Heroes
Recovering Rwanda
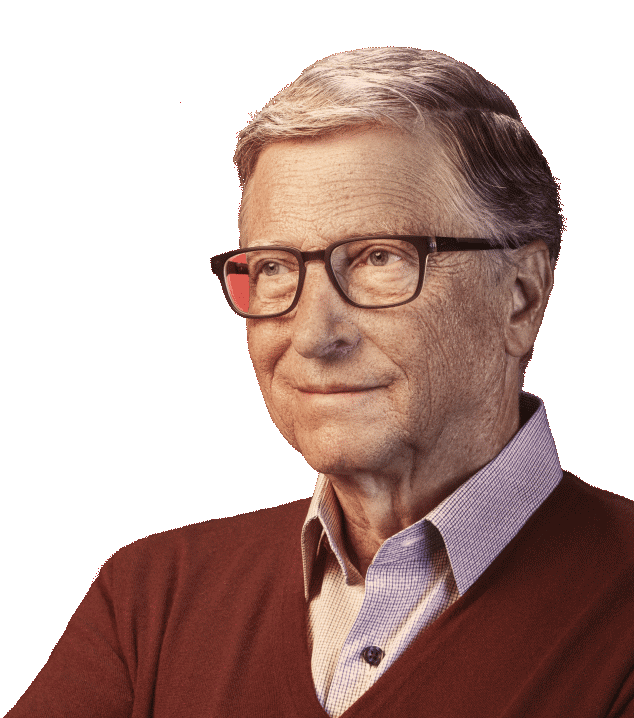
Dr. Agnes Binagwaho helped turn Rwanda into a global health success story.

In 1994, Rwanda was torn apart by a brutal genocide that killed nearly one million people. Its economy and health system were in ruins. Many of the country’s doctors and health workers had been killed or fled. Fewer than one in four children were vaccinated. A cholera epidemic swept through refugee camps. It had the world’s highest child mortality rate and the shortest life expectancy. Rwanda’s future appeared bleak.
Today, Rwanda is a stunning global health success story—one I often cite when I’m asked about examples of health and development progress. More than 97 percent of infants are vaccinated. Rates of child mortality, maternal mortality, and deaths from tuberculosis, AIDS, and malaria have all plummeted. Its health system has become a model for other nations to follow.
Many people were involved in making this dramatic turnaround possible—from government leaders to health workers to the people of Rwanda themselves. Even today, Rwanda hasn’t let up; the country is determined to build on its gains. But the story of Dr. Agnes Binagwaho is a great illustration of what it took to make this transformation possible.
As a physician, leader of Rwanda’s HIV program, and later minister of health until 2016, Dr. Binagwaho has spent the last two decades playing a hands-on role in helping to rebuild the country’s health care system.
Born in Rwanda but raised in Europe, she moved back to Rwanda after the genocide to help with the reconstruction. At the time, Rwanda’s health system had so few resources that when Dr. Binagwaho would return from trips abroad she would fill her suitcases with medical supplies to help care for her patients.
The transformation of Rwanda’s health system has its roots in a very simple, but powerful idea promoted by the government of Rwanda. It’s the belief that health is a human right for all—no matter their income, ethnic group, or where they call home.
“The lesson of the post-genocide period for Rwanda—and for countries around the world hoping for recovery from social upheaval of many kinds—is that a nation’s most precious resource is its people,” Dr. Binagwaho wrote in a Lancet article documenting Rwanda’s recovery while she was minister of health.
To reach the poorest families, Rwanda trained thousands of community health workers who travel from home to home providing care. The government built rural health posts to expand access to medicines and health services. They also launched a nationwide health insurance program. At the heart of the government health care program is establishing trust between the government and the communities they serve. The health workers, for instance, were selected by the villages they served, so the people could decide who would care for them.
While much more work needs to be done to continue to strengthen health care, Rwanda’s progress has been remarkable. That the country’s health system has managed to achieve so much progress on a limited budget compared to other poor countries is often called a “miracle.”
Dr. Binagwaho is quick to correct that misconception and steer credit to the country’s people. “It’s everything except a miracle. It’s the hard work of thousands of health professionals,” she says. “Everything that Rwanda has done is one way or another replicable.”
Sharing what Rwanda has learned about health care is the goal of Dr. Binagwaho’s new career in academia. After leaving the ministry of health in 2016, she was appointed vice-chancellor of the University of Global Health Equity, a university dedicated to educating health care professionals about how to improve health care among the world’s poorest people.
Founded in 2015 by the nonprofit health care organization, Partners in Health, and funded in part by our foundation, the university seeks to radically change the way health care is delivered around the world. The new approach focuses on training a new generation of health care professionals to provide more equitable health services and meeting the world’s most pressing health challenges—including containing diseases like Ebola and designing and running better health care systems.
Currently based in Kigali, the university is building a new campus in the rural community of Butaro in northern Rwanda. The remote setting will allow students to experience first-hand how Rwanda’s effective system of health care delivery is improving the lives of the poor. I look forward to the impact the university’s graduates will have on the future of global health as they help share the lessons of Rwanda’s success with the rest of the world.