emerging economies like India, China and South Africa, which have a remarkable history of using innovation to address tough health challenges. They are adopting new TB strategies, and are poised to develop the next wave of innovations. This could change the way the world fights the epidemic.
The major problem is outdated tools. TB is preventable and treatable, but the most common TB test is more than 125 years old and misses half the cases. By the time most TB patients are correctly diagnosed and treated, they may have unknowingly infected many others – creating an endless cycle.
At the same time, today’s TB drugs are more than 40 years old and take six months to work. The combination of poor tests and outdated treatments is driving the spread of drug resistance, undercutting global efforts to stop the epidemic.
I witnessed this firsthand in 2009, when I visited the King George V TB hospital in Durban, South Africa. I met a woman with HIV who had been diagnosed with a highly drug-resistant type of TB. She told us about the despair she felt when she learned she had such a dangerous form of the disease.
Fortunately, there is a promising pipeline of new TB diagnostics, drugs and vaccines under development. And we are starting to see results. Just today, I saw how India is using these innovations. I marked World TB Day by visiting the state-of-the-art L.R.S. Institute of Tuberculosis and Respiratory Diseases in New Delhi with Dr. Ashok Kumar, head of India’s TB program. L.R.S. uses a new molecular test, GeneXpert, which can accurately determine whether a patient has TB in about two hours.
Molecular diagnostics could revolutionize TB care, and things will continue to improve as the price comes down and new tests are developed. This is where India could have global impact. India is a leader in developing low-cost health technologies, and the country could produce high-quality, inexpensive molecular TB diagnostics. This would increase access at home and across the globe.
Meanwhile, South Africa is stepping up its own efforts. The country will likely begin widespread use of GeneXpert soon. This could profoundly impact health in a country where thousands of lives are lost each year to TB/HIV co-infection.
India and South Africa’s leadership shows the extraordinary potential for high-burden countries to pioneer TB innovations. Their success could be a model for other countries—and save millions of lives in the process.
Let's Finish the Job
My Annual Letter: End Polio Now
Polio, once a worldwide scourge, threatens to make a comeback unless all countries do their part to eliminate it. Eradication is tantalizingly close but funding to fight the disease still falls short.

Aid for the poorest has already achieved a lot. For example, because of donors’ generosity, we are on the threshold of ending polio once and for all.
Polio is a terrible disease that kills many and paralyzes others. Fifty years ago it was widespread around the world. When you talk to people who remember polio in the United States, they’ll tell you about the fear and panic during an outbreak and describe grim hospital wards full of children in iron lungs that maintained their breathing. At its peak in the United States in 1952, polio paralyzed or killed more than 24,000 people.
As a result of mass mobilizations to administer the polio vaccine, polio was eliminated in the United States and most developed nations decades ago. Most people who live in rich countries assume the disease is long gone and that it doesn’t kill or paralyze children anymore. But it is still a frightening presence in a number of places around the world.
In 1988 the global community adopted the goal of ending polio altogether. At that time more than 350,000 children a year worldwide were killed or paralyzed by the disease. Since then, vaccination coverage has increased significantly and the number of cases has gone down by 99 percent, to fewer than 1,500 last year. There are now just four countries where polio transmission has never been stopped: India, Nigeria, Pakistan, and Afghanistan.
That’s incredible progress, but the last 1 percent remains a true danger. Eradication is not guaranteed. It requires campaigns to give polio vaccine to all children under 5 in poor countries, at a cost of almost $1 billion per year. We have to be aggressive about continuing these campaigns until we succeed in eradicating that last 1 percent.
Therefore, funding is critical to success. Organizations such as Rotary International and the governments of India, the United States, the United Kingdom, and Japan are all major contributors to the polio campaign. Our foundation gives about $200 million each year. But the campaign still faces a 2011-12 funding gap of $720 million. If eradication fails because of a lack of generosity on the part of donor countries it would be tragic. We are so close, but we have to finish the last leg of the journey. We need to bring the cases down to zero, maintain careful surveillance to ensure the virus is truly gone, and keep defenses up with polio vaccines until we’ve confirmed success.
Why is it so important to end polio? Eradication will have three huge benefits.
The first is that getting rid of polio will mean that no child will die or be paralyzed by the disease in the future. One thing most people don’t realize is that if we don’t finish the job on eradication, we will lose a lot of the ground we’ve gained over the past two decades. The disease will not stay at its current low level. If we don’t get rid of it, it will spread back into countries where it’s been eliminated, and it will kill and paralyze children who used to be safe. Only eradication will guarantee that all children are safe.
The second benefit is that the money that will be saved by eradicating polio far exceeds what we are spending on eradication efforts now. The long-term benefits of the last couple of billion dollars spent on eradication will be truly phenomenal. A recent estimate added up the cost of treatment that won’t be necessary and the enhanced economic contribution of adults who won’t get polio. Eradication could save the world up to $50 billion over the next 25 years.
The third benefit is that success will energize the field of global health by showing that investments in health lead to amazing victories. The eradication effort illustrates so well how a major advance in the human condition requires resolve and courageous leadership. To win these big important fights, partnerships, money, science, politics, and delivery in developing countries have to come together on a global scale.
The history of polio and polio eradication is fascinating. (One of the best books I’ve read on the subject is David Oshinsky’s Polio: An American Story.) Polio was the first disease that raised significant money from the broad public. The March of Dimes was created to combat the disease. Although President Roosevelt and lots of Hollywood stars helped the campaign, its huge success came from neighborhood-based fundraising. I remember March of Dimes volunteers ringing our doorbell when I was growing up and asking for a donation. By any measure, the public’s generosity in supporting that charity made it one of the most successful health-related fundraising campaigns ever.
The March of Dimes funded research into the first polio vaccine, which was invented by Dr. Jonas Salk and introduced in 1955. It was such an important priority to get the polio vaccine out widely that the U.S. government sponsored the campaign, which it had never done before. The campaigns of the late-1950s were wildly successful, and by 1961 the number of cases in the United States was down to just 161.
A second polio vaccine—this one in the form of liquid drops that children swallow instead of an injection in the arm—was invented by Dr. Albert Sabin and licensed in 1963. By 1979 there was no more poliovirus in circulation in the United States. Dr. Salk’s and Dr. Sabin’s vaccines are still the key tools used for eradication today.
To this day, the smallpox campaign is the only successful human disease eradication campaign in history. At its peak, smallpox killed over 2 million people every year and also blinded and disabled large numbers. The eradication campaign started in 1967, the last naturally acquired case of smallpox was in 1977, and the world was certified as being free of smallpox in 1979. (Two excellent books on the smallpox eradication are Dr. D.A. Henderson’s Smallpox: The Death of a Disease and the forthcoming House on Fire by another key smallpox warrior, Dr. Bill Foege.)
Smallpox had a number of characteristics that made it easier to eradicate than polio. Almost everyone who got smallpox developed a distinct rash. In contrast most polio infections are not noticed because less than one in 100 people infected are paralyzed, even though all those infected can transmit the virus. This means by the time a paralytic case is found, the poliovirus has probably spread.
Also, the vaccines against polio are not as effective as the smallpox vaccine, which was so powerful that a single vaccination protected almost everyone. In the case of the most common polio vaccine, at least three doses are required to get 85 percent of children fully protected. In many countries of the developing world, even more doses are needed to reach the immunity levels needed to stop transmission of the virus.
But the polio campaign also has some huge advantages that the smallpox campaign did not have. The advanced science we have today lets us sequence the DNA of the polio virus and develop an understanding of the history of transmission, which guides our work. We also have far better communications and modeling tools than were available in the 1970s, and those are being used in smart ways to respond rapidly to every outbreak.
In 2003 I would have said we were just a couple of years away from ending polio, and I would have been wrong. That year there were false rumors in Nigeria that the polio vaccine caused women to become sterile. This allowed the disease to have a resurgence and to spread to many other countries. The experience of 2003 serves as a reminder to be humble as we move forward. But humility does not mean fatalism.
Fortunately those false rumors have been almost completely eliminated through the leadership of key political and religious figures. In 2009 when I visited Northern Nigeria to meet with the most important traditional leader, the Sultan of Sokoto, he committed to the campaign. It was fantastic to see him publicly giving his support. (He also gave me a horse to thank me but I told him I couldn’t take it.)
Last year both India and Nigeria had substantially fewer cases than ever before. In India the number of cases went down from 741 in 2009 to just 41 in 2010. In Nigeria, thanks in large part to the renewed leadership in the northern part of the country, the number went down from 388 to just 18. But alongside the phenomenal progress was another reminder that gains can be lost without sustained action.
The majority of cases in 2010 were in countries that had been polio-free until the virus travelled back across borders and caused outbreaks in areas where people had gotten lax about vaccination. There was a large outbreak in Tajikistan in the first half of 2010 and another in Congo in the second half. In both regions there were a number of immunization campaigns organized as a response. Today the outbreaks appear to be under control.
What those outbreaks in formerly polio-free countries prove is that eradication is a global project requiring every country to do its part. Very few projects demand global participation. In most areas each country can pursue its own approach, and countries can compare outcomes to see which approach is the most successful.
Philosopher and historian Will Durant once observed that the only thing that could get countries to join forces would be an alien invasion. To my mind, terrible diseases are surrogates for an alien invasion. If we are to succeed, the world needs leadership from a global institution and significant, coordinated resources from rich countries to fund activities in the poorest countries.
For polio, the World Health Organization (WHO) has played the central role with Rotary International, the Centers for Disease Control, and UNICEF as key partners. Polio eradication has benefited immensely from having Rotary’s support. Rotary had the vision to get involved in 1985 and has kept polio eradication as its top priority. Everywhere I go to learn about polio, I see Rotary members helping out with the hard work.
I feel sure that with continued support we will be able to show significant progress building on this year’s work. The site www.polioeradication.org tracks the key parts of the campaign including fundraising and the latest cases. I will make a number of trips focused on polio this year, including additional trips to India and Nigeria, and will write a report for the foundation website. For anyone who wants to support the polio campaign, which would be fantastic, visit www.rotary.org/myrotary/en/take-action/end-polio.
Not Letting Up
Going the last mile in India
Eastern India's Bihar state closes in on eradicating polio.

“The last mile is when people get most fatigued,” says Dr. Hemant Shukla, who leads polio eradication efforts in eastern India’s Bihar state. But having made major strides against polio, India now is closing in on it with vaccination programs for nomadic peoples and others who are hardest to reach.
Be Prepared
Annual Letter: A health emergency
I’m willing to be seen as a troublemaker by people who are happy with the status quo on global health.

Malaria: Progress on Multiple Fronts
The fight against malaria is making very good progress. The death toll, overwhelmingly of young children in Africa, went down from 985,000 in 2000 to 781,000 in 2009. Of the 99 countries with malaria, 43 have decreased cases of the disease by more than 50 percent. Turkmenistan and Morocco were recently declared malaria-free. For these communities the reduction in both death and sickness makes a huge difference. And it is possible only because of increased donor spending, which reached $1.5 billion in 2009.
The Roll Back Malaria group, with strong support from the WHO and our foundation, has set an aggressive goal to provide bed nets to almost every household that needs them in the next few years. As coverage goes up from its current level of 42 percent, it will have a dramatic impact. In Senegal, where 80 percent of households own a bed net, the number of malaria cases went down 41 percent in a single year. Many amazing grassroots groups are helping with the delivery of bed nets. The Nothing But Nets campaign, for example, has gotten hundreds of thousands of individual citizens and organizations like the United Methodist Church and the National Basketball Association involved in the fight against malaria.
We are also working on lowering the cost of the anti-malaria drugs containing artemisinin, which are expensive enough that people are still using less effective drugs instead. The approaches range from breeding the plant that provides artemisinin to have a higher yield, to using very advanced synthetic chemistry that can make artemisinin starting with simple sugars.
As is the case with all infectious diseases, the ultimate tool against malaria would be a low cost, highly effective vaccine. The RTS,S vaccine, developed in partnership with the pharmaceutical manufacturer GSK, is in its final phase-3 trial stage. Interim data will be available later this year, and we should have final results by 2015. A number of other vaccine candidates that might be even more effective or might be combined with RTS,S are also making progress, and several will start human trials this year.
Saving the Youngest Children
Of the 8.1 million deaths per year of children under the age of 5, over 40 percent happen in the first 28 days of life, or the neonatal period. The good news is that we are headed in the right direction. In 1995 there were an estimated 5.6 million neonatal deaths. The most recent estimates show the number down to around 3.6 million.
Unlike the deaths that take place after a child is 28 days old, almost all of which can be prevented by inventing and delivering vaccines, reducing these early deaths requires a range of approaches. Some require new tools such as an ointment for the baby’s skin that prevents infection and an antibiotic solution for cleaning the cut umbilical cord. However, many of the key interventions involve social and behavioral change. You can have a huge impact (on both newborn and maternal health) by increasing the number of births done by a skilled provider in a clinic. It’s also important to teach mothers to wash their hands before handling a baby, to have frequent skin-to-skin contact with their babies, and to breastfeed exclusively for the baby’s first six months. (Mother’s milk contains not only key nutrition but also antibodies that block infection until the baby’s immune system is ready to operate on its own.) Where all of these elements come together, neonatal deaths can be reduced by 50 percent or more, so it’s critical that we learn more about how to teach and motivate mothers effectively, especially at a large scale.
Melinda has been a strong leader on maternal and child health issues. She gave an especially powerful speech last year to the Women Deliver conference. The plight of mothers and their babies is something she feels deeply, and it’s something we talk about a lot.
When she came home from a trip to Malawi she shared the experience of seeing two babies in a hospital in the town of Lilongwe, lying side-by-side in the same incubator. They were born within hours of each other. Each had suffered the same condition—they were unable to breathe at birth. Sadly, it was clear that only one would survive. That baby’s mother had made it to the donor-funded hospital in time for her delivery and was able to get the care she needed. Her baby was immediately resuscitated, which saved his life. The other was not so fortunate. He was born on the way to the clinic, on the side of road, and was not resuscitated soon enough. I wish everyone had a chance to experience what Melinda did, so they could see how things are improving but also understand the urgent need to do more.
HIV/AIDS and the Need for Leadership
Progress continues in fighting the AIDS epidemic, but the pace is slow. The rate of HIV infection has been reduced by almost 20 percent over the last 10 years, to fewer than 2.7 million infections per year. The number of people dying from AIDS has gone down by more than 20 percent in the last five years, to fewer than 2 million annually. Given all the lives that are at stake, I am impatient enough about this that I am willing to be viewed as a troublemaker by people who are happy with the status quo.
The war against AIDS is being waged on two fronts—treating those who are already infected and preventing new infections. Treatment continues to be scaled up, with more than 5 million people receiving HIV drugs. This is a great success story. Rich country generosity has been crucial and the execution in poor countries has been strong. However, there will not be enough money to treat everyone who will become infected if we don’t halt the progress of HIV. Because we don’t have a cure for AIDS, treatment has to continue for a patient’s entire life. That means costs continue to increase as you put more and more people on treatment.
Even without including people who will become infected in the future, the cost of treating the 33 million people living with AIDS today would be over $40 billion per year at current costs—over four times as much as is provided in aid today. To minimize the funding gap we need to reduce per patient costs of treatment. Drug costs have already been reduced to less than 20 percent of treatment costs. Most of the future savings will have to come from treatment models that reduce personnel, laboratory, and overhead costs. The difficulty of funding treatment makes it clear how important it is to prevent new cases. The sooner we make progress the better. There needs to be a sense of urgency that doesn’t exist yet.
Prevention breaks down into several different areas. The easiest should be preventing mother-to-child transmission since it simply involves giving a mother drugs to prevent transmission to her child. There is a lot of focus on getting from the current number of over 300,000 infections per year to zero. Another prevention approach is counseling people to change their behavior, including avoiding risky acts and using condoms. Then we have prevention approaches that rely on new tools. We now have three tools that have shown significant impact. The first is male circumcision, which I discussed last year. Amazingly, teenagers in communities with high HIV incidence show a high willingness to be circumcised. Kenya is leading the way with over 200,000 circumcisions performed. However, there are over 10 million men in high-risk settings in Africa who would benefit from male circumcision, and we should be scaling up 10 times faster than we are.
Another new tool is a vaginal microbicide gel that a woman can use to protect herself. A recent trial showed a gel containing tenofovir protected women against infection. Now the question is how long it will take before the gel is rolled out on a large scale. As someone outside the field, I am surprised at the number of steps it takes. First the product has to be licensed, which requires approvals from regulatory groups in both the country where the product will be used and donor countries. Many of these approval steps happen serially rather than in parallel, and it is only when the entire approval process is complete that the product can be rolled out. Even then the process isn’t complete because a whole system for delivering the product needs to be put together, and again a lot of these steps proceed in a slow serial fashion.
Another new prevention tool, PrEP (Pre-Exposure Prophylaxis), involves someone without HIV taking an anti-HIV drug on a regular basis to block infection. A PrEP trial showed a strong prevention benefit for the participants who consistently used the drugs and a weaker impact when all the participants were included. With both microbicides and PrEP I think countries with large epidemics should figure out how to do large community trials as soon as possible. This would shorten the time before all patients have these lifesaving tools by many years.
If the United States had an epidemic where almost half the girls in large neighborhoods contracted a terrible disease, we would find a way to cut through all the complexity. With HIV it is more difficult since there are many countries involved. But we need to work creatively to shorten these delays.
The best tool would be a vaccine for HIV. The scientific progress on this has gone well. The positive results of the trial in Thailand were a turning point for the field, and blood samples from the volunteers are being studied in depth for lessons about why that vaccine worked but only to a limited degree.
There has also been an explosion in the discovery of antibodies that block HIV infection. Scientists don’t yet know how to make a vaccine that will cause patients to generate lots of these antibodies, but there are several approaches that look promising and will be ready to go to trials in the next few years.
In order to get a fully effective HIV vaccine we will almost certainly need several rounds of trials where we learn and improve the candidate vaccines. So to get a vaccine as soon as possible we need to minimize the length of the trials and the time between trials. So far each cycle has taken over five years. The field needs to look into how to shorten this so that progress matches the urgency of the problem.
Building Dreams
In China, speeding toward the future
In September 2010, I traveled through China to visit with vaccine makers, computer scientists, energy technology companies and car manufacturers.

I travelled to China for the first time in 1990 on Microsoft business and have been back many times since. One very memorable trip was in 1995 with Melinda, my father and Warren Buffett. We rode the trains and traveled around as tourists for several weeks—it was an incredible trip and a lot of fun.
My recent trip was unique and especially exciting, as I had the opportunity to do work that spans my various interests. I met with our team at Microsoft Research Asia, where I saw some incredible innovations in search and related technologies. I also met with a number of vaccine companies that are working with our foundation. For the last part of the trip, I joined Warren Buffett, Charlie Munger and other Berkshire Hathaway board members. Our main focus was a visit to BYD, an incredible company in which Berkshire owns a 10 percent stake. BYD fully lives up to its name, which stands for Build Your Dreams. It manufactures batteries, electric and hybrid cars and buses, and many highly innovative green products.
The meetings with vaccine manufacturers were about the potential for expanding development of new vaccines in China for use worldwide. Historically, most important vaccines have originated in Europe and the United States. Now, countries like Brazil, India and China are providing lower-cost versions of some of them. Ideally, they’ll also get involved in inventing new vaccines. Because these countries suffer from many of the infectious diseases that we need new vaccines for, local development could help speed vaccine dissemination. Also, because countries like China have experience in making low-cost vaccines, they could be better at designing new ones in ways that make them low in cost from the very beginning. That would be wonderful.
And so the foundation is reaching out to new vaccine companies, seeing how we can help them and what holds them back. This was my first visit with some of the companies in China. I was impressed at how quickly the industry is moving ahead. They really understand low-cost manufacturing, and they’re getting their quality up to world standards. Over the next five to ten years, they have the potential to create many breakthrough vaccines, as well as to help get current vaccines to the world’s poorest people, for whom price can be a significant obstacle.
Specifically, the foundation is trying to make sure that every child in the world gets three vaccines: pentavalent (against diphtheria, tetanus, whooping cough, hepatitis B and influenza B), rotavirus (against severe acute gastroenteritis) and pneumococcal (against pneumonia). Together, these three could reduce child deaths by almost one million per year. If we can get their cost down, then we’ll be able to get all three to even the poorest children in the world. It looks like China could help out on low-cost rotavirus and pneumococcal. So we have possibilities there, as we do in India and Brazil.
Gearing up to manufacture vaccines that meet international standards is a costly and complex process. In China we saw a flu vaccine manufacturing line that is unique in that it involves growing flu virus in chicken eggs. The plant has to buy a huge number of eggs and make sure they're all sterile. It’s quite a process, and people worry that, in the event of a big epidemic, they might not be able to buy enough eggs and grow the virus quickly enough. But in our visit to Sinovac Biotech, headquartered in the Beijing University Biological Industry Park, we saw that it has really distinguished itself by rapidly building up its flu vaccine capability. That was quite impressive.
I love any excuse for spending time with Warren Buffett, whether we’re playing golf (which neither of us is very good at) or playing bridge, which we're kind of just okay at.
Our visit to BYD was amazing. The company was started back in 1995 by a battery expert. It grew to be very strong in phone batteries and car batteries, and then, in 2003, BYD decided to make its own cars. It has about six percent of the domestic car market and plans to expand its product line and volume quite dramatically. It’s an innovative company, pushing forward on battery technology, doing electric taxis, electronic buses and electric storage systems.
BYD has created an entirely electronic bus using special batteries and a special electronic motor. The company has innovated to bring the battery cost down and the battery life up. If it works as well as planned, the operator saves enough on fuel to be able to pay quite a premium for the bus. We rode around on a prototype and participated in a ceremony where a local city committed to buy a thousand of these buses. They will be a huge help in reducing the smog in Chinese cities and could even help start to reduce CO2 emissions.
BYD headquarters is in Shenzhen, in the southeast part of China next to Hong Kong. Shenzhen is where the Chinese economic miracle started; it was a special economic zone. So I wasn’t surprised to see a lot of modern buildings and a pretty impressive car factory. But I was blown away when I heard how quickly they put up the buildings. In the U.S., you just can’t build nearly as fast.
What was even more amazing was to go to a city in the middle of China, Changsha, which has six million people, and see a new factory that will turn out 400,000 cars a year. It was built in less than two years from start to completion. Around the city, new high-rise buildings are going up where only cornfields stood just a few years ago. You hear about China’s 10-percent annual economic growth, but to fully understand you really have to see it in person. China is moving at incredible speed.
Hello, Biosensor?
Cell phone science
Most of us think of cell phones primarily as a convenient tool to stay in touch with people and store information. But increasingly, scientists are exploring ways to use cell phones to deliver critical health care to people in developing countries.

If you’re like me, you’ve probably become quite attached to your cell phone. These amazing devices allow us to do things that previously could be done only with a computer, such as search the Internet, read books, watch TV and movies, and purchase things online.
But what I find even more impressive is how researchers are examining ways to put cell phones to use to improve health in developing countries. This week, the foundation announced grants of $100,000 each to eight scientists who are pioneering the use of cell phones to improve health care in communities where resources are limited. The grants are part of Grand Challenges Explorations, a foundation-funded effort to jumpstart unconventional projects that we believe have the potential to improve global health.
For example, Peter Lillehoj and Chih-Ming Ho of the University of California, Los Angeles, received a grant to develop a disposable malaria biosensor based on a SIM card platform. The SIM card-biosensor will allow malaria detection to be performed using a cell-phone, which will make diagnostic testing more widely available in rural and remote areas.
Terry Ferrari of World Vision will be field testing the use of two cell phone modules that will help community health workers in Mozambique caring for pregnant women and newborns to assess, to take action, and to refer cases with complications and emergencies. Another mobile-phone based tool being developed by Marc Mitchell of D-Tree International uses clinical algorithms to quickly identify women at risk during labor and delivery and assist with emergency transfer to a hospital. If these tools are successful, they could significantly reduce maternal and infant mortality rates.
Mark Thomas will be leading a team at VaxTrac to field test a mobile phone-based vaccination registry that uses fingerprint scans to track people who have received immunizations. The goal is to reduce redundant doses and increase coverage levels in developing countries.
I shared information about these and other innovative cell phone projects that we’re funding today at the 2010 mHealth Summit, an international conference focusing on the use of mobile technology to improve health care in the developing world.
Cell phones are amazing tools. For some of us, they’re about staying in touch. For millions of people, it could be about staying alive.
Showing Promise
Discovery science – taking the challenge
Five years ago, the Bill & Melinda Gates Foundation awarded $458 million to research projects aimed at creating breakthrough treatments for diseases that cause millions of deaths each year in developing countries. The results are showing promise and leading to new approaches in discovery science.

This week in Seattle, I’ll be speaking at our annual Grand Challenges in Global Health (GCGH) conference. We’ll be looking at what has been accomplished and what we’ve learned since awarding the first round of GCGH grants in 2005.
We launched GCGH five years ago with an ambitious goal: find innovative ideas to tackle the most persistent health issues in developing countries. We knew that to find the tools we needed to improve health around the world, we had to think beyond conventional science. We turned to the best, most creative minds from all scientific fields—immunology, physics, biology and even engineering—and asked them to apply their talents to global health research.
In five years, scientists from around the world have taken up this challenge. For example, Dr. James Baker, a scientist and professor at the University of Michigan created a new way to prepare and administer vaccines as nasal drops. They don’t require constant refrigeration—a huge challenge in many developing countries. During the grant period, Dr. Baker was able to apply this technology to three diseases—Hepatitis B, influenza, and respiratory syncytial virus.
I find this kind of “technology platform” that you could apply to multiple diseases particularly exciting because our work is not simply about scientific discovery. It’s about delivering effective solutions. Some of what I consider the greatest successes are grants that have led to new partnerships with the potential to turn great scientific ideas into real-world solutions.
Dr. Rafi Ahmed, an immunologist at Emory University, for example, built a partnership with Genentech, a biotech company. Ahmed and his team have shown that it is possible to reinvigorate T-cells “exhausted” from chronic viral infections such as Hepatitis C and HIV—an approach that could be applied to a therapeutic vaccine or new combination treatments.
Similarly, Richard Axel, a Nobel Prize-winning neuroscientist, and Leslie Vosshall, a scientist at The Rockefeller University, are now collaborating with Bayer CropSciences and SentiSearch to continue their research on novel compounds that block insects’ abilities to find plant or human targets. The compounds they identify could become the insect repellent of the future.
Even projects that weren't scientifically successful taught us valuable lessons. For me, investing in these projects is worth the risk. I believe that risk-taking is essential if we are to develop truly transformative health technologies. And the Grand Challenges program continues to evolve as we learn the best ways to push the envelope further. So while we will continue to support this kind of innovative research, it is important that new donors and organizations do more to fund this kind of work. I believe that projects like Baker’s, Ahmed’s and Axel’s—among many others—prove that these are challenges worth tackling.
We Have Proof
Real Lives. Real Progress.
Optimism is always in short supply, but it’s needed to sustain efforts to improve global health and support development. Fortunately, thanks to development aid, reasons for optimism abound. To help highlight them, and Melinda and I are actively involved in the Living Proof campaign.

Melinda and I are heading to London in a couple of days to thank the UK for its history of generosity and remarkable commitment to foreign aid. We want to share the proof that investments in global health and development are saving lives, improving livelihoods, and building prosperous societies.
In the last 50 years, child deaths in the developing world have been cut by more than 50 percent; polio cases have been reduced by 99 percent; measles deaths in Africa dropped by 92 percent between 2000 and 2008; and malaria cases have been reduced by 50 percent in 38 countries between 2000 and 2008. Through our work, especially our visits to the field, Melinda and I have been deeply touched by personal stories of lives changed for the better. We have seen clear evidence that targeted foreign investments are saving lives, preventing and curing disease, and helping people to lift themselves and their communities out of poverty.
Earlier this year, we transferred the Living Proof campaign to the ONE Campaign. Living Proof highlights the positive impact foreign aid is making. It aims to challenge stereotypes and misconceptions about development assistance, using a series of success stories that will galvanize support, energize activists and ultimately inspire action. With the message that effective aid in global health and development is working, the campaign will share the proof that smart aid is having a lasting impact on people’s lives and livelihoods and advancing real progress in developing countries.
ONE is expanding Living Proof to reach new audiences in more countries and to highlight the lasting impact of European investments. On October 18, the ONE Campaign is launching Living Proof in London. Both Melinda and I will be there to share stories about real lives and real progress being made around the world.
For us, these success stories have a profound impact on the way we look at our investments, and we believe that telling these stories to as many people as possible can help change the way they look at what we can achieve in the future. Together with ONE and our partners, we want to get these stories and facts out and inform the conversation around the opportunities in global health and development.
We are confident that spreading the word about what’s working is one of the most important things we can do to motivate governments and others to invest in effective development aid.
Health Affects Minds
A disturbing link: disease and intelligence
For me personally and for the Bill & Melinda Gates Foundation, improving global health is a way to fight poverty as well as to save lives. The role of health in social and economic development is highlighted by new research on infectious disease and IQ.

Central to our work in global health has been the effort to reduce infectious diseases such as diarrhea and malaria in developing countries. Because these diseases no longer affect the rich world, they haven’t received the attention they should given their truly devastating impacts on poor communities, where they’re prevalent.
Infectious diseases in developing countries are important not only because of the tragic toll they take in human lives lost, but also because of the tremendous social and economic costs associated with them.
Recently I read an article in The Economist, which looks at growing evidence that disease and intelligence are connected in ways that are pretty shocking and troubling. Although more studies are needed, the evidence makes me even more convinced that we need to get after malaria and diarrhea – and many other diseases far too common in the developing world – in a big way.
Specifically, new research by University of New Mexico researchers has found that cognitive ability (IQ) is generally lower in places where infectious diseases are widespread, i.e., poor countries.
People are just now realizing this. It’s a huge scandal and yet another reason why it’s so critically important to fight infectious disease, which takes a huge toll on people’s ability to learn and climb out of poverty.
What’s going on is that fighting off parasites and microbes associated with things like diarrhea and malaria takes away energy that the body needs for brain development. This is especially true among children and infants. Newborns use almost all their metabolic energy for their rapidly developing brains. Analyzing IQ and epidemiological data from around the world, the UNM researchers found that the burden of infectious disease plays a much bigger role in depressing IQ than other possible explanations that have been talked about.
There’s also clinical evidence. For example, research in Uganda found that children who survive cerebral malaria, which affects more than a half-million African children every year, continue to suffer significant cognitive impairments, mainly memory and attention deficit, even two years later. The Ugandan researchers found that these children can be helped by weekly sessions where they use cognitive training software on PCs. But this is an expensive, intensive and only partially effective approach to a problem that could have been prevented to begin with.
The cognitive problems created by malaria are another strong reason why our foundation has made fighting it a priority. We’re trying to help develop a safe, highly effective and affordable malaria vaccine, while also supporting efforts to improve treatment, diagnostics and other malaria control measures.
Widespread infectious disease may even impair kids who don’t get sick themselves. Adults who are ill are less productive; farmers grow less food, for example. Less food means less energy available for their kids and their kids’ brain development. An article in The Lancet medical journal estimates that because of malnutrition, poverty and poor health, over 200 million children under five years are not fulfilling their developmental potential.
In the past, some people have suggested that poor countries are poor because the people there have lower IQs. But it’s really the other way around. Poverty breeds disease, which can affect brain development, which reinforces poverty. Improving global health is a way to break this cycle.
More and Better Crops
Better farms – improved lives
With support from the foundation, six nonprofit agricultural development organizations are helping hundreds of thousands of poor farmers in Sub-Saharan Africa and South Asia grow more productive, profitable, and sustainable crops.

Three-quarters of the world’s poorest people rely on farming small plots of land to feed themselves and their families. Helping these small farmers grow more crops and get them to market can have a tremendous impact on reducing hunger and poverty and associated problems.
But it’s a complicated challenge that requires support and investments across the agricultural value chain—from cultivating better seeds and soil conditions to improving farm management, access to markets, and government policies.
In 2008, we announced $306 million in grants to six organizations to help poor farming families in Sub-Saharan Africa and South Asia boost their productivity, increase their incomes, and improve their lives. When we announced the grants, I promised to post annual updates about the projects as a way to share the progress, setbacks, and lessons of our work in agricultural development.
Looking at the 2010 updates that have just been posted to the foundation website, I’m amazed at the life-changing results that our grantees have achieved in such a short time. In the last year, these organizations have touched the lives of hundreds of thousands of farmers and they are on track to help more than 5 million farming families in the years ahead.
Highlights From the 2010 Updates
In many parts of India and Africa, small farmers rely solely on rainwater to grow their crops and can produce barely enough food for their own subsistence. International Development Enterprises (IDE) last year worked with 731 agricultural equipment dealers to make affordable small-scale irrigation systems available to more than 100,000 farmers. IDE also helped about 12,000 farmers secure microfinancing to pay for the new systems. As a result, these small-farm families have been able to produce and sell surplus crops and increase their incomes by an average of $600 per year—enough to pay for school, healthcare, and invest in their farms.
The International Rice Research Institute (IRRI) is making steady progress toward its goals of providing 400,000 farmers with heartier varieties of rice that can withstand drought, flood, extreme cold, and harsh soil conditions. IRRI has trained more than 750 scientists in rice breeding and crop management, developed more than 200 new varieties of stress-tolerant seeds, and distributed over 6,500 tons of seed to farmers in the last year. And through a process called “participatory variety selection,” IRRI gets farmers directly involved in developing rice varieties that will grow best under local conditions.
In 2009, TechnoServe used its foundation grant to help provide 67,000 small-holder coffee growers in East Africa with access to equipment that enables them to process their beans into high-quality coffee. TechnoServe also helped train thousands of farmers in sustainable agronomy practices, and how to evaluate the quality of their coffee beans.
Working in Bangladesh, CARE organized more than 15,400 dairy farmers into groups that can collectively buy better feed and receive training in animal husbandry to produce larger amounts of higher-quality milk from their cows. Largely because of a sudden drop in demand for fresh milk in Bangladesh, CARE managed to link only about 5,400 farmers—a quarter of its target—to refrigeration facilities where they could store surplus milk for sale. But the organization met its goal of deploying 120 community veterinary workers, and more than 4,400 local dairy farmers used artificial insemination services provided by CARE.
In East Africa, more than 47,000 dairy farmers received help from Heifer International to form business associations and establish chilling plants that will help get the farmers’ milk to market. Although Heifer was able only to secure financing for five new chilling plants instead of 23 as planned, the new and existing plants helped farmers sell more than 118,000 liters of milk per day, more than we had expected. Heifer also helped local breeding services perform more than 56,000 artificial inseminations and is investigating new approaches to substantially increase that number in the next two years.
In Kenya and other sub-Saharan countries, the Alliance for a Green Revolution in Africa (AGRA) is bringing affordable fertilizers and training in integrated soil fertility management techniques to farmers. Although the start of these projects was delayed in 2008 because of political unrest in Kenya and rising fuel costs, AGRA has begun to make progress in helping farmers adopt more environmentally sustainable farming practices.
The annual progress reports on these organizations enable us to see what’s been working well in each program, and to adjust our strategies to address unexpected challenges and to adapt to the evolving needs of local communities and individual farmers. I’m encouraged by the strides that our nonprofit partners and the farmers are making through these programs despite challenging conditions. At the same time, I see how much more needs to be done.
Since 2006, the foundation has committed more than $1.5 billion in grants to support agricultural development efforts. The G8 and G20 nations have committed $22 billion to food security over three years and African countries and leaders are also making big increases in their domestic investment in agriculture.
This renewed attention to agricultural development is important. We know that better farming is the most important solution for overcoming hunger and poverty, and that the investments the foundation and others are making can have an incredible impact in a relatively short period of time.
An Encouraging Visit
Nigeria advances the fight against polio
In a visit to Africa’s most populous nation, I witnessed remarkable progress against polio, with lessons for the fight against infectious diseases worldwide.

With continued hard work and investment the world is on a path toward something pretty incredible, the eradication of polio. In the past two decades, polio cases around the world have been reduced by 99 percent. If we can get rid of the last 1 percent, polio will become the second major infectious disease, after smallpox, that has ever been completely eliminated. There are still gaps in funding for polio eradication, and new outbreaks could reverse some of the progress made so far. But if polio is eliminated, never again will a child be crippled by this terrible virus.
We have a chance to get there because of some great efforts, particularly by the Global Polio Eradication Initiative, which involves the World Health Organization, Rotary International, the US Centers for Disease Control and Prevention (CDC) and the United Nations Children's Fund (UNICEF). The Gates Foundation is very involved in supporting polio immunization campaigns and other efforts to educate parents and communities about the importance of immunization. We’re also supporting work to improve polio surveillance and to develop better vaccines and anti-poliovirus drugs.
Northern India and northern Nigeria are two areas where polio continues to be a problem. I visited northern India in May this year to see the progress there. I was very excited to visit northern Nigeria in June, because the progress there since my last visit in February 2009 has been especially impressive. As of July 14th, only five cases due to wild polio viruses were reported in Nigeria this year, versus hundreds last year.
I spent most of my first day in Kano, one of the northern states most vulnerable to polio. I met with community leaders, visited a local health center and stopped in at an informal school where students study the Koran in Arabic. On the streets and most everywhere else we went, I noticed so many young children around. Nigeria has more people by far than any other African country, and more than 40 percent of them are under the age of 15. That makes polio immunization a big challenge. Kano had just begun a campaign to immunize more than 6 million children under the age of five.
Part of the challenge is overcoming fear and suspicion. In Kano in the past, false rumors linked immunization to sterility and HIV. Community leaders told me that because polio vaccine is free and brought to people in their homes, some people think there must be something wrong with it. Community leaders play a critically important role in helping to overcome mistrust, and a big focus of anti-polio efforts is on informing these leaders and enlisting their support.
Another ironic thing I noticed was that because polio cases have been dramatically reduced, it’s more difficult to know whether local immunization campaigns are reaching everyone they need to reach, particularly sub-populations that may be more at risk. Without many actual cases, you have to rely on other ways of monitoring immunization rates, and the different measures are sometimes quite inconsistent. I think we need to look at how to help get more reliable data to guide our efforts and ensure they’re effective.
Also of concern is the risk that progress against polio in Kano might be undermined by the virus filtering back in from neighboring countries and other parts of northern Nigeria. Increasingly, the problem needs to be approached on a regional basis.
The school we visited was very interesting. It didn’t really look like a school. There were no classrooms, just children sitting on the street, against a wall or under a tree, holding slates with Arabic script written on them. I asked one of the boys to recite the lesson from his slate, and he did.
That night in Abuja, the Nigerian capital, I had dinner with government officials including the Minister of Health, Onyebuchi Chukwu. It was interesting to learn about some of the creative approaches being used to inform Nigerians about the importance of immunization. Pro-immunization messages are being embedded in the plotlines of popular TV entertainment programs, for example. One of Nigeria’s largest mobile phone service providers has agreed to send out about 25 million free text messages on polio and health.
The next day I had a number of meetings including a session with several state governors and one with Nigeria’s new President, Goodluck Jonathan. Commitment from Nigeria’s leaders has been crucial in advancing the nation’s fight against polio.
A recurring theme I picked up from the people I talked to was the importance of using what we’ve learned and accomplished in the drive against polio to fight other illnesses such as infant diarrhea, respiratory ailments and malaria. I do believe that polio eradication helps strengthen routine immunization, which has the potential to save the lives of large numbers of children.
Wherever I go, I always find that saving children’s lives is a universal concern. I was very impressed with Nigeria’s progress against polio. I tried to encourage everyone to not let up.
Microbicide Trial
Exciting News for HIV Prevention
I believe that one important way to stop the spread of AIDS is by empowering women to protect themselves from infection. I'm encouraged that new research shows positive results from women using antiretrovirals for HIV/AIDS prevention.

As I mentioned in my speech to the XVIII International AIDS Conference on Monday, one promising area in the fight against HIV/AIDS is antiretroviral (ARV) -based prevention: pills, injections, and gels that contain the drugs now used for treatment.
And so it really was a privilege to be in Vienna when the incredibly exciting results of a new study were released. The Centre for the AIDS Programme of Research in Africa (CAPRISA) microbicide trial, the first of a new generation of ARV-based microbicides, showed reduced risk of HIV and herpes infections in women. This is the first time that a microbicide has been found to be effective.
What makes this so important is that we are a big step further in putting HIV prevention in the hands of women, who account for the majority of HIV infections worldwide.
The CAPRISA microbicide is a topical gel that contains tenofovir—an antiretroviral drug widely used to treat HIV infections which women in the study inserted up to 12 hours before sex and soon after having sex for a maximum of two doses in 24 hours.
The tenofovir gel was found to be 39 percent effective in reducing a woman's risk of becoming infected with HIV during sex. The study also found that the microbicide is 51 percent effective in preventing genital herpes, important because women with genital herpes are at greater risk for HIV infection. Widespread use of the gel, at this level of protection, could prevent more than half a million new HIV infections in South Africa alone over the next ten years saving many lives.
The CAPRISA microbicide trial findings are an exciting advance for HIV prevention. They give us reason to be hopeful, not just for an effective microbicide, but also for other ARV-based prevention tools now in development. As with any promising new HIV prevention tool, we look forward to discussions on how we might collaborate with other funders to support projects to confirm and extend these findings.
I’m really glad I attended the conference this year. As I said in my speech, even as we advocate for more funding, we need to be much more efficient in our approaches for treatment and prevention. But there was tremendous energy in Vienna and I am optimistic that we can push ourselves to make the most of every dollar of funding, to identify the most effective ways to save lives, and to share what we learn as widely as possible.
A Hopeful Message
A Roadmap for HIV Prevention
I traveled to Vienna to speak at the 2010 International AIDS Conference, the premier gathering for those working to prevent and treat HIV infection, which is a priority of the Gates Foundation. My message was hopeful, but advocated for changes to make anti-AIDS efforts more effective.

I’m honored to speak at the XVIII International AIDS Conference in Vienna today. This conference marks an important turning point in the fight against AIDS.
There are good reasons to be hopeful—we have seen amazing progress. The number of people getting treatment for AIDS has increased twelve-fold since 2003. The people at this conference and major partners such as the Global Fund to Fight AIDS, Tuberculosis and Malaria and PEPFAR have helped make this possible.
At the same time, we have to recognize that these are tough times for those of us who are passionate about fighting HIV. Economic turbulence has driven up government deficits, and some countries have responded by reducing their investments in global health. These are the challenges we all face, but they don’t have to define our time.
And that is why, even as we are hopeful, we have to be honest with ourselves: We don’t have the money to treat our way out of this epidemic. Even as we continue to advocate for more funding, we need to make sure we’re getting the most benefit from each dollar of funding and every ounce of effort.
If we push for a new focus on efficiency, especially in prevention, we can, over the next two decades, drive down the number of new infections dramatically.
Here’s how we can do that:
- We need to scale up existing tools, like male circumcision and preventing mother-to-child transmission.
- We need to focus prevention efforts on the communities where transmission is the highest, such as men who have sex with men, injecting drug users, and sex workers.
- We also need innovations in basic science, diagnostics, computer modeling, and our understanding of the virus itself. This would make it possible to create new weapons for our fight against AIDS, prevent even more infections, and save even more lives. Vaccines, new diagnostics, and antiretroviral-based prevention (pills, injections and gels) are some of the new tools I’m really excited about.
If we scale up existing interventions and add new tools in the hardest-hit countries, it would change the face of AIDS. New cases would plunge. Millions more could be treated. The control of HIV would stand alongside the eradication of smallpox as one of the great public health victories in history.
This is the opportunity we have. We can keep doing things the old way, and keep getting the same result. Or we can push ourselves to make the most of every dollar of funding and every ounce of effort: to identify the most effective ways to save lives, and to share what we learn as widely as possible.
If we do that, we will have matched our compassion with the growing capacities of science, and we will start to write the story of the end of AIDS.
Travels in India
Seeing self-help in action in India
I was on the road again in May 2010 on a visit to northern India. I came back excited by the progress I saw in villages that have suffered from dire poverty and the persistence of polio.

India is always a fascinating place to visit. I’ve now been there more than a dozen times. I went in July 2009 to look at the government’s efforts to improve health care in poor communities. I returned in May 2010 to see how things are going with projects that are trying to help eliminate polio and other infectious diseases, and help improve things for people in some of the poorest areas, specifically the states of Uttar Pradesh and Bihar in the north of the country.
I traveled to Uttar Pradesh with Rahul Gandhi, a member of Parliament. He has been a real innovator in organizing women’s self-help groups, and one of our first stops was a meeting of self-help group leaders. It was incredible to listen in on their discussions and hear them encouraging one another with songs and chants about vaccinations, sanitation and safe birthing practices. You could hear in their voices how they had gained optimism and confidence from their experiences working together.
These women go out to other villages and in the past three years they’ve helped form over 20,000 new self-help groups. The groups enable women to get microloans at lower rates than the moneylenders charge and work to improve services, like health and education, in their villages. I really can't express how uplifting it was to listen to these women talk about how they organized. If one woman couldn't get something to be done, then ten would show up. If that didn't work, 100 would show up. Rahul was making the point that self-help groups are a key enabler, not super expensive, with all sorts of additional benefits that contribute to our health and education goals.
I also went to Bihar, the poorest state in India, but one that’s making lots of progress. Polio is still a significant problem there, and the campaign against it is very intense. As in Utter Pradesh, self-help groups play an important role in Bihar, particularly groups organized by PRADAN, a nonprofit group of professionals who provide development assistance to India’s remotest villages whom we support through the Bill & Melinda Gates Foundation.
Among other things, PRADAN helps farmers improve their agricultural practices so they can increase their crop yields and even find new sources of income, such as by developing arjuna tree plantations for rearing silkworms and weaving silk. It was amazing to see how self-help groups aided by PRADAN expertise had completely transformed the villages we visited, keeping kids in school, encouraging girls to marry later and to take control of their family size, all things that improve the well being of their families and the village as a whole.
While in Bihar, I also met with the Chief Minister of the state. Under his leadership, Bihar has made significant progress, improving health outcomes and increasing vaccination rates. It’s really encouraging to see progress being made in one of the poorest places in India. You realize if it can happen here, it can happen almost anywhere.
My last few days were spent in India’s capital, New Delhi. I met with innovators from some of the Indian companies that make inexpensive vaccines, which are helping make vaccination more affordable for kids around the world. I also met with government officials including Prime Minister Manmohan Singh and Health Minister Ghulam Azad, whose energy and commitment were also very impressive.
So it was an uplifting trip. India has a good chance of eliminating polio in the next few years, which would be a huge achievement. And the progress being made toward many development goals is truly inspiring.
Making Medicines Available
Eliminating killer diseases with new medicines
For people suffering from serious but treatable diseases like pneumonia and tuberculosis, access to drugs can mean the difference between life and death. A new report and two recent announcements are signs of progress in efforts to expand access.

In the developed world, we sometimes take life-saving medicines for granted. But as I’ve traveled in the developing world, I’ve seen first-hand the huge difference they can make. A new report and two recent announcements are reminders of the important role of the pharmaceutical industry, especially in helping save the lives of people in poor countries.
The new report is the Access to Medicine Index 2010 from the Access to Medicine Foundation, based in the Netherlands. The index ranks 20 of the world's largest pharmaceutical companies on their efforts to make sure that medicines are made for and reach people in developing countries. The latest index found that companies are being more transparent about their efforts to expand access. They’ve also taken steps to make drug pricing more equitable and to increase R&D on diseases affecting poor countries. But in the words of the Index’s founder Wim Leereveld, “the industry as a whole still has a long way to go.”
One example of progress on access is the announcement by GlaxoSmithKline and Pfizer Inc. that they will accelerate production and distribution of new vaccines against pneumococcal disease, which kills 1.6 million people a year—mostly in developing countries, and half of them children under the age of five.
Glaxo and Pfizer will supply 30 million doses a year, for 10 years, at a price that is more affordable for developing countries. Estimates are that the vaccines could save 900,000 lives by 2015, and up to 7 million lives by 2030. Key to this effort was an innovative financing mechanism, known as an Advance Market Commitment, piloted by the GAVI Alliance. I am pleased that our foundation was able to support this effort in partnership with GAVI, the World Bank, the World Health Organization, UNICEF and the national governments of Italy, Canada, Norway, Russia, and the United Kingdom.
In another important effort supported by the foundation, the non-profit Critical Path Institute (C-Path) and the Global Alliance for TB Drug Development (TB Alliance) will coordinate testing of promising combinations of tuberculosis drug candidates from at least 11 different pharmaceutical companies early in the development pipeline.
If you used the historical approach to testing and getting regulatory approval for new TB drugs—individually and then in combination with other drugs—it could take 24 years. This new approach, which the foundation created in partnership with C-Path and the TB Alliance, hopes to develop effective new combination TB treatments in just six years. Importantly, the U.S. Food and Drug Administration and regulatory authorities in Europe have indicated strong support for accelerating approvals of safe, effective new treatments.
Although many people think of TB as a disease that was conquered long ago, it still kills 1.8 million people a year, mainly in the poorest countries on earth. The current four-drug course of treatment for TB is now 50 years old and requires patients to take numerous pills for six months or longer, which many find difficult, especially given the often-unpleasant side effects. When patients don't complete their course of treatment, the disease can become resistant to the initial drugs. In 2007, there were more than 500,000 cases of drug-resistant TB. New and easier ways to treat TB would be a great step forward.
I believe that these kinds of innovative collaborations between pharmaceutical companies, governments and the non-profit sector are critical to accelerating the delivery of medicines, which is critical to saving lives.
A Gates Foundation Trip
Simple advances, amazing benefits in Africa
On this trip to Africa, I saw simple technologies having big impacts.

In December 2009, I went to Africa on a Gates Foundation trip. It’s really helpful to get a view on the ground of work we’re doing, and to meet the people who are making it happen.
For all the benefits that modern healthcare technology has to offer, it was amazing to see how simple advances in basic sanitation and personal hygiene are making such a difference for the poor in South Africa. And in Kenya, I saw first-hand how the innovative use of cellphones and modest investments in food handling are improving people’s lives.
My trip started in Durban, South Africa, where I met with Neal Macleod, head of Durban Water and Sanitation. Neal has been a leader in thinking through how to improve sanitation for the poor in Durban. Most of us take for granted the convenience and sanitation benefits of flush toilets. But in Durban, many people don’t have access to water. So reducing the incidence of diarrheal diseases and worm infections associated with the use of pit toilets is important – especially for young children who are the most vulnerable. Neal showed me the VIP toilet – which isn’t as fancy as its name suggests, but is a breakthrough in basic sanitation through the use of simple ventilation methods and other inexpensive construction methods, such as installing a fly screen on the ventilation pipe.
After that, I travelled 590 kilometers northwest of Durban to Bophelo Pele, a male circumcision center near Johannesburg that has had incredible success demonstrating how this simple procedure can reduce—by more than 60 percent—the transmission of AIDS from women to men. I met with Professor Bertran Auvert, a French scientist, whose research also proves to skeptics that teenage and adult men are willing to be circumcised. Since the project began, more than 14,000 men have been circumcised, in a procedure that takes a doctor just 7 minutes and costs less than $40. It’s a remarkable example of how modest and wise investments can save lives and significantly reduce the financial impact of AIDS, especially in countries where the infection rate is so high.
In Kenya, I visited Eldoret, where we saw how M-PESA, an innovative cell phone service offered by Safaricom, the local telecommunications provider, is making basic financial services available to poor people. This is a big goal of the foundation, so I was excited to see how popular M-PESA has become. Everywhere I went, I saw the M-PESA logo (“pesa” is Swahili for “money”). M-PESA is an affordable, fast and safe way for people to deposit, save and transfer money anywhere in Kenya. Safaricom is now getting banks and insurance companies involved and the service is spreading to other countries.
In the nearby town of Kabiyet, I saw how an even simpler and older technology—a chilling plant—is helping improve the lives of local dairy farmers. In the past, farmers had to sell their milk within two to three hours or it would go sour. With the new chilling plant at Kabiyet Dairies Company, Ltd. (which the foundation’s grantee, Heifer International, helped finance), the milk can be properly chilled and checked for quality. Now, farmers are getting almost double the price. I met one farmer who told me that he is now able to send his kids to school because of the extra income he earns. In addition, the Kabiyet facility has become a center for a lot of other services that local farmers need, including artificial insemination of cows, veterinary services, and supplements that help dairy cows produce more milk.
Africa is home to 15 percent of the world’s population and many of its poorest citizens. While the continent faces many challenges in reaching the targets of the Millennium Development Goals, the projects I visited show how progress in reaching these goals is possible and can be accelerated. That’s why Africa is a particular focus for the foundation.
Visiting Health Clinics
Delivering health care in India
In July, I traveled to India to see how new investments by the Indian government are improving medical care in poor communities. During the trip, I visited health clinics in the state of Uttar Pradesh and saw how vaccines and other basic health care is being delivered to mothers and children.

My visit to India is a part of my ongoing efforts to see first-hand the impact of issues that people in poor rural and urban communities are facing and to assess how innovative approaches to addressing these issues are working. Look for additional videos in the future as I travel to other regions where the Bill & Melinda Gates Foundation is supporting programs in global health and development.
How to Help
We need productivity and sustainability
Helping poor farmers improve productivity is a critical step in reducing global hunger. But there is an ideological divide over how best to help them. The truth is that both sides have something important to offer.

While the World Summit on Food Security in Rome in November did not achieve all it should, it shined a welcome spotlight on small farmers who make up the vast majority of hungry and poor people in the world. Coming on the heels of a commitment by the G20 to invest $22 billion in developing-country agriculture, the summit provided reason to be optimistic that after decades of neglect, we’ll start investing in the single best strategy to reduce global hunger and poverty.
At the same time, I am worried that as momentum builds behind agricultural development as a long-term alternative to food aid, a growing ideological divide may cause the world to squander a real opportunity to fight hunger and poverty.
The global movement to help small farmers is increasingly divided into two camps. On one side is a technological approach focused on improving productivity. On the other side is an environmental approach that promotes sustainability. Productivity or sustainability – they say you have to choose.
A recent Time Magazine article “Different Shades of Green in Africa,”for example, pits the idea of organic development to help African farmers against the heavy input approach being promoted by the Alliance for a Green Revolution in African (AGRA) and the Bill & Melinda Gates Foundation, calling it “a battle between two very different agricultural philosophies.”
As I said during my speech at the World Food Prize in October, this is a false choice that is dangerous for the field of agricultural development.
At a time of rising population and climate change, we need both organic solutions that promote sustainability and the technological approaches that increase productivity—and there is no reason we can’t have them both.
Many environmental advocates highlight the excesses of the original Green Revolution. They have a point. The Green Revolution increased yields dramatically in many poor countries in the second half of the 20th century, but it also led to over-irrigation and over-fertilization. The next Green Revolution has to be greener than the first.
Some have tried to restrict the spread of biotechnology regardless of its potential to increase productivity. They act as if there is no emergency, even though there are already 1 billion hungry people in the world, and climate change is going to make conditions harsher in the future. The Food and Agriculture Organization estimates that developing countries will have to boost their yields by half to meet the challenge of global hunger. We simply won’t be able to meet that goal without using all the scientific tools at our disposal.
Of course, new technologies must be proven safe for farmers, consumers, and the environment before they’re adopted. That’s why countries should have a strong regulatory infrastructure guided by experts with access to the latest science-based information.
I have seen proof that agricultural science can make people’s lives better. This summer, I attended a roundtable discussion in New Delhi with scientists who developed a new variety of rice called Swarna-sub1. The amazing thing about Swarna-sub1 is that it can survive underwater for more than two weeks, which means it could revolutionize life for millions of farmers in flood-prone areas of India. The researchers used a fascinating technique called marker assisted selection to introduce a single allele, a version of a gene, into an existing rice variety to make it flood tolerant.
I also met with representatives from local NGOs, seed companies, and the government of India to talk about their plans for delivering new seeds to farmers. The government’s goal is to have more than 5 million hectares planted with Swarna-sub1 in just five years.
The tendentious debate pitting productivity against sustainability doesn’t just threaten important scientific advances. It also obscures another crucial lesson from the first Green Revolution: that developing more productive seeds is just one element of an effective strategy. In addition to new seeds, farmers also need training, access to new markets, and organizations to represent their interests. Governments need better data so they can devise sound agricultural policies. By placing so much emphasis on just one link in a very long agricultural value chain, we distract ourselves from a goal we can all agree on: helping small farmers and their families.
Success requires progress on many fronts. African countries must lead the way by spending more on agriculture. Donor countries must do a better job of listening so they can understand what poor countries really need. They should explain more clearly how the money they’re pledging will be spent. I am optimistic that these obstacles can be cleared away and that the world can tap into the opportunity offered by agricultural development. That’s why the Bill & Melinda Gates Foundation has committed more than $1.4 billion to initiatives that support small farmers.
However, if the field doesn’t move past this counterproductive debate, hungry and poor people will suffer. We have a choice: We can let our disagreements get in the way of real progress, or we can agree to help more than a billion people live healthier, happier lives.