Be Prepared
Annual Letter: A health emergency
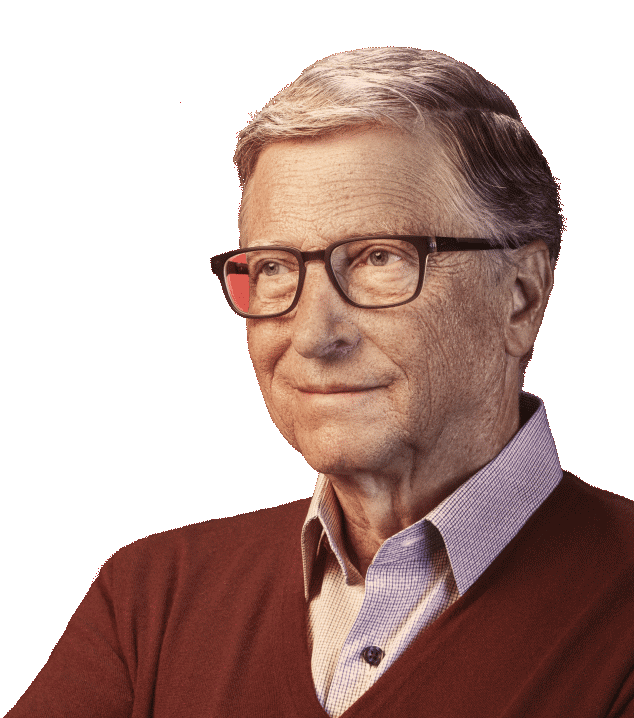
I’m willing to be seen as a troublemaker by people who are happy with the status quo on global health.

Malaria: Progress on Multiple Fronts
The fight against malaria is making very good progress. The death toll, overwhelmingly of young children in Africa, went down from 985,000 in 2000 to 781,000 in 2009. Of the 99 countries with malaria, 43 have decreased cases of the disease by more than 50 percent. Turkmenistan and Morocco were recently declared malaria-free. For these communities the reduction in both death and sickness makes a huge difference. And it is possible only because of increased donor spending, which reached $1.5 billion in 2009.
The Roll Back Malaria group, with strong support from the WHO and our foundation, has set an aggressive goal to provide bed nets to almost every household that needs them in the next few years. As coverage goes up from its current level of 42 percent, it will have a dramatic impact. In Senegal, where 80 percent of households own a bed net, the number of malaria cases went down 41 percent in a single year. Many amazing grassroots groups are helping with the delivery of bed nets. The Nothing But Nets campaign, for example, has gotten hundreds of thousands of individual citizens and organizations like the United Methodist Church and the National Basketball Association involved in the fight against malaria.
We are also working on lowering the cost of the anti-malaria drugs containing artemisinin, which are expensive enough that people are still using less effective drugs instead. The approaches range from breeding the plant that provides artemisinin to have a higher yield, to using very advanced synthetic chemistry that can make artemisinin starting with simple sugars.
As is the case with all infectious diseases, the ultimate tool against malaria would be a low cost, highly effective vaccine. The RTS,S vaccine, developed in partnership with the pharmaceutical manufacturer GSK, is in its final phase-3 trial stage. Interim data will be available later this year, and we should have final results by 2015. A number of other vaccine candidates that might be even more effective or might be combined with RTS,S are also making progress, and several will start human trials this year.
Saving the Youngest Children
Of the 8.1 million deaths per year of children under the age of 5, over 40 percent happen in the first 28 days of life, or the neonatal period. The good news is that we are headed in the right direction. In 1995 there were an estimated 5.6 million neonatal deaths. The most recent estimates show the number down to around 3.6 million.
Unlike the deaths that take place after a child is 28 days old, almost all of which can be prevented by inventing and delivering vaccines, reducing these early deaths requires a range of approaches. Some require new tools such as an ointment for the baby’s skin that prevents infection and an antibiotic solution for cleaning the cut umbilical cord. However, many of the key interventions involve social and behavioral change. You can have a huge impact (on both newborn and maternal health) by increasing the number of births done by a skilled provider in a clinic. It’s also important to teach mothers to wash their hands before handling a baby, to have frequent skin-to-skin contact with their babies, and to breastfeed exclusively for the baby’s first six months. (Mother’s milk contains not only key nutrition but also antibodies that block infection until the baby’s immune system is ready to operate on its own.) Where all of these elements come together, neonatal deaths can be reduced by 50 percent or more, so it’s critical that we learn more about how to teach and motivate mothers effectively, especially at a large scale.
Melinda has been a strong leader on maternal and child health issues. She gave an especially powerful speech last year to the Women Deliver conference. The plight of mothers and their babies is something she feels deeply, and it’s something we talk about a lot.
When she came home from a trip to Malawi she shared the experience of seeing two babies in a hospital in the town of Lilongwe, lying side-by-side in the same incubator. They were born within hours of each other. Each had suffered the same condition—they were unable to breathe at birth. Sadly, it was clear that only one would survive. That baby’s mother had made it to the donor-funded hospital in time for her delivery and was able to get the care she needed. Her baby was immediately resuscitated, which saved his life. The other was not so fortunate. He was born on the way to the clinic, on the side of road, and was not resuscitated soon enough. I wish everyone had a chance to experience what Melinda did, so they could see how things are improving but also understand the urgent need to do more.
HIV/AIDS and the Need for Leadership
Progress continues in fighting the AIDS epidemic, but the pace is slow. The rate of HIV infection has been reduced by almost 20 percent over the last 10 years, to fewer than 2.7 million infections per year. The number of people dying from AIDS has gone down by more than 20 percent in the last five years, to fewer than 2 million annually. Given all the lives that are at stake, I am impatient enough about this that I am willing to be viewed as a troublemaker by people who are happy with the status quo.
The war against AIDS is being waged on two fronts—treating those who are already infected and preventing new infections. Treatment continues to be scaled up, with more than 5 million people receiving HIV drugs. This is a great success story. Rich country generosity has been crucial and the execution in poor countries has been strong. However, there will not be enough money to treat everyone who will become infected if we don’t halt the progress of HIV. Because we don’t have a cure for AIDS, treatment has to continue for a patient’s entire life. That means costs continue to increase as you put more and more people on treatment.
Even without including people who will become infected in the future, the cost of treating the 33 million people living with AIDS today would be over $40 billion per year at current costs—over four times as much as is provided in aid today. To minimize the funding gap we need to reduce per patient costs of treatment. Drug costs have already been reduced to less than 20 percent of treatment costs. Most of the future savings will have to come from treatment models that reduce personnel, laboratory, and overhead costs. The difficulty of funding treatment makes it clear how important it is to prevent new cases. The sooner we make progress the better. There needs to be a sense of urgency that doesn’t exist yet.
Prevention breaks down into several different areas. The easiest should be preventing mother-to-child transmission since it simply involves giving a mother drugs to prevent transmission to her child. There is a lot of focus on getting from the current number of over 300,000 infections per year to zero. Another prevention approach is counseling people to change their behavior, including avoiding risky acts and using condoms. Then we have prevention approaches that rely on new tools. We now have three tools that have shown significant impact. The first is male circumcision, which I discussed last year. Amazingly, teenagers in communities with high HIV incidence show a high willingness to be circumcised. Kenya is leading the way with over 200,000 circumcisions performed. However, there are over 10 million men in high-risk settings in Africa who would benefit from male circumcision, and we should be scaling up 10 times faster than we are.
Another new tool is a vaginal microbicide gel that a woman can use to protect herself. A recent trial showed a gel containing tenofovir protected women against infection. Now the question is how long it will take before the gel is rolled out on a large scale. As someone outside the field, I am surprised at the number of steps it takes. First the product has to be licensed, which requires approvals from regulatory groups in both the country where the product will be used and donor countries. Many of these approval steps happen serially rather than in parallel, and it is only when the entire approval process is complete that the product can be rolled out. Even then the process isn’t complete because a whole system for delivering the product needs to be put together, and again a lot of these steps proceed in a slow serial fashion.
Another new prevention tool, PrEP (Pre-Exposure Prophylaxis), involves someone without HIV taking an anti-HIV drug on a regular basis to block infection. A PrEP trial showed a strong prevention benefit for the participants who consistently used the drugs and a weaker impact when all the participants were included. With both microbicides and PrEP I think countries with large epidemics should figure out how to do large community trials as soon as possible. This would shorten the time before all patients have these lifesaving tools by many years.
If the United States had an epidemic where almost half the girls in large neighborhoods contracted a terrible disease, we would find a way to cut through all the complexity. With HIV it is more difficult since there are many countries involved. But we need to work creatively to shorten these delays.
The best tool would be a vaccine for HIV. The scientific progress on this has gone well. The positive results of the trial in Thailand were a turning point for the field, and blood samples from the volunteers are being studied in depth for lessons about why that vaccine worked but only to a limited degree.
There has also been an explosion in the discovery of antibodies that block HIV infection. Scientists don’t yet know how to make a vaccine that will cause patients to generate lots of these antibodies, but there are several approaches that look promising and will be ready to go to trials in the next few years.
In order to get a fully effective HIV vaccine we will almost certainly need several rounds of trials where we learn and improve the candidate vaccines. So to get a vaccine as soon as possible we need to minimize the length of the trials and the time between trials. So far each cycle has taken over five years. The field needs to look into how to shorten this so that progress matches the urgency of the problem.