Reasons for hope
Welcome to the next phase of the Alzheimer’s fight
I am blown away by how much we have learned about Alzheimer’s disease over the last couple years.

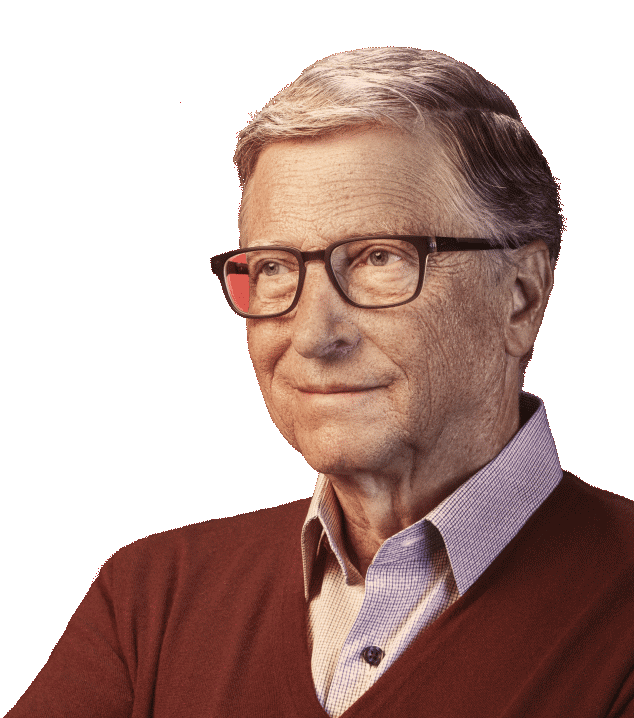
Father’s Day without my dad never gets easier. Although he is on my mind every day, I always find myself thinking about him even more often this time of year.
My dad was a giant in every sense of the word. More than anyone else, he shaped the values of the Gates Foundation, and everything we have accomplished is a testament to his vision of a better world. Sadly, we lost my dad five years ago to Alzheimer’s disease. It was a brutal experience, watching my brilliant, loving father go downhill and disappear.
In the years since his passing, I’ve met far too many people who had similar experiences with their own loved ones. More than 7 million people in the United States are currently living with Alzheimer’s disease. That means about 1 out of every 9 people over the age of 65 have it. As life expectancies continue to go up, those numbers will only increase.
But here’s the good news: We are making massive progress in the fight against Alzheimer’s and other related dementias.
I saw some of the reasons for optimism firsthand during a visit to Indiana last year. I met with the team at Indiana University’s School of Medicine in Indianapolis—where they have an incredible center that is doing lots of leading-edge neuroscience—and took a super cool tour of their biomarker labs. I also got the opportunity to look under the hood of new automated machines that will soon be running diagnostics around the world. It’s an exciting time in a challenging space.
During my visit, I learned more about the latest big breakthrough in Alzheimer’s R&D: blood-based diagnostic tests. A number of different companies have approaches in the pipeline, but each of them works in roughly the same way by detecting the ratio of amyloid plaques in the brain. I’m optimistic that these tests will be a gamechanger. Here in the U.S., this work reached a huge milestone last month: The FDA approved the first blood-based test for patients 55 years and older.
Until recently, the only way to confirm a suspected Alzheimer’s diagnosis was to get either a PET scan or a spinal tap. Neither were the kind of test a doctor would order unless you were showing clear signs of decline. But catching Alzheimer’s early is key. We now know that the disease begins 15-20 years before you start to see any signs. A simple, accurate, and easy-to-run blood test might one day make routine screening possible, identifying patients long before they experience cognitive decline.
When I talk to people about the promise of these new diagnostics, I’m often asked, “What is the point of getting diagnosed if I can’t do anything about it?”
It’s a fair question—but soon it will be moot. The FDA has approved two drugs for the treatment of Alzheimer’s. Both have proven to modestly slow down the progression of the disease, but what I’m really excited about is their potential when paired with an early diagnostic. My main takeaway from my visit to Indiana is that these treatments could be drastically more impactful than I initially thought when given early in the disease’s progression.
Phase III clinical trials are underway now to prove just how transformative these drugs are for people with presymptomatic Alzheimer’s, and we could see results as soon as 2026. Until then, the drugs will continue to help patients who are already showing cognitive decline.
I’m also optimistic that researchers will continue to improve current treatments and develop new drugs. This will require running lots of clinical trials. Without a simple diagnostic test, it is often difficult to find enough eligible patients. In some cases, it takes even longer to enroll participants—as long as three years!—than to conduct the study. My hope is that the new blood tests will get the recruitment time down to less than a year.
All of this progress hinges, of course, on continued funding for Alzheimer’s research. Some of the biggest breakthroughs to date were supported by federal grants, like the discovery of the connection between amyloid proteins and the disease. This isn’t unusual: Medical R&D often relies on government funding to support projects that explore foundational science or aren’t commercially viable yet.
We are on the cusp of turning the tide against dementia—which makes this an especially bad time to pull back on research. Recent cuts to the National Institutes of Health and other government institutions threaten to stop progress in its tracks, and no individual or private organization can fill the gap.
This is the moment to spend more money on research, not less. Right now, all over the world, researchers are collecting data about Alzheimer’s disease. New tools are making it easier for them to share information and work together. As a result, the quest to stop Alzheimer’s has never had more momentum. For my part, I worked with a coalition of partners to create the Alzheimer’s Disease Data Initiative and the Global Research and Imaging Platform, and I am proud to support organizations like the ADDF's Diagnostics Accelerator and Part the Cloud. All of these efforts simplify how researchers and data scientists work together to share data and develop algorithms and tools in order to make advances in the field.
There is still a huge amount of work to be done—like deepening our understanding of the disease’s pathology and developing even better diagnostics. But I am blown away by how much we have learned about Alzheimer’s over the last couple of years.
When we lost my dad, an Alzheimer’s diagnosis was a death sentence. Just five years later, that is finally starting to change. I cannot help but be filled with a sense of hope when I think of all the progress being made on Alzheimer’s, even with so many challenges happening around the world. We are closer than ever before to a world where no one has to watch someone they love suffer from this awful disease.