Handling coronavirus
How to respond to COVID-19
And prepare for the next epidemic, too.

In any crisis, leaders have two equally important responsibilities: solve the immediate problem and keep it from happening again. The COVID-19 pandemic is an excellent case in point. The world needs to save lives now while also improving the way we respond to outbreaks in general. The first point is more pressing, but the second has crucial long-term consequences.
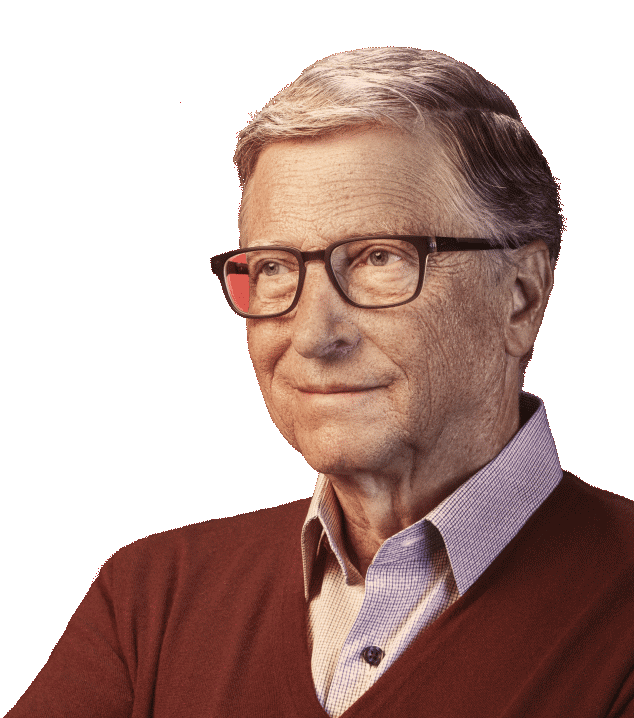
The long-term challenge—improving our ability to respond to outbreaks—isn’t new. Global health experts have been saying for years that another pandemic rivalling the speed and severity of the 1918 influenza epidemic wasn’t a matter of if but when. The Bill & Melinda Gates Foundation has committed significant resources in recent years to helping the world prepare for such a scenario.
Now, in addition to the perennial challenge, we face an immediate crisis. In the past week, COVID-19 has started to behave a lot like the once-in-a-century pathogen we’ve been worried about. I hope it’s not that bad, but we should assume that it will be until we know otherwise.
There are two reasons that COVID-19 is such a threat. First, it can kill healthy adults in addition to elderly people with existing health problems. The data so far suggests that the virus has a case fatality risk around 1%; this rate would make it several times more severe than typical seasonal influenza and would put it somewhere between the 1957 influenza pandemic (0.6%) and the 1918 influenza pandemic (2%).
Second, COVID-19 is transmitted quite efficiently. The average infected person spreads the disease to two or three others. That’s an exponential rate of increase. There is also strong evidence that it can be transmitted by people who are just mildly ill or not even showing symptoms yet. This means COVID-19 will be much harder to contain than Middle East Respiratory Syndrome or Severe Acute Respiratory Syndrome (SARS), which were only spread by those showing symptoms and were much less efficiently transmitted. In fact, COVID-19 has already caused 10 times as many cases as SARS in just a quarter of the time.
The good news is that national, state, and local governments and public health agencies can take steps over the next few weeks to slow the spread of COVID-19.
For example, in addition to helping their own citizens respond, donor governments should help low- and middle-income countries prepare for this pandemic. The health systems in many of these countries are already stretched thin, and a pathogen like coronavirus can quickly overwhelm them. And poorer countries have little political or economic leverage, given wealthier countries’ natural desire to put their own people first.
By helping countries in Africa and South Asia get ready now, we can save lives and also slow the global circulation of the virus. (A significant portion of the commitment Melinda and I recently made to help kickstart the global response to COVID-19—which could total up to $100 million—is focused particularly on developing countries.)
The world also needs to accelerate work on treatments and vaccines for COVID-19. Scientists were able to sequence the genome of the virus and develop several promising vaccine candidates in a matter of days, and the Coalition for Epidemic Preparedness Innovations is already preparing up to eight promising vaccine candidates for clinical trials. If one or more of these vaccines proves safe and effective in animal models, they could be ready for larger-scale trials as early as June. Drug discovery can also be accelerated by drawing on libraries of compounds that have already been tested for safety and by applying new screening techniques, including machine learning, to identify antivirals that could be ready for large-scale clinical trials within weeks.
All these steps would help address the current crisis. But we also need to make larger systemic changes so we can respond more efficiently and effectively when the next epidemic arrives.
It’s essential to help low- and middle-income countries strengthen their primary health care systems. When you build a health clinic, you’re also creating part of the infrastructure for fighting epidemics. Trained health care workers not only deliver vaccines; they can also monitor disease patterns, serving as part of the early warning systems that will alert the world to potential outbreaks.
The world also needs to invest in disease surveillance, including a case database that is instantly accessible to the relevant organizations and rules that require countries to share their information. Governments should have access to lists of trained personnel, from local leaders to global experts, who are prepared to deal with an epidemic immediately, as well as lists of supplies to be stockpiled or redirected in an emergency.
In addition, we need to build a system that can develop safe and effective vaccines and antivirals, get them approved, and deliver billions of doses within a few months of the discovery of a fast-moving pathogen. That’s a tough challenge that presents technical, diplomatic, and budgetary obstacles, as well as demanding partnership between the public and private sectors. But all these obstacles can be overcome.
One of the main technical challenges for vaccines is to improve on the old ways of manufacturing proteins, which are just too slow for responding to an epidemic. We need to develop platforms that are predictably safe, so regulatory reviews can happen quickly, and that make it easy for manufacturers to produce doses at a low cost and a massive scale. For antivirals, there will need to be an organized system to screen existing treatments and candidate molecules in a swift and standardized manner.
Another technical challenge involves constructs based on nucleic acids. These constructs can be produced within hours after a virus’s genome has been sequenced; now we need to find ways to produce them at scale.
In addition to these technical solutions, we’ll need diplomatic efforts to drive international collaboration and data sharing. Developing antivirals and vaccines involves massive clinical trials and licensing agreements that would cross national borders. We should make the most of global forums that can help achieve consensus on research priorities and trial protocols so that promising vaccine and antiviral candidates can move quickly through this process. These platforms include the World Health Organization R&D Blueprint, the International Severe Acute Respiratory and Emerging Infection Consortium trial network, and the Global Research Collaboration for Infectious Disease Preparedness. The goal of this work should be to get conclusive clinical trial results and regulatory approval in three months or less, without compromising patients’ safety.
Then there is the question of funding. Budgets for these efforts need to be expanded several times over. Billions more dollars are needed to complete Phase III trials and secure regulatory approval for coronavirus vaccines, and still more funding will be needed to improve disease surveillance and response.
Why does this require government funding—can’t the private sector solve this on its own? Pandemic products are extraordinarily high-risk investments, and pharmaceutical companies will need public funding to de-risk their work and get them to jump in with both feet. In addition, governments and other donors will need to fund—as a global public good—manufacturing facilities that can generate a vaccine supply in a matter of weeks. These facilities can make vaccines for routine immunization programs in normal times and be quickly refitted for production during a pandemic. Finally, governments will need to finance the procurement and distribution of vaccines to the populations that need them.
Obviously, billions of dollars for anti-pandemic efforts is a lot of money. But that’s the scale of investment required to solve the problem. And given the economic pain that an epidemic can impose—just look at the way COVID-19 is disrupting supply chains and stock markets, not to mention people’s lives—it will be a bargain.
Finally, governments and industry will need to come to an agreement: During a pandemic, vaccines and antivirals won’t simply be sold to the highest bidder. They’ll be available and affordable for people who are at the heart of the outbreak and in greatest need. Not only is this the right thing to do, it’s also the right strategy for short-circuiting transmission and preventing future pandemics.
These are the actions that leaders should be taking now. There is no time to waste.
This post originally appeared on the website of the New England Journal of Medicine. I wrote there about the need for a global pandemic response system in 2015, and about the threat posed by a novel respiratory virus in 2018.