Calculated risk
A bet on humanity worth every dollar
The story behind one of the riskiest ventures our foundation has ever attempted.

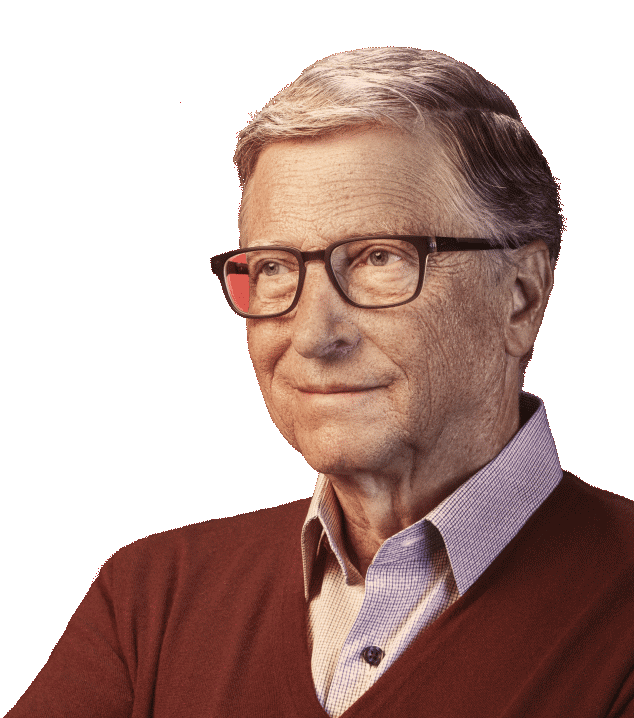
In Part 2 of the Netflix documentary series Inside Bill’s Brain, the director notes that my analytical approach to my job isn’t particularly inspiring. He’s got a point. I describe what I do as “optimization”—a wonky way of saying I try to make sure our limited resources help as many people as possible. I’ll never be the intrepid health worker on the front lines fighting disease. But if our foundation and its partners can help that worker reach more children with better tools, we all can create better lives for generations to come. Our decision to fight polio is one of the best examples.
In 2007, our foundation joined a decades-long effort to eradicate polio. We made our first big grants for what we thought would be a five-year, final push to end polio, a disease that had terrorized the human race for thousands of years. Over a decade later we are still pushing. Risky bet? Yes, but I think we were right.
The Netflix documentary talks a lot about my willingness to dive into projects, like polio eradication, where there’s no guarantee of success. In the second episode, my friend Bernie describes me as a risk taker, making his point with a story that involves a surfboard, a volcano, and a dislocated shoulder.
Watching the series got me thinking about what the word “risk” really means. In the polio fight, the risk takers are the thousands of health workers and volunteers braving war zones and getting to some of the hardest-to-reach places on earth to deliver vaccines to kids. They are the heroes of polio eradication.
The risks I take are more like what Warren Buffett does when he makes an investment on the bet that it will be worth ten times as much down the road. Warren spends a lot of time looking for a company that has great long-term prospects. Then he makes a big investment and holds it for many years. He’s famous for staying the course through market gyrations and economic cycles.
Our foundation isn’t after financial gain, but we’re aiming for similar ten-fold returns in social impact—in people living better-educated, more productive, longer and healthier lives. Like Warren, Melinda and I pick our areas of focus carefully. Whether we invest $100,000 or $100 million, the decision is always calculated. I spend a lot of time thinking, analyzing data, and talking to experts to judge whether we can really help make a difference. It’s the part of my job I love the most. I’m never happier than when I’m diving deep into the details of a problem, to understand how any proposed solution would work—or fail.
I also feel pressure to make every dollar and every day count. Warren gifted our foundation his wealth to make the world better, and Melinda and I feel a lot of responsibility to use that gift wisely. I say no to a lot more opportunities than I say yes to.
Ultimately, no matter how much analysis we do, I have to be comfortable with a lot of uncertainty. We are tackling problems where progress is measured not just in years but often decades—where your end goal doesn’t change, but your path to get there might have to. The trick is to do whatever I can to keep learning and to be open to new and novel ways to bring us a step closer to our goals. That approach has guided every big bet I’ve made in my career from Microsoft to today—including polio.
In the spirit of the title of the documentary, here’s a look at what I was thinking when we took that bet and set our foundation on one of the riskiest ventures it’s ever attempted.
I had a model in my mind: smallpox, the only human disease ever successfully wiped out. Smallpox was one of humanity’s big killers—at least 300 million people died of it in the 20th century alone. But by 1980, the disease was gone, thanks to a concerted push by global health organizations and thousands of dedicated health workers. That’s one of the greatest achievements of our age.
Early on, Melinda and I were lucky to work with Bill Foege, a key architect of that feat. He made it clear to me why eradicating a disease is a gift to all future generations. People are freed forever from a deadly threat, while the resources that were devoted to fighting that disease are freed up for solving other problems. Plus, victory is energizing: the defeat of smallpox helped inspire a global push to raise vaccination rates and lower childhood mortality. Such benefits, Bill Foege said, can make eradication “the ultimate return on investment.”
Galvanized by the smallpox success, health ministers from United Nations member states came together in 1988 and targeted polio as the next disease to go. They formed the Global Polio Eradication Initiative (GPEI)—a partnership that includes WHO, Rotary International, UNICEF and CDC.
Polio can wither limbs, paralyze lungs, and even kill. There is no cure. And yet we’ve long had the means to prevent the disease: with a cheap, safe, easy-to-administer vaccine. When the GPEI started running vaccination campaigns in 1988, polio was paralyzing 350,000 people a year. By 2007, there were only about 1,300 cases—but progress had stalled, raising the risk that the virus would surge back, and decades of gains would be lost. At the time, I was soaking up everything I could on eradication, its history, science, and epidemiology. I had only seen one polio vaccination campaign (in India) so I planned more trips.
Bill Foege and others at the foundation put together a team and we walked through the possible advances that could help us break through. Polio travels with stealth; nine out of ten people who are infected develop mild symptoms, if any, but can still spread the virus to others. So to stop it, you have to reach nearly every child with multiple doses of the vaccine over time.
That takes money and organization; it requires political cooperation and parents who trust the process and are willing to have their children be immunized. It takes an army of volunteers and trained health workers who can be counted on to knock on doors throughout a village in search of every last child and keep accurate records of who they immunized and who they missed. Stopping polio requires scientists and trained people on the ground watching out for reports of children whose limbs become abruptly paralyzed. None of the countries where polio remained in 2007 had all the pieces needed to complete that puzzle. That was the challenge, but also where we saw opportunities.
We bet that with innovations including better disease surveillance and improved mapping, we could get a clearer picture of where the virus was hiding, and that computer models could better predict where it might go. We saw ways to increase the number of vaccination campaigns and improve their quality. Deploying precise genetic tests to sample sewage could help us track the travels of different strains of the virus in the environment before it paralyzed children.
We spent about six months studying the problem and then dove in. Back then I was sure we’d be done with polio by now.
Ten years have taught us a lot. For all the great technologies and fresh ideas about how to stop polio, the real test is how they play out on the ground—in the villages and clinics of the last few countries where the disease has dug in. Unfortunately, in some places, these last steps to eradication have been slowed by risks that I underestimated, including war and political unrest. But in far more places, we’re beating the disease, as people, from parents to presidents, commit to the hard work of ending polio.
As of 2011, polio was completely gone from India, a country that experts thought would be the last place to wipe out the virus because of its size, complexity and the fact that tens of millions of its citizens live in extreme poverty. The children most at risk were in underserved, inaccessible regions, where they were often missed because of their families’ frequent moves in search of work. But leaders at all levels of government made it a priority to find those children—setting up vaccine booths in train stations, sending out vaccinators on motorbikes, boats and donkeys—and halt the disease.
In Nigeria, both traditional religious leaders and local, state and federal officials have been instrumental in building community trust in the polio program, ensuring parents allow their children to be immunized, and strengthening the quality of the vaccination campaign. It’s commitment like this that has enabled Nigeria to reach three years without a single case of wild poliovirus, which means Africa could be certified wild polio-free in 2020. This is unprecedented progress.
Global cases of wild polio this year have ticked up from the 33 cases last year, and no doubt we’ll face new challenges as we focus on Afghanistan and Pakistan, the two remaining countries where the virus has yet to be stopped. The job is to keep moving forward, adjusting to the unexpected with new ideas and energy so we can reach the last unprotected child and achieve a polio-free world. That’s a bet worth every dollar.