Disease atlas
These maps could point the way to stopping malaria
We’re using them to maximize scarce resources.

It’s Mosquito Week again on the Gates Notes. This year I’m exploring some of the science behind malaria and other mosquito-borne diseases. You can read below about how maps are revolutionizing the fight against malaria. I’ve also written about how the malaria parasite is a clever shapeshifter and how genetically editing mosquitoes could help us defeat the disease.
Imagine calling the fire department and telling them: “There’s a house burning somewhere in the city!” They ask you for the address or at least some nearby streets, but you’re not sure. Without more specifics, it’s just about impossible for them to help.
For decades, the malaria community has faced a similar problem, but on a national scale. In many of the countries with a lot of malaria, we have had a national estimate of how prevalent it is, but very little reliable information about the breakdown within the country. That means health officials have to distribute bednets across an entire region, hoping to get everyone who might be at risk while also covering people who aren’t.
This problem is especially urgent now. After more than 15 years of steady progress against the disease, the improvement is slowing down. Funding for malaria has also flatlined. If we simply stick with the same tools and the same strategies, progress will stall, and the disease might make a comeback. We need to do more with what we have.
I am happy to report that things are changing, thanks to better data. A combination of new technology and improved systems is helping us target lifesaving interventions in the places where there’s the greatest risk of malaria—making sure that each dollar spent has the biggest possible impact.
I admit that data isn’t as sexy as shapeshifters or the X-shredder. Yet the topic is super-important. It is a big focus for our foundation’s malaria strategy, one of the key things we bring to the table given our interest in technology and innovation. This post will get more in-the-weeds than I usually do on TGN, but if you are as obsessed with malaria as I am, I hope you’ll find it interesting.
Health experts estimate the burden of disease in two ways. One is to use anonymous information collected by health workers. But this information has a lot of gaps and gets aggregated as it moves up the chain from the clinic to the district to the province. This would be roughly equivalent to adding up the cases in every hospital in a U.S. state and only reporting the total. It obscures a ton of local variation, and by the time all the data is processed, the report may be a year out of date.
The other source is surveys. Health workers go out to a community and test a few volunteers for malaria, then repeat this at sites across the country. But this process is expensive and time-consuming, which limits the number of samples a country can take and how often it can take them.
The malaria community is tackling the problem in two ways. A nonprofit called the Malaria Atlas Project (funded by our foundation) started by gathering all the data they could find from every endemic country. They discovered something surprising: Although there were big gaps on the map where we had very little information, overall there was a lot more data than anyone expected.
Using the information they had, along with data on local conditions that affect the spread of malaria (such as the temperature, humidity, and the location of health clinics), MAP started building computer models that give us a much clearer picture of what’s going on.
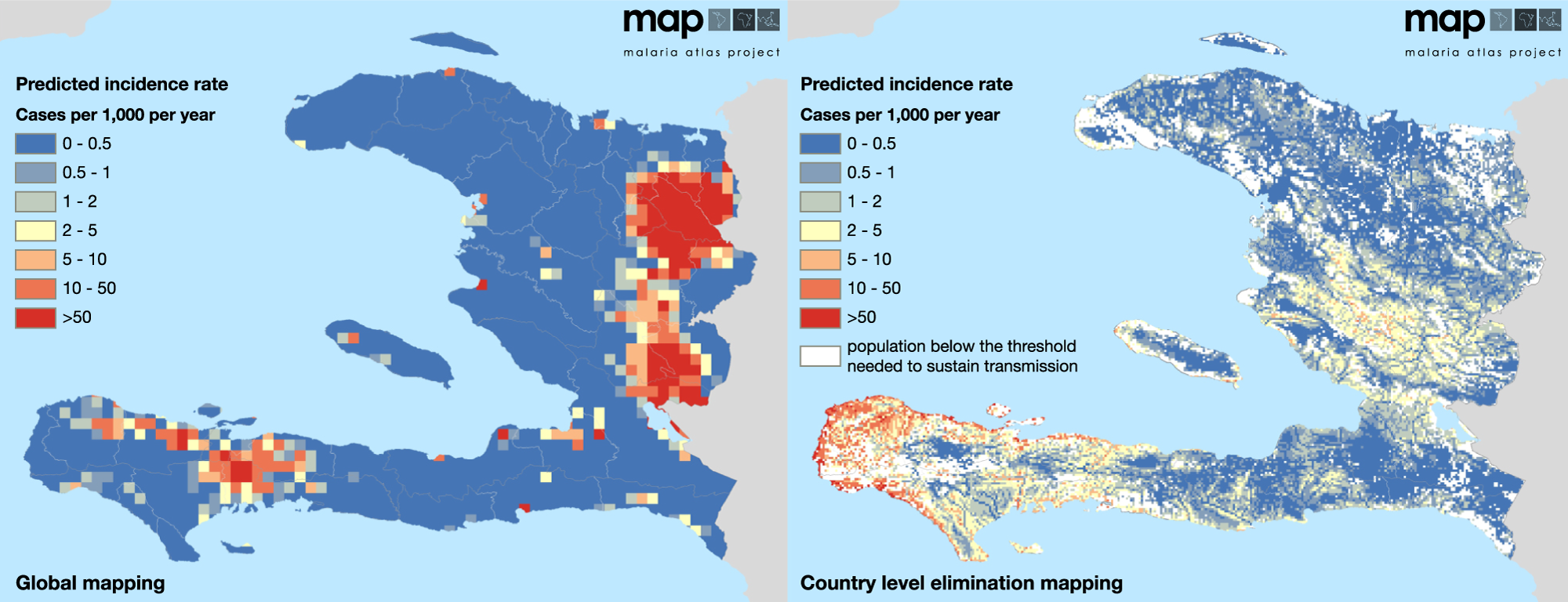
The results are remarkable. We now have data-rich maps with pixels that are just 5 km square. Instead of blanketing entire regions with bednets and other anti-malaria measures, health officials can target efforts where they will do the most good.
Now comes the next step: getting even better data so we make maps with an even higher resolution. To accomplish this, our foundation and other partners are helping countries strengthen their systems for monitoring disease. In the poorest places, this might mean disaggregating their data and making sure it is accurate and timely. For others, it means equipping health workers with mobile phones or tablets so they can enter the information digitally. More than 60 countries already use the same software to report health data, vastly simplifying the process of collecting and analyzing information.
Below you can see a dramatic example of what the future of mapping looks like. Both are maps of Haiti. The one on the left uses the 5x5 km resolution, built with aggregated data. (Remember, this was already a huge leap forward from national estimates.) The one on the right uses data from individual health facilities to create pixels that are just 1x1 km square. See how much more detailed it is? When you need to maximize scarce resources, this kind of information is invaluable.
There is more to come. One promising approach uses genetic analysis of the malaria parasite to make the maps even more robust, for example revealing how the disease is transmitted from place to place.
Genetic data is also helping us identify insecticide-resistant mosquitoes and drug-resistant forms of the disease. In Vietnam, health officials recently noticed an alarming spike of cases in one region of the country. Then genetic analysis of the parasite in that region revealed that they were fighting a drug-resistant strain of malaria. They quickly switched to a more effective drug and expect to see the number of cases drop soon.
This kind of work is best done at the local level. So we’re funding programs that help scientists in developing countries do more of this analysis themselves, rather than sending samples off to a lab in the U.S. or Europe. Increasingly, scientists in Senegal, Thailand, and other countries are doing their own analysis, which both speeds up the process and puts local experts in the leading role where they belong.
There is a lot of innovation in the malaria field right now, including work on vaccines and other parasite-killers and a way to fight the disease using test-tube mosquitoes. Better data and malaria maps will help us put all these breakthroughs to their best use, and bring us closer to the day when this disease is gone forever.