Longer lives, better living
Why I’m digging deep into Alzheimer’s
More and more people are getting Alzheimer’s disease. What will it take to find a breakthrough?

In every part of the world, people are living longer than they used to. Thanks to scientific advancements, fewer people die young from heart disease, cancer, and infectious diseases. It’s no longer unusual for a person to live well into their 80s and beyond. My dad will celebrate his 92nd birthday in a couple weeks, a milestone that was practically unimaginable when he was born.
This fact—that people are living longer than ever before—should always be a wonderful thing. But what happens when it’s not?
The longer you live, the more likely you are to develop a chronic condition. Your risk of getting arthritis, Parkinson’s, or another non-infectious disease that diminishes your quality of life increases with each year. But of all the disorders that plague us late in life, one stands out as a particularly big threat to society: Alzheimer’s disease.
You have a nearly 50 percent chance of developing the disease if you live into your mid-80s. In the United States, it is the only cause of death in the top 10 without any meaningful treatments that becomes more prevalent each year. That trend will likely continue as baby boomers age, which means that more families will watch their loved ones suffer from cognitive decline and slowly disappear. Despite this growing burden, scientists have yet to figure out what exactly causes Alzheimer’s or how to stop the disease from destroying the brain.
I first became interested in Alzheimer’s because of its costs—both emotional and economic—to families and healthcare systems. The financial burden of the disease is much easier to quantify. A person with Alzheimer’s or another form of dementia spends five times more every year out-of-pocket on healthcare than a senior without a neurodegenerative condition. Unlike those with many chronic diseases, people with Alzheimer’s incur long-term care costs as well as direct medical expenses. If you get the disease in your 60s or 70s, you might require expensive care for decades.
These costs represent one of the fastest growing burdens on healthcare systems in developed countries. According to the Alzheimer’s Association, Americans will spend $259 billion caring for those with Alzheimer’s and other dementias in 2017. Absent a major breakthrough, expenditures will continue to squeeze healthcare budgets in the years and decades to come. This is something that governments all over the world need to be thinking about, including in low- and middle-income countries where life expectancies are catching up to the global average and the number of people with dementia is on the rise.
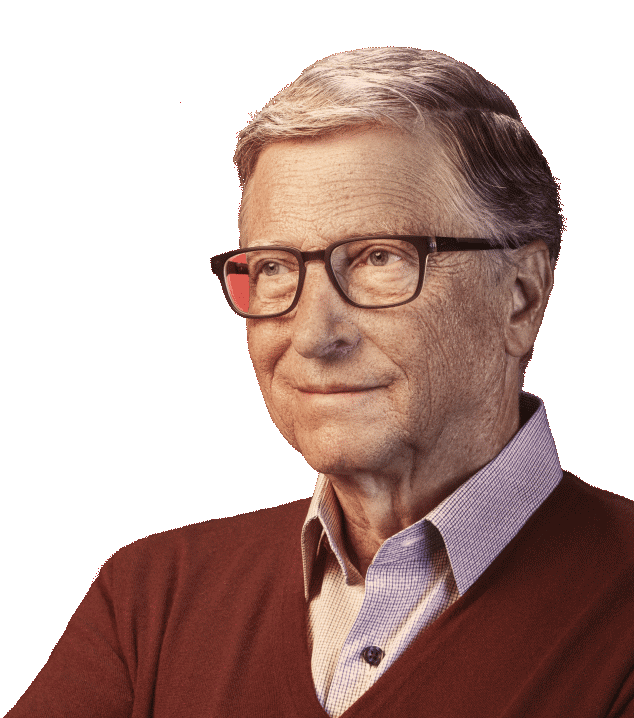
The human cost of Alzheimer’s is much more difficult to put into numbers. It’s a terrible disease that devastates both those who have it and their loved ones. This is something I know a lot about, because men in my family have suffered from Alzheimer’s. I know how awful it is to watch people you love struggle as the disease robs them of their mental capacity, and there is nothing you can do about it. It feels a lot like you’re experiencing a gradual death of the person that you knew.
My family history isn’t the sole reason behind my interest in Alzheimer’s. But my personal experience has exposed me to how hopeless it feels when you or a loved one gets the disease. We’ve seen scientific innovation turn once-guaranteed killers like HIV into chronic illnesses that can be held in check with medication. I believe we can do the same (or better) with Alzheimer’s.
I’ve spent considerable time over the last year learning about the disease and the progress made to date. There’s a lot of amazing work being done in this field to delay Alzheimer’s and reduce its cognitive impact. What I’ve heard from researchers, academics, funders, and industry experts makes me hopeful that we can substantially alter the course of Alzheimer’s if we make progress in five areas:
- We need to better understand how Alzheimer’s unfolds. The brain is a complicated organ. Because it’s so difficult to study while patients are alive, we know very little about how it ages normally and how Alzheimer’s disrupts that process. Our understanding of what happens in the brain is based largely on autopsies, which show only the late stages of the disease and don’t explain many of its lingering mysteries. For example, we don’t fully understand why you are more likely to get Alzheimer’s if you’re African American or Latino than if you’re white. If we’re going to make progress, we need a better grasp on its underlying causes and biology.
- We need to detect and diagnose Alzheimer’s earlier. Since the only way to diagnose Alzheimer’s definitively is through an autopsy after death, it’s difficult to identify the disease definitively early in its progression. Cognitive tests exist but often have a high variance. If you didn’t sleep well the night before, that might skew your results. A more reliable, affordable, and accessible diagnostic—such as a blood test—would make it easier to see how Alzheimer’s progresses and track how effective new drugs are.
- We need more approaches to stopping the disease. There are many ways an Alzheimer’s drug might help prevent or slow down the disease. Most drug trials to date have targeted amyloid and tau, two proteins that cause plaques and tangles in the brain. I hope those approaches succeed, but we need to back scientists with different, less mainstream ideas in case they don’t. A more diverse drug pipeline increases our odds of discovering a breakthrough.
- We need to make it easier to get people enrolled in clinical trials. The pace of innovation is partly determined by how quickly we can do clinical trials. Since we don’t yet have a good understanding of the disease or a reliable diagnostic, it’s difficult to find qualified people early enough in the disease’s progression willing to participate. It can sometimes take years to enroll enough patients. If we could develop a process to pre-qualify participants and create efficient registries, we could start new trials more quickly.
- We need to use data better. Every time a pharmaceutical company or a research lab does a study, they gather lots of information. We should compile this data in a common form, so that we get a better sense of how the disease progresses, how that progression is determined by gender and age, and how genetics determines your likelihood of getting Alzheimer’s. This would make it easier for researchers to look for patterns and identify new pathways for treatment.
By improving in each of these areas, I think we can develop an intervention that drastically reduces the impact of Alzheimer’s. There are plenty of reasons to be optimistic about our chances: our understanding of the brain and the disease is advancing a great deal. We’re already making progress—but we need to do more.
I want to support the brilliant minds doing this work. As a first step, I’ve invested $50 million in the Dementia Discovery Fund—a private fund working to diversify the clinical pipeline and identify new targets for treatment. Most of the major pharmaceutical companies continue to pursue the amyloid and tau pathways. DDF complements their work by supporting startups as they explore less mainstream approaches to treating dementia.
I’m making this investment on my own, not through the foundation. The first Alzheimer’s treatments might not come to fruition for another decade or more, and they will be very expensive at first. Once that day comes, our foundation might look at how we can expand access in poor countries.
But before we can even begin to think about how we do that, we need lots of scientific breakthroughs. With all of the new tools and theories in development, I believe we are at a turning point in Alzheimer’s R&D. Now is the right time to accelerate that progress before the major costs hit countries that can’t afford high priced therapies and where exposure to the kind of budget implications of an Alzheimer’s epidemic could bankrupt health systems.
This is a frontier where we can dramatically improve human life. It’s a miracle that people are living so much longer, but longer life expectancies alone are not enough. People should be able to enjoy their later years—and we need a breakthrough in Alzheimer’s to fulfill that. I’m excited to join the fight and can’t wait to see what happens next.