Abundant air
Breathing new hope into Africa’s fight against COVID-19
In Africa’s battle against COVID-19, a Kenyan doctor is making sure every breath counts.

As the COVID-19 pandemic spreads across Africa, hospitals across the continent face shortages of essential medical supplies needed to treat the respiratory disease and keep patients alive.
Not just masks and ventilators, but oxygen.
For people living in wealthy countries, medical oxygen is often taken for granted. In many low-income countries, however, oxygen is often in short supply or not available at all. And globally, a lack of oxygen –needed to treat pneumonia, malaria, and other diseases—leads to hundreds of thousands of deaths each year.
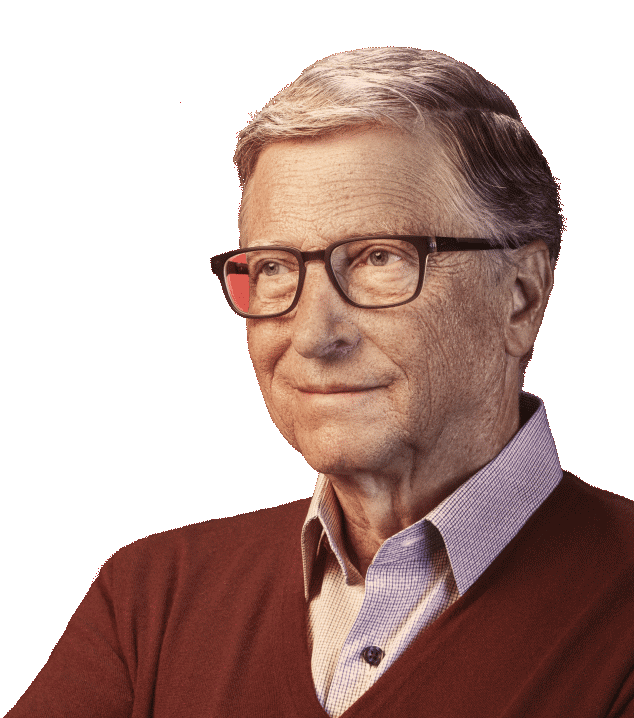
Addressing this often overlooked challenge is the life’s work of Bernard Olayo, a Kenyan doctor who founded Hewatele, an innovative organization working to ensure all patients—even in remote areas of the country—have access to oxygen.
Now, he is playing a critical role in Kenya’s preparations to tackle COVID-19 by scaling up oxygen supplies that will be needed to keep the most critically ill patients alive.
While the number of COVID-19 cases in Africa remains low compared to other parts of the world, the continent is bracing for a surge of infections. According to the World Health Organization, up to 190,000 people could die of COVID-19 in Africa if the disease is not controlled. A widespread outbreak would flood many of Africa’s fragile health systems.
A lot of attention has been focused on the lack of ventilators in Africa. Ventilators are the mechanical devices that help patients breathe, pushing air in and out of their lungs, when they can’t on their own. And the shortage of them is a real problem. But the lack of oxygen itself is equally worrying. The coronavirus attacks the respiratory tract, inflaming the lungs and making it difficult for patients to breathe. Oxygen, delivered through a mask or nasal tube, is an essential and effective first line of treatment that’s less invasive than being on a ventilator. Oxygen is also needed to run a ventilator. If COVID-19 patients have access to oxygen as an initial treatment, however, it may prevent many of them from becoming so critically ill that they would require one of the limited number of ventilators to breathe.
What Bernard is hoping to avoid during this pandemic are the painful choices he faced as a young doctor because of a lack of oxygen. After medical school he was posted to a rural hospital, where many of the patients were children battling pneumonia who needed oxygen for treatment. But Bernard soon learned that there was never enough oxygen available. He and the other hospital staff often had to share a single cylinder of oxygen between patients. When there were too many patients and not enough oxygen, he and other doctors would be forced to decide which children would receive oxygen and live, and which would go without it and sometimes die—a choice that broke his heart, he says.
That experience inspired Bernard to investigate the source of Kenya’s oxygen supply shortages. He discovered that one of the biggest challenges is that oxygen is expensive in Africa. In Kenya, oxygen costs about 13 times more than what it does in the United States. The high cost was driven, in part, by a lack of competition. In many countries, including Kenya, there was just a single oxygen supplier for the entire country. And with many health facilities located hundreds of miles away from the oxygen plants, transportation costs drove up prices even higher. The long distances and poor roads also meant that deliveries were unreliable. Hospitals and clinics would regularly run out of oxygen supplies.
In 2014, Bernard founded a public-private partnership to try a new approach that would make access to medical oxygen more affordable and reliable. He named the organization Hewatele (Swahili for “abundant air”). Given the delivery challenges in Kenya, Bernard decided to build oxygen plants at several of the busiest hospitals in the country, where demand is highest and reliable electricity for production is available. The oxygen is then sent out for delivery using a milkman model, with oxygen cylinders regularly dropped off at remote hospitals and clinics and the empty cylinders returned to be refilled. This system ensures that there is always more than enough oxygen available at each facility. Using this new approach, Hewatele has cut the market price for oxygen in Kenya by 50 percent. Now, Bernard is working to expand the number of oxygen plants in Kenya and bring Hewatele’s business model to other parts of Africa.
While the COVID-19 pandemic has brought much needed attention to the oxygen gap in Africa, more needs to be done to ensure that everyone has access to this simple medical intervention. Thanks to Bernard’s efforts, progress is being made. His work has already helped save the lives of thousands of children and adults and will save many more in the future—one breath at a time.